|
Dr Tom Cromarty Editor Interests: Paediatric Emergency Medicine, Medical Engagement and Leadership, Simulation, Quality Improvement, Research Twitter: @Tomcromarty |
Welsh Research and Education Network
WREN BlogHot topics in research and medical education, in Wales and beyond
Dr Celyn Kenny Editor Interests: Neonates, Neurodevelopment, Sepsis, Media and Broadcasting Twitter: @Celynkenny |
32nd Annual Symposium: Cystic Fibrosis in Children and Adults Royal Society of Medicine, London1/12/2018 20th November 2018 Dr Chris Course The 32nd Annual Symposium for Cystic Fibrosis in Adults and Children took place at the Royal Society of Medicine in London on 20th November 2018. It had been organised by Professor Iolo Doull from the Department of Paediatric Respiratory Medicine and Cystic Fibrosis at the Children’s Hospital for Wales, Cardiff, and aimed to serve as an update for hot topics and emerging trends in the care of cystic fibrosis over the past 12 months. This was my second visit to the Royal Society of Medicine, and again it didn’t disappoint. It is a great venue for any meeting, and always provides excellent conference facilities and service. The RSM put on a great variety of meetings, and there is generally something for everyone, no matter what your area of clinical interest. Many of the meetings are either free or very reasonably priced.
The 32nd Symposium for CF started with a talk from Dr N ick Simmonds from the Royal Brompton about some of the diagnostic challenges emerging in the world of CF. With increasing understanding of CFTR gene variations and mutations, there is an increasing awareness of variable clinical phenotype and disease penetrance. There appears to be an increasing acceptance of a range of CF-related disease, and single-organ disease (e.g. pancreatic dysfunction with normal respiratory health) is being seen in some of the more variable genotypes in some patients. The importance of clinical correlation with genotype was highlighted, as well as the importance of functional assessment of CFTR in diagnostics. The traditional importance of sweat chloride was stressed, and a discussion was had around the emerging use of nasal potential difference calculations in functional assessment of CFTR was discussed. This was followed by a presentation from Dr Julian Forton, Consultant in Paediatric Respiratory Medicine, Cardiff on how best to diagnose respiratory infection in children. This focussed on the successful completion of the CF-SpIT trial, led by Dr Forton (and paper available here: https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(18)30171-1/fulltext) which found that induced sputum samples were as effective as two-lobe broncheo-alveolar lavage samples (currently the gold standard test) at assessing the pathogens present in the lower airways, but were easier to obtain and better tolerated, avoiding need for general anaesthetic. There was also a suggestion that induced sputum may be superior at assessing the bacteria present in the larger airways, which can be symptomatic in children with signs of bronchitis (wet cough). The paper is a really good read, published in the Lancet, and great to see such influential research being undertaken locally in Wales. After speaking with Dr Forton, the findings of CF-SpIT are starting to change practice internationally, especially in Australia, where routine bronchoscopy (not just for symptomatic children) is a much more common undertaking. The morning was rounded off with presentations from Dr Kris de Boeck, Leuven University, Belgium on the challenges on investigating the clinical efficacy of newer disease modulating CF drugs (such as Ivacaftor) in children with rare genotypes, and Professor Martin Walshaw who chaired the NICE CF guideline (https://www.nice.org.uk/guidance/ng78). This provided an interesting contrast between the emerging advice on the challenges of investigating the treatment of rare genotypes with newer therapies, and the role of well-established management in cystic fibrosis and how to recommend best practice in a dynamic and changing treatment landscape. Following lunch, there was a discussion from Professor Andrew Jones of the Manchester Adult CF centre on the complexities of which pathogens we should worry about (in short, we all still worry about pseudomonas, but with newer culture techniques, there are isolates emerging, such as achromobacter, ralstonia, and anaerobes which may or may not be associated with accelerated decline in lung function) and the challenges of extrapolating in vitro models in in vivo clinical situations. This was followed by a presentation from Professor Jane Davies, Royal Brompton Hospital, on the new and emerging therapies in CF. The future at present seems to be the CF modulating drugs, such as Ivacaftor, which improve the function of dysfunctional CFTR, and the potential for combination therapies which improve CFTR production and expression. The main challenges with these drugs still seem to be their immense cost, and correlating this with affordable clinical benefit. The ongoing story of gene therapies was also briefly touched upon, and although initial trials and mechanisms have had suboptimal results, newer trials and modalities are being developed and funded. After a coffee break, the fellow presentations began. This was an opportunity for fellows and trainees to present interesting cases and discussion points to the meeting (and where I had the opportunity to discuss a case and the potential ethical implications for newborn screening). Despite the excellent calibre of the presentations that had come before, and their high academic rigour, the audience were kind and supportive for the trainee presentations, and I wasn’t faced with any overly challenging questions! In summary, the 32nd Annual CF Symposium was a thoroughly enjoyable meeting, and relevant to anyone with an interest in respiratory health in paediatrics. It also provided a useful insight into the transition for these children into adult services and how the focus of management can change with the move to adult CF teams. It was also a valuable opportunity to undertake a bit of CV building with a case presentation (at present anyone who presents at the CF symposium is also invited to submit a review article on the subject for Paediatric Respiratory Reviews). Professor Doull is organising the 33rd Symposium in 2019 also, so keep a look out on the RSM website for further details.
2 Comments
Dr Annabel Greenwood  Earlier this month I attended the Wales Neonatal Network Audit & QI Day and a hot topic for discussion was sepsis and the use of antibiotics. The sepsis risk calculator (SRC) is a fairly new concept due for implementation in neonatal units across Wales early next year…but what does it involve?! What is the sepsis risk calculator? The SRC was established by the Kaiser Permanente Health Group in Northern California, and has reduced antibiotic use in babies by almost 50%. It is a tool for calculating the risk of early-onset neonatal sepsis (EONS) in babies ³ 34/40 gestation. It uses maternal risk factors together with the clinical presentation of the baby to calculate a probability of EONS per 1000 babies. Why is it important? The incidence of EONS is 0.5-0.9/1000 live births in babies ³34/40 gestation, with a 3.5% incidence of mortality. Current guidelines for EONS are not sensitive or specific e.g. the definition of chorioamnionitis can vary, diagnostic tests have poor predictive value for EONS, and 40-50% of cases are not captured by current screening tools. Furthermore, current guidelines do not take into account the clinical examination of the baby. We have a duty as clinicians to improve antibiotic stewardship, avoid unnecessary investigations, and shorten duration of stay in hospital. The calculator in more detail… An initial probability of EONS is calculated based on the population incidence together with risk factors for sepsis including; gestational age, highest maternal antepartum temperature, GBS carriage status, duration of rupture of membranes, and the nature and timing of intrapartum antibiotic administration. The baseline risk is then modified based on the infant’s clinical examination Implementation of the Sepsis Risk Calculator… The calculator is not currently in use in neonatal units across Wales. However, following extensive discussion at the Wales Neonatal Network Audit & QI day, the provisional aim is for implementation early next year. It has already been implemented in some neonatal units across England (Plymouth, Exeter, Bath, Southampton, Oxford), with a reported 40-70% reduction in antibiotic use (depending on the centre So…what do you think? On reflection, after listening to the discussions at the Wales Neonatal Network Audit & QI day and exploring the topic further, I feel the implementation of a sepsis risk calculator on the neonatal and postnatal units is a positive move towards improving our antibiotic stewardship, protecting babies against unnecessary investigations, whilst at the same time easing the workload of the medical team by reducing unnecessary procedures. However, let’s not forget that neither the SRC or current guidelines will pick up unwell babies at birth…There is of course no substitute for clinical acumen!
30th October 2018, RCPCH London Dr Chris Course The RCPCH and the NIHR (National Institute for Health Research) held annual joint study day aimed at promoting and de-mystifying academic training careers. This free study day is fairly new on the RCPCH events calendar, having only been held for the past couple of years, but aims to tackle an area of training which is sometimes perceived as difficult to understand and undertake.
This was my first trip to RCPCH HQ in London, and it was great to actually see the place where its all run from. Despite not being as grand as the Royal College of Surgeons or GPs, it was a modern building with good meeting facilities. I was also a little worried that, not already been on an academic training pathway, I may be a little “out-of-it” or some of the subject matter may not be useful or attainable for me. Thankfully, I was wrong! There was a really good mix of trainees in attendance with a wide range of backgrounds. Some were already undertaking PhDs, some were nearing the end of their training and looking to build a research career, some were already on an academic training fellowship. Meeting all these colleagues with different backgrounds in the “Networking” session during the morning helped me to put my own current aspirations and difficulties into context and to being finding some solutions to these problems. The speakers for the day were an eminent bunch and gave some really useful and insightful talks. Professor Anne Greenough started the day with a broad introduction to academic career paths, and how the new progress curriculum is building research and academia into the training domains, aiming to improve our exposure to clinical research, as well as encouraging the Deaneries to facilitate more academic opportunities. Dr Chris Gale then gave his personal experience of his path into an academic career, giving a “how-to” guide too framing a research question, finding the supervisors and mentors to help develop your project and then how to find the grant money. It was encouraging to hear how perseverance is the key to obtaining the funding, and giving hope that somebody wold fund your project if you’ve had a good idea! The morning was rounded off by Professor Paul Dimitri trying to de-mystify the NIHR – not an easy task! It seems to be a very complex structure, and I can’t say I understand how they work completely, but I’ve definitely got a better idea of where to find more information now. There was also good formation on how to further an academic career as a trainee and consultant after completing your initial projects. The afternoon included workshops from Dr Lauren Kier from the Wellcome trust, covering tips on grant application writing and how to secure that all-important funding, and balancing clinical and academic priorities through your training grades. Following this, there was a presentation covering developing a career in industry, and leaving clinical medicine. I can’t say this talk filled me with inspiration, but it was a interesting to hear the experiences of life outside of clinical medicine with a medical degree. The day was a rounded off with an entertaining talk from Professor Mike Levin, giving an overview of “A journey into research with no plan”, and how an inquisitive mind and a bit of serendipity can help forge an academic career. I’m not sure if the much more structured and formalised training career we have now, with portfolio and ARCP demands, would still allow such a career path, but it was interesting all the same. I would recommend the Academic Trainees Day to anyone contemplating an academic training path or thinking about taking time out of training to do research. Also highlighted in the day was the RCPCH’s Academic Toolkit www.academictoolkit.org which is another useful resource for anyone wanting to know more about academic careers. The day highlighted the challenges and obstacles to an academic career, and how to start overcoming them, and was a good networking opportunity to learn of other peoples experiences. The day showed that an academic career can be a challenging one to start and maintain, but can be incredibly rewarding. Dr Rebecca Broomfield A summary of a year taken out of program to pursue an interest in clinical leadership.  During the last year I have spent my time as a Welsh Clinical Leadership Fellow. While we want to use this blog to promote research and education we also want to highlight opportunities that we have within Wales for trainees. The year as a Leadership Fellow was one of the hardest but most enjoyable of my career. I have blogged on here individually about some of the fantastic opportunities which I was able to attend. I encourage you to look up the posts on the Faculty of Medical Leadership and Management Leaders in Healthcare conference and the blog on the Neuroscience of Leadership course at MIT to name a few. In this summary post I want to give you an overview of why I think clinical leadership is so important and what this year involved Why do it? Is it even important? Leadership is everyone’s business. As you go through your career you will be but into leadership positions even if you don’t think that you are. Everybody within medicine is a leader in some way and therefore surely it is important to learn the skills to be a good one? We teach other things, procedures, history taking, interpretation of investigations so why not teach leadership? I believe there is some weight in the argument that leaders are born, not made in that some people will naturally gravitate to and thrive in leadership positions. But every leader can improve, and therefore good leadership can be taught. If as trainees we are given an opportunity to learn these skills then this can only be a good thing for the future of health care. The Faculty of Medical Leadership and Management Trainee steering group is a fantastic resource for trainees. (https://www.fmlm.ac.uk/about-us/networks-and-groups/trainee-steering-group). They have just published a toolkit which outlines the importance of clinical leadership more eloquently than I can summate in this paragraph. It offers hints and tips to expand your own leadership styles without having to take a year out like I did. This can be found here: https://www.fmlm.ac.uk/members/resources/leading-as-a-junior-doctor The Project When I started this year, I anticipated that the patient improvement project which I had selected to do would be the complete focus of my attention but actually this was a very small part of the lasting impression I have from this year. My project was based within the medical education department at Cardiff and Vale Health Board. I worked with the simulation team changing the way which we collected feedback from our simulation courses, helping with the development of a new simulation suite, designing and leading new simulation courses and co-ordinating a innovative in-situ simulation program to tackle falls. My supervisor Dr John Dunne was fantastic, alongside Miss Melanie Cotter they gave me freedom which I have not had in a structured training program to pursue my own interests and develop my project as we went along. Because of this I probably worked harder than I ever have, but also enjoyed work more than I ever did. My project actually became more of a tool in which to try out different leadership styles and the hints and tips we were learning as part of the PGCert in Leadership and management. It was successful and will leave a sustainable change within the medical education department. As fellows we were all encouraged to take steps to select a project that was outside our comfort zone. While I did have a previous interest in medical education and simulation I am a paediatrican and a lot of my work this year has been done within adult specialities. The projects which we had very varied and extremely different but all offered the same opportunities and similar enough experiences. The PGCert This is the qualification which runs throughout the Leadership Fellow year. It is run by Academi Wales through Trinity St David University. The course gives you a qualification at the end of the year and is a big difference in Wales when compared to the clinical leadership opportunities offered in England, Scotland and Northern Ireland. There were structured sessions spaced throughout the year which were attended by a wide variety of participants outside the fellowship program (clinical directors, speech and language directors and dentistry leaders to mention a few.) These focused on a variety of different areas within clinical leadership. Teaching different leadership styles, exploring coaching qualifications and self reflection with tools such as Myers-Briggs. The best session was the team building session in Elan Valley – again on this site there is a blog post dedicated to this experience. As a tip to this years Welsh Clinical Leadership Fellows – write your project up before you go back to clinical rotations! Right now, when I’m writing the essays, I wish I’d followed this advise from the year before me 😊 The Good I have been able to develop myself more in this year than in the whole of training so far. I have had the opportunity to analyse my behaviour looking at my preferences, understand when they might not be the best option and how to make them work for me. I have been taught the tools to look at difficult situations from different perspectives and recognise that not everybody thinks like me! – This in itself seems simple, obviously not everybody thinks the same but I was really able to explore just how different other peoples viewpoints were. By being able to see and appreciate these, not necessarily agree, you can avoid a great deal of conflict and confusion. Resulting in, as well as from, poor leadership. But I was also taught how to deal with conflict, how to turn challenge and opposition into a unifying aspect rather than a dividing one. I have learnt to ask for forgiveness, not permission and have been given the confidence to express my opinion. I have explored my own personality and learnt to look after myself. I hope to work in the emergency department and these skills will be invaluable as I go through my career to increase my emotional intelligence and resilience. The Bad It was HARD work. The first few months finding your feet and trying to work out what direction you wanted your project to go in were really difficult. As trainees we come from very structured environments, rotating from job to job, thinking in 6 month blocks and ticking off targets to pass the ARCP. This year was different, at the start there were no targets, you had to make and develop them yourself. You had to become used to managing your own diary. Not having to clock in and clock out was very liberating but also intense. As a group we handled this either by working every hour never really clocking off, in order to justify our time or by spending a while drifting around not really achieving much with he vast amount of time offered to us. This evened out in the end as we learnt the skills which came with the freedom. It was your responsibility to create opportunities rather than somebody handing them to you. And networking is a skill which can only be achieved through practise and comes easier to some than others. On a personal note, I was also away for large chucks of time from my family home. I have 2 small children aged 5 and 3 and part of this year was to have the flexibility to see them more frequently. I’m not sure I achieved that, being on a plane to Boston while my daughter was on stage at St David’s Hall in her first ballet show was a particular low point. (Thanks go to my Mum for stepping into that!) In Summary The pros far outweigh the cons. I have learnt so much more about who I am. What is good about my leadership style but also what I need to work on. My biggest learning point from this year is to respond not react, something that I didn’t even recognise I was doing until this year. I have had the opportunity to develop a long lasting quality improvement project, which is sustainable even after I have left my post. But I worked hard, I created my own opportunities and spent less time with my family than I would have liked. But ….. Would I do it all again? … Absolutely! If you are interested in applying for the Welsh Clinical Leadership Year and want me information please do contact me, I’d be more than happy to chat over coffee.
Guest Blog from Dr Katie Greenwood ST8 Hello! Thank you WREN team for giving me the opportunity to share my experiences over the past few years with you. Life as a paediatric trainee can be one of considerable stimulation, compassion, challenge and significant reward. The desire to deliver a very high standard of performance and achieve excellence within the workplace, has made me recognise the importance of developing exciting out of hours interests and achievements. Alongside working hard as a senior paediatric trainee, I have developed a passion for competing in triathlons and have participated in a number of challenging races across the world. Where did it all begin?......… A friend mentioned joining the Cardiff Triathlon club, apparently the fastest growing club within the UK. I pondered the idea of joining the team. Here are a few initial thoughts which crossed my mind: - How on earth do people manage to swim/cycle/run within one race? - Open water swimming in the UK sounded particularly un-exotic! - How does a busy paediatric trainee fit in the training for this challenging sport? After joining the club I started my racing career with a low key Cardiff “try-a-tri” triathlon and finished the same season with a race in the French alps….the famous (and brutal!) Alpe D’huez mountain climb. Oh dear! From these moments on, I haven’t looked back! Over the past few years I have been fortunate enough to win both the Sprint and Standard distance Welsh Champion triathlon titles. I have also been selected to compete for Great Britain (‘GB Age group Team’) at the 2017 World Triathlon Championships in Rotterdam and European Championships 2018 & 2017 in Estonia and Dusseldorf Germany. I was absolutely delighted to represent team GB and finish in the top 10 in each race. So what does all this involve?
I would encourage everyone to enjoy a hobby outside of work and if you are interested come and join the triathlon club. Immense enjoyment can be experienced at every level and it is a fantastic way to meet new people and keep fit ready for the workplace!
Dr Chris Course The European Respiratory Society held their annual Congress for 2018 in Porte de Versailles conference centre, Paris. The European Respiratory Society is a non-profit organisation which aims to promote lung health and drive standards for respiratory medicine globally. In addition to publishing the European Respiratory Journal and educational handbooks, the annual congress is the largest respiratory conference in the world, covering topics on respiratory health and disease from fetal life to old age. Having registered months ago, (with an excellent discount on the registration fee for the honour of being under 40!) the congress program arrived in my inbox a few weeks ago, and to say it was overwhelming was an understatement. There were numerous concurrent sessions, across three floors of the conference venue, with special seminars and workshops on topics from non-invasive ventilation in adults, to bronchoscopy, lung ultrasound and inhalers for COPD. Having a paediatric/neonatal interest made it much simpler, as once you had filtered out all of the adult program, there was a manageable range of choices! The whole conference ran across four to five days, with the majority of the paediatric program running across the middle three days. The quality of presentations was high, and the speakers were clearly eminent in their field. Despite being a “European” conference there were speakers from across the world. I had gone with Professor Sailesh Kotecha and members of the research team at the School of Child Health, Cardiff University, and Professor Iolo Doull from the Paediatric Respiratory Medicine team in Cardiff. The first day we attended sessions on Prematurity and Lung Disease which included work presented by David Gallacher (Neonatal GRID trainee, Wales) from work he conducted with the School of Child Health at Cardiff University looking at pro-inflammatory cascades in the Preterm lung. Presentations also included work on Ureaplasma treatment for Preterms, animal models looking at effects of different durations of mechanical ventilation on long term alveolar structure and the Forced Oscillatory Technique for real-time assessment of preterm baby’s lung mechanics. The afternoon had an excellent Paediatrics Year in Review session looking at the top literature from the last year, the highlight of which was Dr Ian Balfour-Lynn (Royal Brompton, London) presenting the last year’s work on Cystic Fibrosis disease modifying drugs like Ivacaftor and Orkambi. The second day started with the Paediatric Grand Round where challenging cases and unusual diagnoses were presented and discussed, and this brought a good contrast to some of the talks from the first day on mechanistic and translational science. This as followed later in the day with a Lungs on Fire session where quick fire case presentations and questions were put to a panel of experts and the audience with the opportunity for us to vote along – this gave me confidence that some timers no-one knows what the right answer should be! Another session looked at the infectious causes of wheeze and asthma and our current knowledge in their manipulation. Talks included work on the microbiome of the upper airways, and our current evidence base for the treatment of pre-school wheeze, and it looks like Montelukast is out again! A running theme across the first two days was the quantity of work looking at azithromycin for the treatment of a range of conditions, and although lots of the evidence was convincing, I was occasionally left wondering if it’s the current fashionable treatment or a drug with further unexplored potential. The second day ended with the paediatric dinner, which started with a boat trip down the Seine, followed by dinner at the foot of the Eiffel Tower. This was a great evening and opportunity to escape the conference venue. As much as I enjoy a good conference, the inside of a presentation hall is pretty much the same wherever you are, and it was nice to get out and see a little of the City of Lights. Dinner was interesting (the starter consisted of a mixture of tuna steak and strawberries…) but so was the opportunity to meet new people from across Europe and the world. The last day (slightly tired!) we got in nice and early, mainly because our posters had to go up! After a coffee and a croissant, we headed to the first session on Prenatal Origins of Respiratory and Atopic Disorders which included data from the COPSAC (Copenhagen birth cohort) studies and animal models looking at how maternal smoking, and interestingly “vaping” may affect offspring into adult life. It also highlighted the scientific, economic and clinical difficulties in managing such large birth cohort studies and how replicating results can be challenging. Following this, we attended a session on Advances in Primary Ciliary Dyskinesia. This covered pathophysiology of this rare and little understood disease and highlighted how genetic are changing diagnosis. However, it was rightly pointed out after the presentations that, much as with Cystic Fibrosis, the phenotypic variance of these genotypes is still not clearly understood, and the continuing importance of expert interpretation of histological samples and formation of centres of excellence to manage this condition. We ended the ERS by having a walk through the exhibitors hall. There was a great ‘Game Zone’ where we could play with video laryngoscopes, bronchoscope and thoracic ultrasounds and it was great to have a go with bits of kits that we’d seen or heard about but had little experience with. Tutors were on hand thankfully to guide us through the finer details! We also had a look through the commercial and pharmaceutical exhibition areas, which looked more like a new car show at times (not sure a hologram is really required to advertise an inhaler) and there was a paucity of the free pens, but there were plenty of places to sit and have a quiet five minutes, which was much needed by this point! Overall, the ERS Congress was a fantastic experience. Definitely the best organised, highest quality, best value meeting I’ve ever been to, and would thoroughly recommend to anyone with a respiratory interest. Next year the congress is heading to Madrid, check out www.ersnet.org for more information
Faculty of Medical Leadership and Management Wales Regional Conference 2018 13th September 2018 Dr Rebecca Broomfield  While I have completed my year as a Welsh Clinical Leadership Fellow (Blog post teaser … more on that in Novembers posts!) I still very much have an interest in leadership and how we can rise to the current challenges facing the National Health Service. Therefore I was excited to learn that the FMLM were hosting a conference just up the road in Cardiff. It was a heavily packed program and the day flew by in a flash. The FMLM Chief Executive Mr Peter Lees spoke to us about the aims and targets of FMLM and how they plan to achieve this. He was followed by Wales' very own Chief Medical Officer Dr Frank Atherton who opened with "If we don't seize the opportunity as medical leaders …. who will?" He emphasised the need for whole system change not jus on an individual level and that as an NHS in Wales we do not simply need more. We need to harness ideas and bring them together. We need to keep patient safety at the centre of everything we do and bring those who resist change with us through the changes which need to occur. Following the CMO is always a tough gig but it was managed superbly by Dr David Samuel (A fellow Leadership Fellow Alumni) and Dr Sian Lewis. They reminded us of the need for diversity in the workplace and within medical leadership teams. They asked us to do a tabletop exercise to emphasise this point. Each member of the team picked a O or a X card. We were not able to tell each other which symbol we were. Then everybody shut their eyes and the X's were instructed to open their eyes and read the instructions. The task was to plan a holiday but to do so without giving any value or time to the O members of your table. Then the O's reopened their eyes and the task of organising a holiday was given to the table. I was an X. It was incredibly difficult to ignore and not give value to peoples suggestions. It felt awkward and non productive to an effective team working environment. The O's felt undervalued, and eventually gave up suggesting things and went off into their own discussion, effectively planning a whole other holiday. The exercise was trivial but raised a good point - are you really inclusive in your leadership? Do you consciously or unconsciously bias against somebody and importantly how does that effect the team. Post a quick coffee stop we heard from Mr Nigel Edwards (Chief executive, Nuffield Trust) about integrated care and Dame Clare Marx (Current Chair of FMLM, former President of the Royal College of Surgeons, soon to be Chair of the GMC and a dynamic powerful woman) She spoke about the importance of clinical leadership and the fact that we need to change. She suggested that we need to exchange hierarchy for connectivity and that clinical leadership can impact to increase quality, social performance and make financial gains. She believes that positivity has a big impact on your team and that we have a responsibility to coach clinical leaders and help people to develop themselves. Following this we had the unique opportunity to have a panel discussion on current leadership challenges and how we can embrace them and continue to move forward within Wales. We asked for their key Leadership message: Dr Frank Atherton - To use management experience from outside of Medicine and promote interdisciplinary working. Dame Clare Marx - The only thing you can control in life is yourself, the way you work and the way you behave. Understand what it is you have the ability to control. Mr Nigel Edwards - Connect what feels real, we are missing a narrative "tell a story" After lunch we were encouraged by Ms Katie Laugharne (Head of Welsh affairs at the GMC) and Dr Madhu Kannan (Current Welsh Clinical Leadership Fellow within the GMC) to think about Leadership expectations and impact. How the things you do day to day have an impact and how small things, like tea!, can really matter. We were encourage to think about how our leadership style was viewed by members of our teams and if that was the way we wanted it to be. After a quick coffee break we learnt from Mr Christian Servini about what the future generations act was enabling people to do in Wales and the impact this was having on Well-being. Then to end the day a quick fire 5 minute presentation round where we heard about improvement projects which were having an impact around Wales. My project (poster below) was one of those presented. If you are at all interested in Clinical Leadership I would encourage you to take a look at the FMLM website and consider going to the annual conference. Leaders in Healthcare details of this can be found here: https://www.fmlm.ac.uk/events/leaders-in-healthcare-2018
Dr Annabel Greenwood ST3 This is the first (hopefully of many!) of a new blog feature entitled ‘a day in the life of….’ Rebecca and I thought the blog would provide an excellent platform to share experiences of various opportunities and achievements, including paediatric speciality medicine posts, and out-of-programme experiences, both academic and non-medicine related, inspiring readers to explore something new to enhance and enrich their paediatric training. It gives me great pleasure to debut this new blog feature by sharing my experiences of paediatric oncology. Having just completed my 6-month ST3 post, there is absolutely no question that I would recommend it to my fellow trainees! I hope by the end of reading this blog some of the misnomers associated with the world of paediatric oncology will have been dispelled. Now, I’ll be completely honest with you…when I was first given ‘paediatric oncology’ as my ST3 rotation, I was a little apprehensive to say the least. My previous exposure to oncology had been only brief encounters during out-of-hours speciality cover, treading water until handover. The complexity of the patients, the mind-field of chemotherapy regimens, and the ‘sick’ potential of the febrile neutropaenia patients is enough to induce a resting tachycardia just thinking about it right?! Let alone managing such situations! Fast forward 6 months, and my feelings as I walk onto the ward each morning couldn’t be further from that overwhelming uncertainty at the outset. And these are just some of the reasons why; 1. Teamwork: The MDT on the paediatric ward is truly wonderful and you feel part of the ‘family’ in no time. The nurses and nurse specialists know everything about their patients and chemotherapy regimens, and are always happy to help, the play specialists have an incredible way of boosting morale and making what can sometimes feel impossible, possible, and the consultants are very ‘hands-on,’ supportive and approachable. I sometimes don’t know where I’d be without the knowledge and advice of the pharmacists, not to mention to the wonderful physios, dieticians, and psychologists. 2. Variety: There is no denying that paediatric oncology is one of the busiest jobs in the hospital. The days can be relentless and sometimes it feels like you spend hours sorting the smallest of tasks, yet it’s often the smallest things that can make the biggest difference to both patients and their families. No two days are the same, from daybed reviews to the ward management of both haematology and oncology inpatients…every day brings new challenges and experiences. 3. Organisational/management skills: New patients often need investigations and procedures sorting quickly, involving liaison with the anaesthetists, surgeons and radiologists. There is a weekly ‘lines list’ to be coordinated for insertion/removal of portacaths/hickmann lines, and there is a weekly ‘planning meeting’ to discuss and arrange patients to be admitted for chemotherapy, investigations or procedures. 4. Practical procedures: There is a small theatre room on the ward for the weekly list of bone marrow aspirates, lumbar punctures and intrathecal chemotherapy. This is primarily led by the consultants and registrars. 5. The management of sick kids: Oncology and haematology patients have the potential to get really sick, quickly. Neutropaenic patients on chemotherapy can become profoundly septic, and sickle cell patients can present in an acute crisis. Coordinating the management of such patients although stressful, is excellent preparation for transitioning to middle grade training. There are protocols for the management of various situations, and as mentioned previously, there is always support provided by the consultant. 6. Emotional aspect: One of my principal anxieties before starting the rotation was how to handle the emotional aspect of the job. Of course, there can be devastating situations where treatment is unsuccessful, however, the kids are incredible, so resilient and courageous, and certainly serve to put things into perspective. Many of the children return to the ward on a regular basis for reviews and chemotherapy, so you really get to know the children and their families, and play a significant part along their treatment ‘journey.’ Of course like most jobs there can be days where there is no spring in my step along the ward, however, the positives far outweigh the negatives, and I am so grateful for the opportunity to experience such a truly wonderful job. If you've done a unique job and want to share your experiences as a blog post then email either Rebecca or Annabel to share different experiences.
‘The Palliative Care Journey: Managing Uncertainty’ Guest blogger Dr Tim Warlow Senior Registrar All Wales Paediatric Palliative Care Network Following the success of last years All Wales Paediatric Palliative Care Network Conference, the team are excited to introduce the much anticipated 2018 conference. This year we will be exploring the palliative care journey from the perspective of the child and family. Hearing from the families themselves, the day will follow their journey from diagnosis through to bereavement. Some of the questions we will be asking include: • When should palliative care be introduced and how do I raise the issue with families? • How do I support families whilst making difficult decisions about their child’s care? • What are the spiritual needs of families at the end of their child’s life? • How do I manage difficult and unfamiliar symptoms at the end of life? • How do I approach uncertainty and grief? • How can Ty Hafan Children’s Hospice help me to provide holistic care to families? When working with families of sick children, many of the most challenging issues we face are also the most rewarding when done well. This day aims to unveil those daunting aspects of care, provide ample opportunity for discussion, and hearing from the expert parents and professionals as to how we can serve our families better. The morning will focus on introducing palliative care and decision making, especially relevant in light of recent high-profile media cases. We will consider how we can involve children better in decisions relating to their care, collaborating with families to ensure they feel listened to and valued whilst navigating legal and ethical uncertainties. Next we will hear from families of children with life limiting conditions themselves. What were the most challenging times, and what actions of professionals were key to their palliative care journey? What was helpful, what was harmful? We will consider how each professional on their journey played a key role in ensuring excellent holistic palliative care and what we can learn from one another. Finally, the afternoon will include a series of breakout groups to provide opportunity to really get stuck in exploring an aspect of the palliative care journey that is a priority for you. There will be time to discuss and ask questions in a smaller group setting. Topics include supporting children and families at the end of life, managing difficult symptoms, supporting grief, bereavement and spiritual care, and how to support staff including debriefing. Last year’s conference was booked up quickly and over 100 delegates had a fantastic day. Now in its fourth year we have built on the lessons of previous years, responded to your feedback, and produced a day which promises to be challenging, rewarding, and a fascinating insight into the lives of our patients and families through their own eyes. Here is some feedback from last year’s conference as a taster of what delegates took away: “Learnt many new things. Was challenged on preconceptions and pre-existing myths of Palliative Care. Enjoyed the professional, but personal element for some speakers / discussions.” “ Excellent day from start to finish, sessions we interesting, informative and thought provoking.” “I was hooked from start to finish” “The case studies/discussion groups with the panel of different professionals involved with the neonate and their families’ journey were excellent and thought provoking. These were great for learning about how processes can work well and can adapt along the way.” We look forward to you joining us in October Key details Date: 18th October 2018
• Location: Park Inn by Radisson Hotel, Cardiff City Centre • Cost: £32 per person (£16 subsidised tickets available for students and upon individual request) • Bookings and information: education@tyhafan.org 9th-10th July 2018 Dr Rebecca Broomfield The Patient Safety Congress aims to transform the UK’s approach to delivering high quality care. It champions patient safety as the organising principle of a healthcare system which is truly efficient, effective and able to offer the best experience to patients and carers. I was lucky to be able to attend the Conference in Manchester in July. Prior to attending I had minimal experience with the Health Service Journal who sponsor the event and although clearly focusing my training and clinical work on optimising patient safety I knew very little about this movement within healthcare. The HSJ run awards and publish a journal purely focusing on and publishing patient safety initiatives and ways which can all make out practice patient focused and as safe as possible. The conference was busy and if I am completely honest the timetable when I first looked at it was completely overwhelming. There was key note lectures which drew the participants together and then 5 streams running throughout the 2 days which you could dip in and out of to cover the sessions which most interested you and met your personal learning needs. Along with an exhibition centre and poster presentations focusing on 9 different topic areas. Unfortunately due to childcare compromises (working parent problems!) I wasn’t able to travel up to Manchester until the Monday morning so missed the opening keynote speakers which I was reliably informed were excellent and predicted the exit of The Right Honourable Jeremy Hunt from his health secretary post, but unfortunately the predicted replacement Dr Kevin Fong turned out to be less accurate! When I arrived I set up shop in the Human Factors stream. The streams for day 1 were: Human factors, Delivering quality improvement on the frontline, Driving a culture of patient safety, Improving patient safety through governance and compliance and finally Bridging the gap: policy and clinical Practice. The human factors stream was chaired by Martin Bromiley OBE (@MartinBromiley) of medical “Just a routine operation” fame https://www.youtube.com/watch?v=JzlvgtPIof4 – if you don’t know who he is or his story as a healthcare professional then you really should so click on the youtube link and learn about it. What is human factors? As defined by NHS England Human Factors for healthcare are: “Enhancing clinical performance through an understanding of the effects of teamwork, tasks, equipment, workspace, culture and organisation on human behaviour and abilities and application of that knowledge in clinical settings”. Essentially it is about Making it easy to do the right thing The stream started well and I very much enjoyed hearing from 3 speakers talking about how they had introduced human factors within their areas or work and outlining the importance of doing do. Dr Shelly Jeffcott (@drjeffcott) spoke first about the importance of human factors and outlined some goals. She emphasised designing the systems so that it is easy to do the right thing and the importance of integrating human factors training in the medical workforce. Education for Scotland have developed an e-learning package on human factors. It is easy to create an account and access this at: https://turasdashboard.nes.nhs.scot//User/PersonalDetails/Create?openIdApplicationId=e8c7cbb9-34fd-4c87-8c6c-7232cf6786d7 Next up in this session was Mr Simon Paterson-Brown (@spbsurgery) he spoke about the use of training within a surgical environment to develop non technical skills. His sessions Non-Technical Skills for Surgeons have international acclaim and have been widely published. Finally the session ended with Professor George Youngson (@ggyrach) whop focused on thE impact of bullying and discrimination in care systems. Bullying is a huge problem in the NHS and this was outlined during this session Professor Youngson identified that it is still a problem and has done work proving its detrimental effect on patient safety. He encouraged us to speak up for safety and ensure that bullying was addressed in our departments. The stream then moved onto the nudge theory and how we can use this within the NHS. Helping people to make the right decision at the right time thus improving patient safety. During this session there was talk about the noble prize winning book “Thinking fast and slow” by Daniel Kahneman looking at the way people make decisions and how the nudge theory exploits this. By understanding how people behave we can design better policies and systems to improve patient safety. The EAST framework was suggested here: Easy, Attractive, Social and Timely. Any change in behaviour should fit into this framework. And where there is variation in practice it offers a good target for change. After lunch I remained in the Human Factors stream and the session delivered by Abbie Coutts and Professor Bryn Baxendale (@gasmanbax) focusing on situational awareness. During this session it was the first time in this conference that I was exposed to a patient story being used to demonstrate a learning point. This is something which was utilised through the conference, across many different streams and had a truly powerful impact. Abbie Coutts presented her father’s case and observations on why errors occurred. She has used the errors in care which happened to her father to teach the health board which cared for him about human factors. She suggests that this should be taught by people doing the job and understand why errors happen in order to address them rather than just how they happened. Professor Bryn Baxendale then spoke about balancing acts and how to embedded key skills and behaviours into practice. Both speakers focused on normalising excellence and doing the simple things well. The fourth session in the human factors stream again used a patient story presented by Kathryn Walton https://www.youtube.com/watch?v=r7gk1AvZKZA We heard from the patient, the healthcare worker and what happened afterwards. I would encourage everybody to follow the link about and listen to the story. This was an exceptionally emotive story and emphasised. The final breakout session I attended was delivered by The GMC within the Driving a culture of patient safety stream who presented a discussion on the GMC survey and understanding this data in relation to patient safety. The keynote to end day one was delivered by Professor Alison Leary (@alisonleary1) and focused on the fact the “Hope is not a plan” and within medicine what we can learn from other safety critical industries. Professor Leary presented an the fact that the very structure of the NHS is significantly different to other safety critical industries in that we place our most junior inexperienced staff at the front line closest to the operational risk, with the experienced workforce behind the scenes. This is in contrast to other industries who use their experienced work force next to the operational risk and use them to allocate selected work to the junior teams. In the NHS we need to be focusing on rewarding frontline experts to stay where they are on the shop floors rather than moving them further and further away into managerial positions. We need to use good policy and education where the expectations are clear and safety is mandated alongside clear credible leadership. Her closing statement was particularly poignant and a quote from Dr Tracy Dillinger NASA “People defer to hope, but when failure is not an option, hope is not a plan” We went out for dinner in Manchester as a group of leadership fellows and I can 100% recommend The Alchemist for cocktails because they are fantastic, and for those based in South Wales one has just opened in Cardiff (yay!). Back to the conference ...! Day 2 Day 2 opened with the prize giving for the poster competition. I entered 2 posters and this one won its category of ‘Education and Training’ Proof that if you do an interesting improvement project then it’s always worth popping it into a conference because you never know how far it might go. The keynotes opened with Dr Bill Kirkup presenting themes which happen when things go wrong and how we should use these to make sure that as organisations we do not get into situations where things go wrong. He identified the follow themes: - Failure to learn He ended with 5 key points for maintaining patient safety: - Listen to the patient, they are telling you the answer - Honesty not reputation management - Investigate and learn – not suppressing bad news and learning from others mistakes - Dismissing and denial leads to a slippery slope which is harder to stop - Do NOT think “It will never happen here” The second keynote was also focused on investigations but from the Healthcare Safety Investigation Branch and what we can learn from the investigations which they have already processed. It is worth reading the summary documents of these investigations as it is different from a root cause analysis which will take place internally. They look at the route cause but also ask “why?” Again day 2 was split into streams. The 6 streams on day 2 were: Collaborating to achieve patient safety, Delivering improvement on the frontline, Using research to solve the big challenges, Prioritising safety for vulnerable people, workforce the crucial ingredient for safety and Bridging the gap: Policy and the clinical practice. I attended Leading from the top: New research on trust level leadership under the using research to solve the big challenges stream. I left this session feeling quite negative. The panel presented learning which they felt had happened since the Frances Report. Which seemed to be, in their opinions, very little. They appeared to feel that this was a continuing problem with variability in quality and consistency of leadership practises. I feel (esp. as a current leadership fellow) that the Wales deanery is actively promoting and encouraging learning about clinical leadership. And I would signpost anybody to the FMLM website if they want more information on clinical leadership. https://www.fmlm.ac.uk/ I then attended the LEDER program, http://www.bristol.ac.uk/sps/leder/, focusing on what needs to change for people with a learning disability in order to ensure their safety, under the Prioritising safety for vulnerable people. Again this focused on a patient story presenting the experience of the family of Oliver McGowan. (@PaulaMc007) They are campaigning for mandatory training for healthcare professional in how to adapt for patient with autism and learning difficulties. They want to work on preventing these stories and raise awareness for people to make reasonable adjustments. They encourage communication, an overriding theme from this year, with the patients, and their families as they know the patient best. Then, before lunch I moved into the Workforce stream to hear from Leigh Kendall (@leighakendall) Again this presentation focused on a patient story presenting Hugo’s story focusing on preventable harm within a maternity setting. Hugo was born after Leigh suffered from HELLP syndrome at 24 week gestation and lived for 35 days. She is working on improving bereavement information and including bereaved families in the quality improvement processes, alongside communication between healthcare professionals. She again encouraged communication and stated something which will stick with me “You can’t upset us anymore because the worst has already happened” Don’t be afraid to speak to bereaved families they can give you vital information and want to have a voice. Mr Edward Morris then presented the work of the Royal College of Obstetricians and Gynaecologists on Each baby counts (@EachBabyCounts) again focusing on patient stories and human factors to encourage a focus on communication and preventing harm. https://www.rcog.org.uk/eachbabycounts After lunch the conference was again brought back together for keynote sessions. The CQC Chief inspector of Hospitals, Professor Ted Baker, presented an evidence based argument for how Inspections can help us with patient safety. He encouraged us to engage and empower frontline staff to really focus on patient safety and put patients at the centre of what we do. He reminded us to “relentlessly focus on leadership and culture” but also to recognise that healthcare is a high risk area and we have to accept the implications of that fact. He believes that with backing the inspection process can be used to drive forward a culture of patient safety. The Right Honourable Jeremy Hunt MP was due to present next in his role of Secretary of State for Health and Social care, but as he had been relocated and Matt Hancock (@MattHancock) had been in the job for less than 24 hours Professor Bruce Keogh and Dr Aidan Fowler from 1000 Lives stepped up to be part of a panel for the next steps for patient safety. The conference closed hearing from a panel about how their organisations overcame safety challenges. The overriding themes were again all about culture, communication and mindset. If you can get this right then you seem to be on the right track! The Patient Safety Congress was a fantastic, engaging conference and if you get a chance to go I really would. The use of patient stories to focus the attendees was a really useful tool and one which I will take forward with other presentations in the future. It was a really important reminder that we do have the opportunity even as trainees to focus on patient safety and improve outcomes. More information can be found in the HSJ journal https://www.hsj.co.uk/ and on the patient safety congress website https://patientsafetycongress.co.uk/
Guest Blogger Dr Jordan Evans N Engl J Med 2018;378:2275-87. DOI: 10.1056/NEJMoa1716816 If there’s one thing we all know about manging diabetic ketoacidosis (DKA), it’s the importance of being extremely cautious with fluid management due to the risk of causing iatrogenic cerebral oedema right?...Wrong! Once again, like John Snow, we unfortunately ‘know nothing!’. When will the childhood lies end, Father Christmas isn’t real, the Easter bunny’s not real and now this, the most painful blow yet. In this PECARN (Pediatric Emergency Care Applied Research Network) study, published in the New England Journal of Medicine, Nathan Kuppermann et al investigated the influence of intravenous fluid administered on the rates of neurological injury in children with DKA. What was the reason for the study? Brain injury occurs in the region of 0.5% - 1% of DKA presentations. It presents with sudden neurological deterioration. Patients without a marked neurological deterioration may have more mild neurological impairments e.g. memory / cognitive impairment. As all of us were likely taught, brain injury in DKA has long been thought to be iatrogenic, secondary to fluid administration causing cerebral oedema due to osmotic gradients. The evidence for this school of thought is however lacking and evidence has emerged actively disputing it. Alternative explanations have been proposed that there may be something about being particularly unwell with DKA that leads to the neurological injury, possibly inflammatory or vascular changes. The more unwell the patient is the more likely they are to require fluid resuscitation and therefore an association between severe DKA with brain injury and fluid administration could be mistaken as causation. Remember that association is not proof of causation! Oedema may develop secondary to the brain injury itself as it does in other mechanisms of injury such as trauma. Where did the study take place? The study was conducted across 13 centres in the United States. Who did they include ? Children aged 0 – 18 years with a diagnosis of DKA (pH < 7.25, glucose > 16.7 mmol/L. Children with GCS <12 were excluded two years into study (due to concerns of treating clinicians). What did the investigators do? Children presenting to study centres with DKA were randomly assigned to one of the following four groups; 1) 0.9% saline fast administration 2) 0.9% saline slow administration 3) 0.45% saline fast administration 4) 0.45% saline slow administration The fast group were given a 20ml/kg bolus which was then followed with replacement of a 10% fluid deficit with the first half of the deficit volume being replaced over 12hrs and the rest over the next 24 hrs. The slow group were given a 10ml/kg bolus which was then followed by replacement volume for a 5% deficit which was given over 48hrs. The primary outcome was a decline in mental status (GCS <15 on two occasions within first 24 hours of treatment. Patients and parents were blinded but not the clinician. Secondary outcomes; clinically apparent brain injury (neurological deterioration leading to clinical decision to treat for raised ICP, intubation or death), short term memory, memory & IQ at 2 months and 6 months. What were the results? 4912 patients met the inclusion criteria. Due to the complexities of the study of these there were a total of 1389 episodes of DKA included in the study (from 1255 different children). There was a fall in GCS in 3.5% of these epsiodes (48 episodes). There was clinically apparent brain injury in 0.9% (12 episodes). There was no difference between the two groups for any of the outcomes. (Some of the raw results favoured the fast fluid administration group although none of these results reached a statistically significant level). Conclusions Kupperman et al. rightly concluded that ‘Neither the rate of administration nor the sodium chloride content of intravenous fluids significantly influenced neurologic outcomes in children with diabetic ketoacidosis’. Take home message for practice in Wales 1. We no longer need to be as anxious about giving fluid too fast in DKA
2. If you need to give a bolus for shock do so without fear of causing cerebral oedema, this study provides evidence that it’s not harmful. 3. With regards to the fluid deficit replacement although this study shows we could safely give it a little faster stick to current practice of the Wales DKA protocol as it doesn’t show any improvement in outcomes for the faster administration of IV fluids. 4. It’s worth remembering that there is good evidence for using 0.9% saline for maintenance IV fluids in children (to prevent hyponatraemia) so it’s not clear why they chose to have arms in this trial with both 0.9% saline and 0.45% saline. Guest blogger Dr Sandheeah Ramdeny Over The Wall, is an amazing activity camp which is free for children, teenagers and family who are living with serious health challenges. It is a national charity which provide support to kids who are faced with seious health challenges through transformational residential camps across the UK. There are different camps which take place at different times of the year some of the camps focused mainly on the kids living with serious health problems some on the siblings and some on the families. These kids who lives with their health problems are mostly affected by their illness and are unable to participate in fun activities normally enjoyed by their friends and peers. Consequently, these kids then have a reduced self-esteem and self-confidence which can negatively impact on their growth and their development. The main purpose of Over the Wall, is to tackle these issues to allow a transformational change to occur in a safe environment with medical professionals being around to provide the medical care that they need so that the campers return with a new sense of their abilities and ambitions and improved self-confidence. I choose to take part in the health challenge camp which was mainly focused on the kids with serious health challenges which took place in Strathallan, a really nice boarding school located in Perth, Scotland with breath taking landscapes. The medical team were named the ‘Beach Patrol’, which consisted of 5 paediatric Spr, on GP, one paramedic, two nurses. The camp lasted for a week and the first few days were mainly centred around simulation scenarios to deal with the different cases which could arise whilst in camp as well as becoming familiar with the medical condition of the campers and to learn about their individual management plan. There were around 60 campers with a wide range of medical condition ranging from Type 1 diabetic, ALL, sickle cell disease, cerebral palsy, medical condition requiring bowel washout, Haemophilla, Marfan syndrome, Noonan’s syndrome, DiGeorge syndrome, kids with heart failure, patients on daily chemotherapy. Our normal day would start at 07 30 am in the morning and end around 2230 with 2 of us taking turns to do a night shift to provide cover each night. As the medical team, we were involved in giving the campers their medication before breakfast, during lunch and dinner time and accompanying the campers whilst they were carrying out their activities such as ensuring the young Type 1 diabetic would have their blood sugar level monitored and insulin administered accordingly. Each one of us would be closely attached to a camper who could potentially become sick so that we would be able to keep a close eye on them and we would accompany them to all the activities. Most of the activities were based on the campus of the boarding school. For instance, each day would have activities planned such as archery, music, drama, swimming, arts and crafts. These activities would be focused to allow them to realise their potential and us trying to make them believe in themselves and go beyond what they can do. The evenings were based mainly on Talent night where the campers would do an interesting act, play, dance or music to demonstrate each of their talent. There was one day, when the whole team went to Edinburgh to go to the international climbing arena. This was an excellent opportunity to allow campers to reach beyond their capabilities. For instance, on the camper in my group, a lovely 8 year old girl, who was afraid of heights and did not want to attempt any climbing. However, when she saw the other kids having so much fun and me being by her side telling her that I would be here and she could just attempt to climb and that she didn’t have to go too far. She was initially reluctant but the finally agreed. When she started climbing., she realised that she wasn’t scared anymore and was able to climb. When she got down, she was very emotional as she was now able to do something that she could not do. She said that she would never forget this experience. Some of the statements of the campers from Over The Wall, “It is no exaggeration to say that my experience with OTW was on the best weeks of my life. It Is true what they say.” To me, I do believe that Over The Wall provides an amazing opportunity to allow seriously ill children to go beyond the boundaries of their illness and have a positive impact for the rest of their life. For more information go to www.otw.org.uk NH Gent Belfort Hotel, Ghent, Belgium 22-24th June 2018 Annabel Greenwood ST3 Trainee, Wales Deanery The 4th INAC was held in the beautiful and charming city of Ghent, Belgium. The INAC was established to provide a global platform for neonatologists and budding-neonatologists across the world to come together and share their work on the recent advances in neonatal medicine. This year’s meeting was hosted by the Belgian Society of Neonatal Medicine, led by their President, Professor Filip Cools. An exciting programme was awaited, packed full of brilliant talks delivered by highly esteemed neonatologists, and included a showcase of diverse abstracts from all over the world. Delegates attended from over 50 countries across five continents. The conference itself was perfectly situated, set upon a quaint cobbled street, running alongside the iconic canal that winds its way through the vibrant city. From a personal perspective, I was extremely excited to present my work on organ donation on an international stage. Organ donation in neonatal medicine remains a fairly new concept, and I felt privileged to have the opportunity to fly the flag for organ donation, raising awareness and sharing my knowledge and experiences with others at such a prestigious event. I was fortunate enough to be joined by my colleague and friend, Dr Chris Course, on the trip, who was presenting the WREN Project we collaborated on with Dr Zoe Howard, on postnatal antibiotic use across Wales. Our project fitted in perfectly with one of the principal themes of the conference, namely antibiotic stewardship. There was a particular emphasis on neonatal neurology over the course of the weekend, and it was fascinating to learn of the latest developments in such a complex and challenging field. Professor Jose Honold discussed the concept of a ‘Neuro NICU’, a collaborative approach between neurologists, neonatologists, radiologists, neurosurgeons, neurophysiologists, and specially trained neonatal neurology nurses, using specialised equipment to optimise the management of conditions such as high grade IVH, meningitis and encephalitis, seizures, HIE, and those with congenital cerebral malformations. Another highlight was learning about the recent advances in neonatal lung ultrasound by Dr Luigi Cattarossi, to help guide the diagnosis and management of a number of lung diseases including RDS, TTN, pneumonia and pneumothoracies. This quick and focused bedside diagnostic approach has been shown to be as reliable as CXR in demonstrating lung pathology, resulting in less exposure to radiation for the neonate. It was also of great interest to learn about the challenges faced in neonatal medicine in developing countries, and demonstrated the importance of the implementation of simple interventions e.g. bubble CPAP, in making a huge difference in the survival of preterm infants with respiratory distress. Aside from the conference, there was plenty of time to relax and explore the local delights of Ghent. The city was electric as fans set-up camp in the square to cheer-on their country in the Football World Cup! I certainly enjoyed sampling the local delicacies, Belgian waffles being a particular highlight! As the weekend drew to a close, I reflected on what had been a truly fantastic conference. The INAC 2018 provided an excellent platform for learning and certainly inspired new project proposals and ideas to take back to Wales! Next year's conference is planned to be in Tijuana, Mexico with a pre-conference in San Diego, so a little further afield, but another couple of top destinations for sure!
Dr Rebecca Broomfield http://www.peruki.org/ @PERUKItweep As a member of PERUKI and a representative for WREN I attended the update day at the RCPCH London office on June 4th 2018. What is PERUKI?  Paediatric Emergency Research in the United Kingdom & Ireland (PERUKI) brings together clinicians and researchers who share the vision of improving the emergency care of children through high quality multi-centre research. PERUKI also takes an active role in encouraging and mentoring new investigators in the acquisition of research skills, regarding this as a key area for the sustainability of PEM research going forward Why is it important? Paediatric Emergency Medicine,Can strengthen their research activities by working together across the nations. Enabling co-ordination of research activities, and focus on common goals and agendas will help to achieve stronger outcomes. Large scale robust multi-centre clinical research will be developed and delivered over time, and translation into practice will be achieved throughout the health regions. Can I become a member? Yes! If you are interested go to the website (http://www.peruki.org/) and complete the sign up form. What is going on?  So much fantastic research in a variety of states. Some studies have completed recruitment such as the ECLiPSE study (http://www.eclipse-study.org.uk/) which we were involved in at the University Hospital of Wales - I have never been as excited about research as when I managed to randomise the first patient we recruited. Others are established and ongoing such as the CAP-IT study which we are also involved in recruiting for in Wales. Even more are just about to begin such as the FORCE study on Torus fracture management by Mr Dan Perry (@DanPerry), the NOVEMBR study on the use of non invasive ventilation in Bronchiolitis, Paul Macnamara and the SCIENCE study. But the day was also to present problems and potential research ideas. Professor Steve Cunningham presented the problems with research into pre-school wheeze and need for clarification of the grey areas between the ages of 2-4 years and the conflicting evidence base which we currently have. We had a reminder from Dr Tom Waterfield (@DrTomWaterfield) about the importance of establishing the clinical features which make a child with a non-blanching rash and a temperature more likely to have a meningicoccal sepsis than another illness. The rates of meningitis are falling - do we need to act now and progress this research before we miss the opportunity to capture this information. Which features make the child more likely to be unwell and which can differentiate those who are sick with those who are not. Information was presented on the HEEADSSS tool and discussion led by Dr David James (@DrDaveJames) about the definition of adolescence - should it be defined as the ages 10-24 years? and they would rather be 'young people'. Young people presenting to the emergency department are a big group, and this is increasing. As emergency paediatricians can we do something for this group of the population and should we be. The HEEADSSS tool (Home, Education, Eating, Activities, Drugs, Sexuality, Suicide, Safety) is useful but only if you know what services are available in your area and how to signpost people to them. Could we also utilize PERUKI to reduce variation in practice? An example discussed on the day was the use of metal detectors for ingested objects. There was no consistency about the level of training which people had to use the equipment as well as the areas of the body which were scanned. Also there was an inconsistency about what people did with the information when they used the equipment. There was also discussion about findings elsewhere which have not been replicated in the UK data. For example the rotavirus vaccination has been associated with a reduction of seizures elsewhere but the data from the UK does not show this. Why is this? We use a different vaccine could this be the reason or are we not collecting the right data. This demonstrates to me an important feature of research which is to know what is going on and be able to pick up trends in data and potential secondary outcomes which may be unexpected. The future? Is bright! We've taken a few ideas forward for projects within UHW and I am excited to hear the results of the ECLiPSE study.
If you are interested; become a member, follow the twitter feed and attend an update day for more information. If you have any interest in collaborative working, getting involved in research or providing the best care for your patients I would suggest it's worth a look. Princess of Wales Hospital, Bridgend, Friday 8thJune 2018 Annabel Greenwood Paediatric ST3 Trainee Broadly speaking, I feel our exposure to safeguarding training in the early years of paediatric training is limited.
Before you know it, you are the registrar on-call, out of hours, contacted with a complex child protection referral. As a junior paediatric trainee about to transition to middle-grade training, I will inevitably at some point, be faced with this scenario, and if I’m to be completely honest, the thought has previously caused a slight degree of tachycardia, hyperventilation and perspiration on my part, at the uncertainty of such a situation! I therefore searched for a way to dispel my fears and came across a child protection simulation course set-up by Dr Emily Payne, ST8 Community Paediatric Trainee in Wales. This fantastic one-day, multiagency simulation course has certainly enhanced my confidence in the management of child protection cases and I would certainly recommend the day to my fellow trainees. The course facilitates approximately 6-10 trainees, a perfect sized group to allow plenty of opportunity to ask questions and share our experiences with each other. The day began with a couple of short lectures, setting the scene for the day, addressing some key safeguarding principles, including the rights and responsibilities of all doctors, and an outline of the child protection process. We also discussed the ‘ACE’ (Adverse Child Experiences) Study, which has demonstrated that for every 100 adults in Wales, 47 have suffered at least one ACE during their childhood, and 14 people suffered 4 or more events. ACE are stressful experiences occurring during childhood that directly harm a child e.g. sexual, physical or emotional abuse, or effect the environment in which they live e.g. domestic violence, mental health, parental separation. It has been shown that ACE impact across the life course, e.g. affecting neurodevelopment in the early years, potentially causing social, emotional, and cognitive impairment, and perhaps leading to the adoption of high-risk behaviours and crime later on in life. Later in the morning we divided into pairs for 3 workshop sessions focusing on physical, emotional and sexual abuse respectively. These informal, small-group workshops were based on a clinical scenario and provided an excellent opportunity to voice any queries or concerns we had regarding the different categories of abuse. In the afternoon, we worked through a number of simulation child protection scenarios with actors playing the role of the child’s parents, making the situation as realistic as possible. At the end of each scenario we re-grouped to provide feedback and discuss the case in more detail. I felt that this was a completely safe environment to practice leading challenging safeguarding scenarios, and found it extremely useful to receive constructive multiagency feedback, from doctors, social workers and the police. The day was brought to a close with a simulated strategy meeting, and we all played the role of a different member of the multiagency team. This provided a fantastic insight into the role of each member of the team, and demonstrated how everyone works together to collate the evidence in order to generate an accurate account of events, to ensure the safety of the child. I thoroughly enjoyed the course and feel that I will now make the transition to middle-grade training with enhanced knowledge and confidence to manage challenging safeguarding scenarios. 22nd June 2018, Swansea Marriot Hotel Gill Smith, ST4 Paediatrics Trainee, Wales Deanery The spring 2018 WPS meeting was held in a very sunny Swansea. The sun shone down on the beach next to the Marriot hotel which provided a beautiful view during breaks between some excellent presentations and some very thought-provoking talks. The morning presentations were on very varied and interesting topics, which included audits and quality improvement projects from medical students, paediatric trainees and consultants. Presentations from neonatology to general paediatrics meant that there was something for everybody. I particularly enjoyed the presentation by the co-host of the WPS meeting, Dr Carol Sullivan who spoke with enthusiasm and wit about writing a student textbook in paediatrics. It looks like it will be a hit. Just before coffee, we were delighted to see Dr Peter Dale adorned in a bright pink wig and pink cape to highlight and talk about the approaching change to the RCPCH curriculum-progress. He went pink for Progress. Details can be found on the RCPCH website. More fantastic presentations ensued after coffee and the morning session was rounded off with a presentation on the problems encountered by babies born in the late pre-term period. Often thought to be close to term that physiologically they would be similar to those babies born at term. Evidence suggests this is not the case and is certainly gave us food for thought prior to lunch. A brilliant and tasty selection of food was available for lunch, finished by coffee and a chance to chat with the exhibitors. The lunch break was also a great opportunity to pop outside and enjoy the glorious sunshine and beautiful views overlooking the mumbles. After lunch we were kept from any thoughts of postprandial sleepiness by another set of wonderful and stimulating presentations. The first lecture back, presented by Dr Sheena Durnin was perfectly timed about of the use of paediatric pain relief practices in emergency departments in the UK and Ireland. These practices were evaluated across 40 hospitals in the UK and Ireland. It found a wide variety of practices in terms of analgesia used, timing of analgesia policies, and availability of play specialists to name a few. Dr Durnin earned the award of best presentation. Congratulations! Next up, another award winning presentation by Dr Rachel Morris who spoke so eloquently and with such passion about the implementation of family integrated care in a tertiary neonatal unit. The results were encouraging in that since the introduction of Family integrated care there had been an increase in breast feeding rates and a reduction in the length of stay and an anecdotal feeling that parents felt more in control and were ready for discharge sooner. Dr Morris won the best trainee award and this was thoroughly deserved. Following another round of superb presentations, the mid afternoon session was rounded off with an absolute gem of a talk from invited speaker Dr Mark Stacey, consultant anaesthetist and Associate Dean in Cardiff and Vale NHS Trust. The talk entitled ‘A Bakers’ Dozen Resilience Skills’ got us up and thinking. We had to write ourselves thirteen points to aid us in our resilience at work and life and included sleep, meditation and taking care of yourself. Some very important points and recommendations made. This talk left many feeling invigorated and gave us something to talk about during the afternoon tea break over coffee and cake before the late afternoon session. Fuelled with caffeine and carrot cake we had a further four short quick fire talks and the day was completed with a guest lecture from Dr Michael Farquhar, Consultant Paediatrician in children’s sleep medicine at Evelina Children’s hospital. His talk entitled “Rounded with a sleep: Why We Need To Talk About Fatigue” discussed the importance of sleep and gave a convincing argument for the need for all of us to sleep well. Night shift workers are encouraged to take power naps as this will improve our senses, judgement skills and general wellbeing. This talk went beautifully well with the Resilience talk and is definitely something we should all try and think about. Driving tired can be as bad as if driving after drinking alcohol. We made our way to the beach to enjoy the rest of the sunshine before a delightful dinner with colleagues and friends. A lovely end to a fantastic day.
Once again the WPS conference was a great success, showing a very talented bunch of people. It was thought-provoking and inspiring and a great way to meet up with colleagues and brilliant guest speakers. I’m off to get some sleep before the winter meeting (I prescribed it to myself)! Guest post from Dr Laura Potts, Clinical Leadership Fellow, Paediatric Trainee, Wales Deanery The Medical Women’s Federation (MWF) was founded in 1917. They aim to advance the personal and professional development of women in medicine, to change discriminatory attitudes and practices and to work on behalf of women patients and their families.
This year’s spring conference in Cardiff covered a broad range of topics affecting women from living and working with a disability through to antenatal screening and management of HIV. The first talk ‘Prenatal testing ; risks or certainty’ was given by Dr Annie Procter, Consultant clinical geneticist. She discussed the evolution of antenatal testing and its future directions. The potential scope of antenatal screening is vast, especially with the introduction of fetal DNA analysis in maternal blood, but routine screening is currently limited to the three major trisomies. This thought provoking talk advised caution; should we test for everything we can, just because we can? It also highlighted the importance of managing families expectations effectively. Dr Olwen Williams spoke about the progress in HIV and AIDS management in recent years. Huge advance have been made and are now close to enabling affected women to have normal deliveries and breastfeed. Women are however, still presenting with late disease and later in life, with and opportunistic infection and Kaposi sarcoma. She also reinforced the results of the recent PARTNER study which showed that in those with an undetectable viral load, transmission to their partner did not occur. There is a new public health initiative promoting Undetectable = untransmissable. There were also a number of abstract presentations. Of particular interest was the work being done at Singleton neonatal intensive care unit on family integrated care (FiCare), presented by Dr Rachel Morris (ST5 Paediatric trainee and trainee representative for the MWF in Wales) . Family integrated care is centred around four main themes – staff education, parent education, creating the right NICU environment and providing psychosocial support. The concept originated in Estonia and was developed by Professor Lee and colleagues in Toronto. It has been shown to reduce length of stay, retinopathy of prematurity and infections and increase breast feeding rates. Singleton have already had a lot of success, receiving excellent feedback from families and demonstrating reduced length of stay and increased breast feeding rates. During the afternoon there were a number of workshops. I attended Dr Cora Doherty’s session on wellbeing and the healthy team. For optimal team effectiveness and performance mind, body and spirit must be considered, that is to say the team needs a clear vision, good morale and trust and have their physical needs met. The concept of the ‘fitness’ of team members to be part of the team was also considered and how we as team members and leaders have a responsibility to protect our own wellbeing and that of our team. During the remainder of the afternoon there was an interesting talk titled ‘menopause behind the headlines’. Whilst not particularly relevant to our patients it was a delightful insight into what some of us have to look forward to! Dr Clarissa Fabre, President elect of the Medical Women’s International Association (MWIA) shared the results of the most recent MWIA members survey. This included some worrying statistics such as 57% of respondents felt that they had been discriminated in their career, with 41% reporting that they had experienced sexual harassment or bullying in relation to their work. Unfortunately younger doctors reported lover job satisfaction, more sexual harassment and bullying and a higher incidence of stress and burnout. The conference ended with the Dame Hilda Rose lecture, given by Dr Sally Davies, focusing on the importance of stories such as Dr Frances Morgan’s. She was the first woman to receive a doctorate in Medicine in Europe and the first female doctor registered in Wales. She was a pioneer in medical practice and social reform, working all over the world as well as working as a General Practitioner in Wales. These stories demonstrated how far women have come in achieving gender equality but that there is more work to be done, as highlighted by the recent MWIA survey. The MWF work hard to fight discrimination against women in medicine, for example, challenging Jeremy Hunt on the lack of impact assessment for the new junior doctor contact in England and helping to tackle the gender pay gap. An interesting quote was offered at the end of her talk, ‘good practice benefits all, bad practice affects women more’. I wonder what you all think of this? The key messages from this lecture and the conference in general were that huge progress has been made by women in medicine and in women’s health and that we all have a responsibility to report and challenge bad practice and behaviour, and make looking after ourselves and each other a priority. For anyone interested in finding out more about the MWF their website can be found at www.medicalwomensfederation.org.uk Dr Tim Warlow, Paediatric Palliative Care GRID trainee, Wales Deanery Few of us can forget recent cases in the press of Alfie Evans and Charlie Gard. Such tragic cases of breakdown in relationship between families and care teams. I’m sure that alongside my own cries you have had the thought ‘Surely things didn’t have to get to this!’ These cases bring into stark clarity the importance of our skills of communication and our ability to put into practice the ethical and legal duties to involve of families and children in decision making. These cases are nightmare scenarios, but at some points in our career we will face similar challenging situations. Aware of these issues, the All Wales Paediatric Palliative Care Team received £20,000 of Welsh Government funding to improve the skills of paediatricians in these areas. Our response was to organise a series of free workshops exploring issues of ‘communicating difficult news’, decision making and advanced care planning in paediatrics. April 2018 saw the first of these workshops in the fantastic Copthorne Hotel, Culverhouse Cross. Within a month we had filled all our places and the response on the day from delegates was fantastic. The truly multidisciplinary event was attended by consultants, community nurses, therapists, trainees and hospice staff, all of whom engaged amazingly in communications skills breakout groups and seminars. There was time to explore advanced communication skills, read and use the Paediatric Advanced Care (PAC) Plan, and consider the views of families and young people in planning. The highlight of the day was without a doubt an interview with one of our parents whose son sadly died under the care of our service. She discussed the value of good communication, of doctors being prepared and sensitive, and the benefit of early and co-ordinated planning.
The good news is that there are several further days being organised, one for each of the health boards in Wales. The next of these is in Swansea where Dr Griffiths will be using trained actors to facilitate what will be an exhilarating day of interactive learning together with other professionals. Please contact education@tyhafan.orgfor further information about upcoming days and to sign up. All workshops are free of charge and are in great venues with food provided. If doing a good job of communicating and parallel planning with families excites your interest, these days are for you. If you want to run a mile, these days are even more for you! Let’s get to grips with the really difficult stuff of paediatrics, lets help families to live well and for those whose lives are cut short, to live well right to the end. Dr Annabel Greenwood (ST3), inspired by Dr Ian Morris (Consultant Neonatologist, UHW)
Relevance– How important is the content of the article to me, my patients, and my practice? The title and the abstract will help you answer these questions. Internal validity– How sound is the study? i.e. how accurate is the study? Look at the methods to help ascertain this. External validity– How applicableis the article to my practice? i.e how much can I generalize it? The methods and results sections will help you assess the external validity. Now, with those 3 key principles in mind, let us picture the scene… You’re an ST7 trainee, approaching the end of your paediatric training, years of hard work and dedication behind you, your CCT within touching distance. You’re at your START assessment, the last hurdle before consultancy, and now for your critical appraisal station. Twenty minutesto read the article AND then appraise?! How on earth am I going to do this I hear you cry?! Stay calm, take a deep breath, and burst forth the 9 key questions that will help you ace the station! Describe the study What is the type of study (principal method) What type of question is being asked? (e.g. Diagnostic? Therapeutic? Economic?) Where was the study carried out? (is it multicentred or single study) What are the key features?
Describe the research question
What is the relevance of the question? This is usually described in the introduction. Is it an important question? Is it worth reading on? Does it correlate to your clinical practice/scenario? Describe the methods Use the PICO template, but expand…. What are the inclusion/exclusion criteria? Is there any masking or blinding? Are there any secondary outcomes? Comment on the internal validity i.e. how accurate is the study? Use various checklists e.g. CONSORT, STROBE, PRISMA Is there a risk of bias? Summarise the primary results Summarise the key secondary results(briefly) Comment on the External validity– i.e. describe the generalizability of these findings Were the inclusion/exclusion criteria reflective? Limitations? Consider the paper in conjunction with other studies i.e. how does it fit with the evidence out there? Conclusion Overall, does this paper help you answer your clinical question? Important to look at the clinical context! ….And just like that, you did it! 9 logical, concise steps to critical appraisal for the START assessment. Of course, this is only a suggested approach, but one which I will most certainly be adopting for future critical appraisals. Now, where did I put that journal?.....
Dr Rebecca Broomfield Why is it important? The environment created in the workplace is vitally important to the wellbeing of the staff who work there. In clinical medicine this also translates into the wellbeing of patients and ultimately their safety. So what can you do, as a leader, to ensure that your workplace environment is as positive and functional as it could be? This topic was first visited during the Faculty of Medical Leadership and Management (FMLM) conference in Liverpool and covered in the Leadership blog in December. It was covered here by Henry Stewart. He runs the Happy company, which has been listed as one of the 20 best workplaces in the UK for five successive years (www.happy.co.uk). Henry Stewart has also written “The Happy Manifesto” He has identified that people work better when they are challenged and given freedom. As a manager we should be enabling people to innovate, and rather than focusing on weaknesses we should develop our strengths. Mistakes should be celebrated and, within the boundaries of clear principles and targets, team members should be given freedom and ownership of projects. The topic has come up time and time again within the Leadership program I am currently enrolled on. Happier workplaces function better, lead to greater innovation and better results. What can you do? Within a quality improvement program provided by Cardiff and Vale Health board, we recieved a afternoon workshop to discover how we can use positive psychology to improve our own happiness and that of our workplace. This was delivered by Mark Hodder. People tend to currently live with the mindset "I will be happy when....I've lost weight/I have a promotion/I own a bigger house" Thus success creates happiness. Rather than this way of looking at happiness what would happen if we looked at it from the opposite direction, shifting our paradigm and focusing on happiness bringing success? Learnt helplessness is a huge problem, but now we know this we can challenge this and learn positivity. When driving home from work try thinking of 3 positive things which happened that day. They don't have to be big things, just build it into your daily routinue. In work in order to build positive relationships we need 3 positive interactions to every negative one. Can you within your workplace build in positive feedback or interactions. How often do you praise people or say thank you? Could you do this more? Think about how you motivate your team. For praise to be most beneficial it should be given for effort rather than ability. By praising for ability you run the risk of creating a fixed mindset which then has the potential to cause a drop off in performance. Effort and recognising hard work by saying "Thank you" or "I can see you have put a lot of work into ..." A growth mindset is created promoting positivity and providing motivation. When you encounter a problem or a difficulty could you Dispute, Distract, Distance? This technique creates a mindset that setbacks are tempory, local and changeable rather than spiralling into a negative perspective or allowing negative feelings to dominate a workplace. Problems are actively dealt with. What about your face? Consider who your face is for? .... (clue it's not for you!) Your face and body language are ways of communicating to other people. Faces have so much to give away we just have to focus on them and see it. In the same way, we need to be aware of what our face is saying about us and how we can use this to our advantage - smiling is contagious! When we are interacting with people often their facial expressions and body language mirror our own, therefore our behaviour and attitude matters. Think about what your daily facial expressions project about your emptions onto your team. And finally ..... helping other people will help you. 5 random acts of kindness a day have been shown to reduce cortisol levels and thus reduce stress, see how many you can build into your day. Further reading: The Happy Manifesto: Make Your Organiszation a Great Workplace By Henry Stewart
The Chimp Paradox: The Mind Management Programme to Help You Achieve Sucess, Confidence and Happiness By Prof Steve Peters http://www.markhodder.net/ - Links to articles from the workshops and contact details for Mark Hodder. Guest Post: Dr Roisin Begley Preparing for RCPCH Progress: What you need to know 2018 is the year of huge change in paediatric training with the introduction in August of the new RCPCH Progress Curriculum. All trainees will move from the current curriculum to RCPCH Progress, unless they are due to CCT before 15 September 2019. You will not need to re-demonstrate achievement of training levels already completed under the old curriculum ie Level 2 trainees will not need to evidence again that they have met the requirements of Level 1 training. Preparing for Progress: guidance and resources What is different about RCPCH Progress? 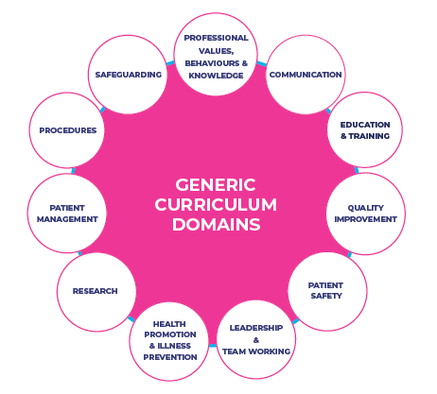 The new curriculum is based on a framework of learning outcomes as opposed to the current list of competencies, and incorporates the Generic Professional Capabilities the GMC expect of all doctors. Collecting evidence for an outcomes based curriculum will be very different from getting a competency signed off. This new approach will allow greater flexibility for you to demonstrate achievement. The curriculum comprises:
Example: LEVEL 1: Curriculum Learning Outcome 2
Key Capabilities
Illustrations 1. Effective working relationships: • Demonstrates skills and strategies for effectively consulting with babies, young children, adolescents and their families in such a way that the child or young person and their family feel able to talk about difficult or emotional issues. • Manages disruptive or antisocial behaviour in children, adolescents and families in clinical settings if it occurs. • Applies knowledge of how different factors influence a patient’s journey and how they may impact effective communication and cause anxiety about treatment and illness. • Communicates, with support, with parents and the rest of the family of a patient who has an acute or chronic illness, is hospitalised, or has died. • Discusses the indications, benefits and possible risks associated with a procedure to obtain informed consent from patients and parents or carers for a procedure that the trainee is competent themselves to perform. A comprehensive range of materials have been produced and are now available from the RCPCH Progress webpage. This webpage, www.rcpch.ac.uk/progress is regularly updated with additional resources and information. Opinions from those using Progress Dr Sophie Con, Wales Deanery Paediatric SHO
"The new curriculum is certainly more succinct than the last. It does take some time to find your way around it though. Sometimes you wish it would be more specific! I think it is more achievable to find an illustration for each point than the previous curriculum" Dr Tim Warlow, Paediatric Palliative Medicine Trainee, Wales Deanery “Our speciality was chosen alongside a small selection of others to trial the new RCPCH progress curriculum. You will be pleased to know that this is an immeasurable improvement on the old curriculum. There are key learning objectives within which are ‘key capabilities’. We link these to our portfolio entries. They are far fewer in number and much better worded than in the previous version. The whole layout and menu selection is much more intuitive, with submenus relating logically within their categories. This is a refreshing change from what was a baffling and frustrating previous system. In combination with what is a much better new portfolio in ‘kaizen’, it feels as through the portfolio might be becoming fit for purpose as a way of signposting our learning, helping us to monitor our progress, and enabling our supervisors to see a clearer picture of what we have been doing. Well done RCPCH!” by Chris Course, Chair WREN Summary
The Welsh Research and Eduction Network (WREN) Spring Study Day took place at the Princess of Wales Hospital, Bridgend on 11th May 2018. Once again, attendance was well supported by doctors from across the training grades (and an Advanced Neonatal Nurse Practitioner!), as well as Dr Huma Mazhar (from Singleton Hospital), Dr Naomi Simmons (from Glan Clwyd Hospital) and Dr Judith van der Voort (Head of School) joining us for the day to learn more about how the network is getting on and our current activities. Our educational programme was once again diverse, with talks from Dr Phil Connor and Rhian Thomas-Turner about the new Children and Young Adult’s Research Unit at Noah’s Ark Children’s Hospital for Wales and their plans for increasing junior doctor involvement. Dr Ian Morris then gave an excellent strategy for rapid-fire critical appraisal, with an emphasis on the START assessment (slides available on our website, or on request). Dr Gethin Pugh from the Quality Improvement Skills Team at the Wales Deanery also gave us an introductory workshop to Quality Improvement, as well as teaching us the basics of the Plan, Do, Act, Study model and signposting the further QI training opportunities available. The WREN Blog continues to go from strength to strength and now receives over 500 hits a month on our articles, under the editorial leadership of Dr Rebecca Broomfield and Dr Annabel Greenwood. They are looking for contributors too, so if you have something to share or a topic you’d love to write about, please get in touch. Four new projects are being undertaken via the network, three of which are starting now. Details of the WREN projects and their project leads are below. Project leads can be contacted on the Current Project Portfolio page. We will be disseminating these projects amongst the units, but if you would like to get involved in any of the projects in WREN’s current portfolio, please contact the project leads (details below). If you have an idea for a project you would like to develop with WREN’s help, please contact either myself or Siwan Lloyd via our website, or using the details at the top of this newsletter. The next WREN study day is planned for November 2018 (confirmed date to follow), and we hope that you will be able to join us for another stimulating and thought-provoking study day, building on from the success of the last! Newly Launched Projects Project Title: ‘The Impact of the Meningococcal B Vaccination on Septic Screens’ Project Leads: Dr Ele Jones (ST5) and Dr Rebecca Towler (ST5) Description: Pyrexia is a common adverse effect of the Meningocccal B vaccination. NICE guidelines exist for the management of fever <3 months of age and recommends investigations for sepsis for pyrexial infants but does not make comment of post-vaccination infants. This project aims to retrospectively assess how infants are managed in paediatric and neonatal units who are presenting with fever post-Meningococcal B vaccination over a 12-month period. Project Title: ‘Aiming to improve paediatric trainees confidence with ECG interpretation’ Project Leads: Dr Ankita Jain (ST6) Description: The Paediatric Cardiology department at UHW gets several referrals a month from various hospitals to provide their opinion on ECGs done on children for various clinical indications. We would like to help improve confidence in paediatric ECG interpretation, and have developed a structured online educational module. Using a pre- and post-quiz on ECG interpretation it is hoped to show how skills can be improved. The link for the quiz is https://goo.gl/forms/2Qj8NBZHBdOYL33d2 Project Title: ‘Can a resus drug App help improve accuracy and reduce stress in time-critical scenarios?’ Project Lead: Dr Jordan Evans (ST5) Description: Accurate calculation of WETFLAG resus drugs is critical, but can be affected by stress and the time-critical nature of emergency scenarios. This project aims to assess whether a smartphone app can help to improve prescribing accuracy and reduce doctor stress levels in resus situations. A pilot study has shown an App to be effective, and this project aims to assess larger numbers of doctors and nurses using the technology in simulated scenarios. Ongoing Projects Project Title: ‘Head injuries on the postnatal wards’ Project Lead: Siwan Lloyd, ST3 Description: A pilot study at UHW has demonstrated that infants being accidentally dropped on the postnatal ward is not an uncommon occurrence, however their management and level of investigation following injury was very variable. Following on from this, an all Wales study is underway to determine the incidence, risk factors and management used, with the aim of producing a best practice guideline for these infants and their parents. Project Title: ‘Re-audit of the Management of Respiratory Distress Syndrome in Preterm Infants’ Project Lead: Chris Course, ST4 Description: Following the initial audit in 2014/2015 by WREN, a Wales Neonatal Network guideline was introduced for the Management of RDS in Preterm Infants in June 2016. The re-audit has commenced March 2018 and is running for six months to assess how the new national guideline has affected patient care. Project Title: ‘Management of feverish illness in infants <3 months old’ Project Lead: Blanche Lumb, ST1 Description: Do we consistently meet the NICE standards set in the investigation of sepsis in <3 month old infants? This project aims to assess that the appropriate investigations occur in a timely manner, and that appropriate empirical treatment is commenced across paediatric assessment units in Wales. Where we chose to deviate from the guidance, are we documenting this appropriately? Upcoming Projects (Planned Start September 2018) Project Title: ‘Evaluating the impact of the introduction of the SEREN program on Type 1 Diabetes Management in Children’ Project Lead: Matthew Ryan, ST6 Description: SEREN is a structured education package for children newly diagnosed with T1DM. This project will assess SEREN’s impact by using Quality of Life questionnaires, serial HbA1c measurements and number of DKA admissions for children diagnosed with T1DM in the years pre and post introduction. Dr Annabel Greenwood As Trainee Representative for Paediatric and Neonatal Organ Donation for Cardiff and the Vale Health Board, I was very much looking forward to this opportunity to spread the word and raise awareness about organ donation. The concept of organ donation in paediatric practice is relatively new but currently very topical, and a recent article in the March edition of Archives of Disease in Childhood highlighted the fact that despite recent attempts to promote organ donation, donation rates remain fairly static, particularly in the neonatal intensive care setting. The knowledge and experience of paediatric organ donation amongst healthcare professionals is limited, and it was therefore of no surprise that when we enquired at the beginning of the simulation day whether participants had ever been involved in a case of organ donation, only two had previous experience, one of which was in adult medicine. The paediatric simulation day was the first of its kind in Wales, and it was fantastic to see such a wide variety of the multidisciplinary team in attendance, all enthusiastic to learn more about organ donation and the processes involved. The day began with a case presentation from Gail Melvin, one of the brilliant ‘SNODs’ (Specialist Nurse in Organ Donation). She recalled one of her experiences of neonatal organ donation and it provided a great insight into the referral process from the consideration of organ donation, right through to harvesting in theatre. This set the scene perfectly for the simulation scenario, as the aim was to work through a case from presentation to the emergency department, to withdrawal of life-sustaining treatment, prior to organ donation. The scenario was broken down into sections, with a debriefing session after each section to optimise the opportunity for discussion. Actors played the role of the child’s parents, allowing candidates to practice the often difficult and sensitive encounters with families regarding the withdrawal of life-sustaining treatment. The afternoon session consisted of workshop sessions, covering brainstem death testing and communication skills stations relevant to organ donation. There was also a brief session outlining a quality improvement project I am currently undertaking aiming to raise awareness of paediatric and neonatal organ donation at a trainee level. The day was brought to a close with a parents’ account of their personal experiences of organ donation. This really hit home the huge impact organ donation can have not only on those receiving a donation, but also on the families of the donor. It was incredible to hear the strength the family were able to take in the face of extreme adversity and despair, in the knowledge that their child was able to help save the life of others through the donation of their organs. The organ donation team received excellent feedback regarding the simulation day, and following its success, we hope to build upon our education programme, extending similar opportunities to healthcare professionals across Wales. A date for the diary is an upcoming organ donation deanery study day in August…final details to be confirmed! If you have any queries about paediatric organ donation or would like to get involved, please feel free to contact me. For more information on organ donation please visit:
https://www.organdonation.nhs.uk/ Dr Rebecca Broomfield Photo credits to Dr Sara Long, Dr Kathryn James, Dr Laura Potts Leadership course run in MIT Boston USA As Clinical Leadership Fellows we were privileged to have the opportunity to attend a Leadership Course at Massachusetts Institute of Technology. 5 of us hopped on a plane at the end of March and flew over to Boston in order to attend Applied Neuroscience: Unleashing Brain Power for You and Your People We flew in the day before the course and in true tourist fashion made the most of the first day getting over jet lag before the course began. None of us had been to Boston before and despite venturing out to an Irish bar with live music on our arrival we were all up bright and early on the Monday morning. (Thanks jet lag!) We grabbed our lonely planet guides and re-embraced our travelling student identities to explore a fantastic city. We spent the day following the Freedom Trail - Boston has a very limited history but what it does have it exploits amazingly! The trail lead us through the start of the American Independence and British invasion. We stopped off in the harbour at lunch time and took a (freezing cold!) boat trip too see all the islands. We continued our trail and then extended it to include a viewing of the bronze duck statues in the main park. We watched the sunset in the tallest building in Boston with cocktails that were stronger than they tasted! Day 1 The course was facilitated by Dr Tara Swart (@TaraSwart) She holds a BSc in Biomedical Science and PhD in Neuropharmacology from Kings college London. She read Medicine at Oxford University gaining a BM BcH qualification. She is an executive coach and is passionate about disseminating simple, pragmatic neuroscience-based messages that change the way people work. This course was not aimed at medics, and I do feel that we would have benefited from a slightly more rigorous focus on the scientific evidence for some of the science taught on the course, however, this was not it's aim and in fact may have alienated some of the audience who were present. Having looked into the evidence presented since the course, there is a significant scientific knowledge base behind the methods taught. There has never been a room where, as a medic, Imposter Syndrome has a more appropriate setting. The course was full of chief executives and people who have multi-million pound contracts in their back pockets and more staff working underneath them imagined possible! However, the problems encountered and the neuroscience to increase behaviors and lead change were relevant to both the medical and the commercial setting. The insight which mixing with leaders from completely different worlds to our own has allowed us to gain was worth attending the course alone. Right from the word go this course was structured differently to the majority. We sat on circular tables with 4-5 other delegates but at the back of the room were juggling balls, skipping ropes and standing desks. There were refreshments available through the whole day (although, caffeine was removed at 14:00 - it reduces your sleep quality after this time) and at the start we were actively encouraged to access refreshment as needed and walk around the classroom freely. While the skipping only occurred in the breaks some people did take advantage of the juggling balls and juggled at points throughout the teaching. While we learnt on the course that social safety is the area of culture in the workplace and wellbeing which has the biggest impact on the brain the next biggest area is physical activity. By standing up and engaging in a physical activity such as skipping or juggling we were actively engaging our brains and increasing our neuroplasticity, which is the brain's ability to reorganize itself by forming new neural connections throughout life. Brains tend to hold onto old pathways, in order to create new pathways you need to rest, fuel, hydrate and oxygenate your brain. by exercising you increase the release of brain derived neurotrophic factors (BDNF) which helps with the formation of new pathways. Neuroplasticity is an important concern when thinking about the neuroscience of leadership. We do not unlearn habits or behaviour, this is not possible but we are able to overwrite these pathways. Translated for use in leadership this could be as simple as giving people an alternative option rather than simply managing an undesirable or ineffective behaviour by saying "don't do that". Making new neural connections for behaviour is tough, but it is the first time which requires the most effort. As you repeat the same pattern of behaviour you strengthen this pathway and therefore make it more automatic. There are 2 areas of the brain involved with learning new behaviours; the cortex - which is learning by instruction and the limbic system which is learning by experience. Knowledge/organisation of reality happens in the pre-frontal cortex but feeling and managing anxiety is under the control of the limbic system. A brain stem reflex is often change preventing within behaviour modification. Logic is not enough in order to modify behaviour and promote change you need to connect the 2 systems. How can we use neuroscience to our advantage in the workplace? The top 7 emotional drivers within the workplace are:
Communication is one key area where neuroscience can give us the edge over others. Using your limbic system to promote bonding and enhance the emotions above can give you an edge in leadership. Trust is the number 1 emotion but trust uses more resources than mistrust, and is therefore more difficult to employ. Can you use neuroscience to create a better bond and increase trust? Yes, and it's as simple as eye contact. When you next communicate face to face with somebody try actively looking with your right eye into their left eye. This will activate their right limbic system which has been shown to create a strong bond. A bond enables colleges to feel more valued and creates a better working culture and environment. I've been trying this out since I returned and I feel that it has enabled me to shortcut some relationship building and create a quicker more valuable relationship. As far as I know, nobody has thought I've been looking at them strangely or even been aware that I am trying out this technique so even if it initially feels awkward for you it's worth a try! Face to face communication is always better, so make the effort to do this when possible. The role of stress .... The right ventral lateral pre frontal cortex is active in stress and has a role in regulating emotions. This area responds to pain - notably physical pain causes the release of natural painkillers whereas psychological pain does not, it also contains cortisol receptors. Cortisol is a fight or flight response hormone. It has a natural morning spike and then maintains low levels throughout the day accept in crisis or when there is a threat to survival. Having too much cortisol can lead to physical manifestations from yourself or the team which you are leading. These include poor sleep, irritability and craving chocolate/caffeine. The physical symptoms can detract from your brain power and demand attention, too much cortisol can also decrease your immunity and increase your abdominal fat thus impacting your physical health. Emotion biases all decisions and stress/fear biases decisions to the emotional system through the cortisol pathways. Interestingly some studies have shown that cortisol levels can be transmitted to others in a similar way to pheromones. Therefore a leader who has high levels of cortisone has the potential to expose others to them as well as themselves. Stress is just one of the recognised threats to your brain power in work, others include uncertainty and uncontrollability. As a leader you do have the power to influence these for your team. Can you adapt your leadership in order to make your team feel more in control of the tasks which they are performing? You can definitely reduce uncertainty. We did a good exercise on the course which focused on re-framing our responses. As a leader when a suggestion is made by a member of your team the automatic response is to say "No". In order to say yes it requires more mental energy as a leader but improving your ability to this can increase the level of control which your team feel they have and promote the positive emotional drivers outlined above. We were tasked in pairs of making a suggestion to overcome a problem to our partner. Initially they had to respond with "No" Then we had to re-ask the question and they had to a respond with "Yes, but .." thus entertaining the idea but outlining the potential barriers stopping this from happening. As the questioner we than had to once again make the same suggestion but our partner needed to respond with "Yes, and..." Using "Yes, and .." reduces the social isolation of your team and increases the attachment and bonding created. Oxytocin, which is released when creating a good bond, shapes the neutral circuitry of trust adaption. Reward and attachment emotions regulate emotion and improve decision making. Thus by utilising this type of leadership within your team you can promote good decision making and reduce stress. There is lots to gain A 10% improvement in performance is equivalent to an extra 23 working days annually. Other key points from day 1
During the course all food was provided and the menu was created to promote healthy eating and ensure that the nutrients provided promoted brain agility. It was followed up with an evening reception - I'm not sure where the wine fits into a healthy lifestyle but it was definitely welcome after all the information provided during the course. Our thanks also have to go to Mr William Fleming, a fellow course participant who took us out to sample the local seafood in the evening, but also allowed us to pick his corporate brain with ideas that could benefit our leadership styles and leadership within the NHS. (I think/hope he learnt a little bit from us too!) Day 2 During day 1 we were taught that people are 15% more productive on the days that they do 30 minutes of aerobic exercise in the morning. While i'm not sure this counts as aerobic exercise, we took this on board and as a group of Clinical Fellows all attended the precourse early morning yoga session. The picture above is the view from the glass walled classroom we were practicing in, this rivals the morning session of beach yoga I took part in while travelling for the most breathtaking yoga view. It was a calming start to the day, followed by a breakfast of foods, as yesterday specifically selected to enhance wellbeing and increase brain agility. We were more focused on day 2 on our own strengths and weaknesses and what we can do to improve our leadership while increasing our own resilience and mental toughness. If we can maintain our mental toughness and resilience as leaders then we promote a culture within our organisation that it is important to do the same. "Nobody would get into a car without filling it up or maintaining it - Why do we not do this with ourselves?" Maximise your potential Prior to the course we completed a Neurozone questionnaire. This is a detailed questionnaire which enables you to focus on small changes you can make to maximise your own potential and therefore improve your leadership. Two of my areas for focus are improving my sleep and increasing the diversity of my exercise. Both of these require a small change but have the potential to have a big impact on my reserves. Culture Culture and patterns of behaviour and beliefs frequently impact perception, cognition and actions. You have a responsibility as a leader to use your skills to create a culture where your team members thrive. Your actions as a leader speak louder than the word which you use. My take home messages ...
What am I doing differently since the course?
Further reading: “Neuroscience for Leadership: Harnessing the Brain Gain Advantage” Tara Swart, Kitty Chisholm & Paul Brown We had a day to play with before flying home, part of my year is focusing on simulation and medical education. Therefore I took advantage of being in Boston to visit the 'Centre for Medical Simulation' which has a worldwide reputation. There was a course going on that day and so I got to see their sim suite in action and speak to their faculty. It was very interesting to note that they are also focusing on the educational value of simulation and how we can evidence this. Their facilities are excellent and it was exciting to be able to spend a short time there.
The afternoon was spent at the Boston Tea Party museum learning about leaders who promoted a change by making a stand - very relevant to the topics which we had been covering, and yet another leadership perspective. Boston was fantastic, I would recommend it as a city break. The course was an amazing opportunity to understand some of the rational behind current leadership techniques and put a neuroscience basis to their implementation. I have a lot of areas to work on to maximise my own leadership potential and am looking forward to trialling these out over the coming years. Dr Rebecca Broomfield Photo credits to Dr Sara Long Please read this blog with Nickelback "What are you waiting for?" playing in the background. It encapsulates the mood i'm aiming for! https://youtu.be/w-Ng5muAAcg Nestled somewhere near the middle of Wales, with very limited phone signal and Wi-Fi that intermittently functions is Elan Valley. Its a stunning location to explore for people who love outdoor adventures and the location for a fantastic 3 day team building residential which was facilitated by Academi Wales as a part of the Pg Cert qualification I am enrolled in during my year as a Clinical Leadership Fellow. It is an amazing place to focus on team-working and your role within that team. During the residential course we studied the Belbin Team Roles, how they interact together and our personal preferences. My team was facilitated by Phil Davies, who is an ex Wales international player and currently the Head coach at the Nambian national Rugby union side. As a head coach of an international team, Phil offered a different perspective on team working from the traditional NHS viewpoint. (And I've stolen the Nickelback song from him - Thanks Phil!) Team-working is something which often doesn't get enough time within the NHS. By being aware of its importance and how you function within a team you should be able to more readily achieve your goals. Belbin Team Roles What is Belbin? A team role as defined by Dr Meredith Belbin is "A tendency to behave, contribute and interrelate with others in a particular way" He has grouped these roles into 9 clusters of behaviour. When you take the Belbin self reported questionnaire you get a break down of your personal team preferences. The outline of the roles is described in the picture below. You don't need a person for each role to create a good team but you should try to consider all perspectives. It may be also useful to look at a team which isn't functioning to its best, does everybody within that team have the same preference and therefore the same perspective on a problem. Having the same preference can be a source of conflict as well as preventing the team achieving its goal. My primary preference was the 'Shaper' role with my secondary preference being 'Resource Investigator' As a group of Leadership fellows we had surprisingly diverse results, reinforcing that no type is better or worse in a leadership role. The report was slightly different from the other personality or preference reports we have completed this year. Instead of looking at areas to develop we were encouraged to focus on developing our strengths rather improving on our weaknesses. Each role has it's own strengths and weaknesses, knowing the preference of your team member allows you to distribute workload to their strengths, thus improving the efficiency of your team. For example, I had a low score for the 'Completer Finisher' role therefore, as a leader, I need to identify a person on my team who has strengths in this role in order to ensure my team actually completes their tasks! Once we had learnt the theory and our own preferences we were split into teams in order to put this into practice. The teams were selected in order to ensure that the majority of the roles were covered in within team. The details of what exactly happened in Elan Valley will forever stay amongst the team who attended. (Trust is an important part of creating a functioning efficient team environment!) But we participated in a variety of tasks that allowed us to explore our own role and communicating and motivating the other team members. The morning focused on goal based tasks. Each task started had a time limit and started with a printed instruction. Each task had rules which could not be broken and a goal which needed to be achieved. An example of one of the tasks we undertook was a maze task. A maze was laid out out of sight from the team and we were put into a large square laid out on the ground unable to see the maze. Our team was only allowed to communicate within the box, only 1 team member was able to leave the box at any one time and all members had to successfully navigate their way across the maze to complete the task. There was of course a time limit on this. Our first team member returned to tell us the structure of the maze, we had to work out, remember and communicate a pattern of boxes which we could step on to get across to the other side of the maze. This task acutely demonstrated to me the importance of others perspectives and the importance of communication. People like to be communicated with differently depending on their thought processes. (Just in case you were wondering we managed to get all of our team members across within the time limit and only received one penalty!) The afternoon was structured slightly differently. The whole cohort was brought back together and we were to function as subsections of an overarching team. The team goal was to earn 'money'. The money would then be spend on unlocking clues which would give us the location of a prize which we were aiming to achieve. We could earn money by completing a variety of tasks. Tasks were diverse and each has a value attached to it. We split into our sub-groups and decided which tasks we wanted to complete in order to earn money and then spend the afternoon working through these tasks. Again, of course there was a time limit set on this. All the subgroups had to come back together to decide how this money was spent. Some of the afternoon tasks were more adventurous and required taking team work to a whole other level. My personal favorite task was the "leap of faith". This involved climbing up a tiny rope ladder onto a small triangle platform which was positioned high into the trees and then jumping off. You were harnessed and your team members were in control of the ropes. In order to work your way up the ladder you needed to trust your team members not to let you fall with the ropes, you needed a team member to anchor your ladder to stop it flapping about in the wind and enable you to climb straight and you needed encouragement from the team when halfway up you suddenly realised that it was a long way down! Despite ripping a pair of jeans I managed to get to the top and jump. It was a good exercise in overcoming barriers and how important support and trust were within a team. (Just for completeness we earned enough money and managed to get a well earned box of chocolates!) Take home messages .... I learnt a surprising amount about myself and team roles from participating in the residential course. However, the most important of these was Communication The role of communication in good team-working cannot be underestimated. It is vitally important especially when you've realised that people don't all think like you or have the same perspective as you do. Obviously this covers the face-to-face communication when outlining a task but also the importance when managing a large busy team in communicating the overarching vision of the team which you want all members to progress towards. It is very difficult to motivate and drive forward a team when you do not all have a shared vision as to what you want to achieve. I would suggest reflecting on how you manage a team and the actions you use to motivate other members. How many conflicts or mistakes have been due to poor communication? Other than communication the importance of looking at things from others perspectives was emphasised to me throughout these personally challenging activities. When faced with a problem, taking on a different viewpoint or consulting a member of your team who you know has a different role preference to you can fundamentally change how you choose to tackle it. As a part of this it is also important to remember the importance of your role within your team, you may have a perspective which nobody else has considered. Do you need to work on Active listening? Listening is a vital part of communication. However, it's importance can often get overlooked when concerned about getting your opinion heard and shouting loud enough to have your say in a team activity. How many times do you have a conversation where you are already planning your answer? the next point your want to make? or even thinking about what you are having for dinner that evening. (Unsurprisingly) communication works best when you actually listen to the people in your team. When you honestly reflect on this can you say that you always do this? Most people don't. Next time you are communicating with a college try giving them all of your attention, focusing in on what they say and responding to this rather than your previously planned out structure of how you want the conversation to go. Since trying this out after the residential I have noticed a significant improvement in my communications and my ability to influence change. Things I am currently working on developing are:
More information https://academiwales.gov.wales/
https://www.elanvalleylodge.co.uk/ http://www.belbin.com/ |
Editors
Dr Annabel Greenwood Categories
All
|





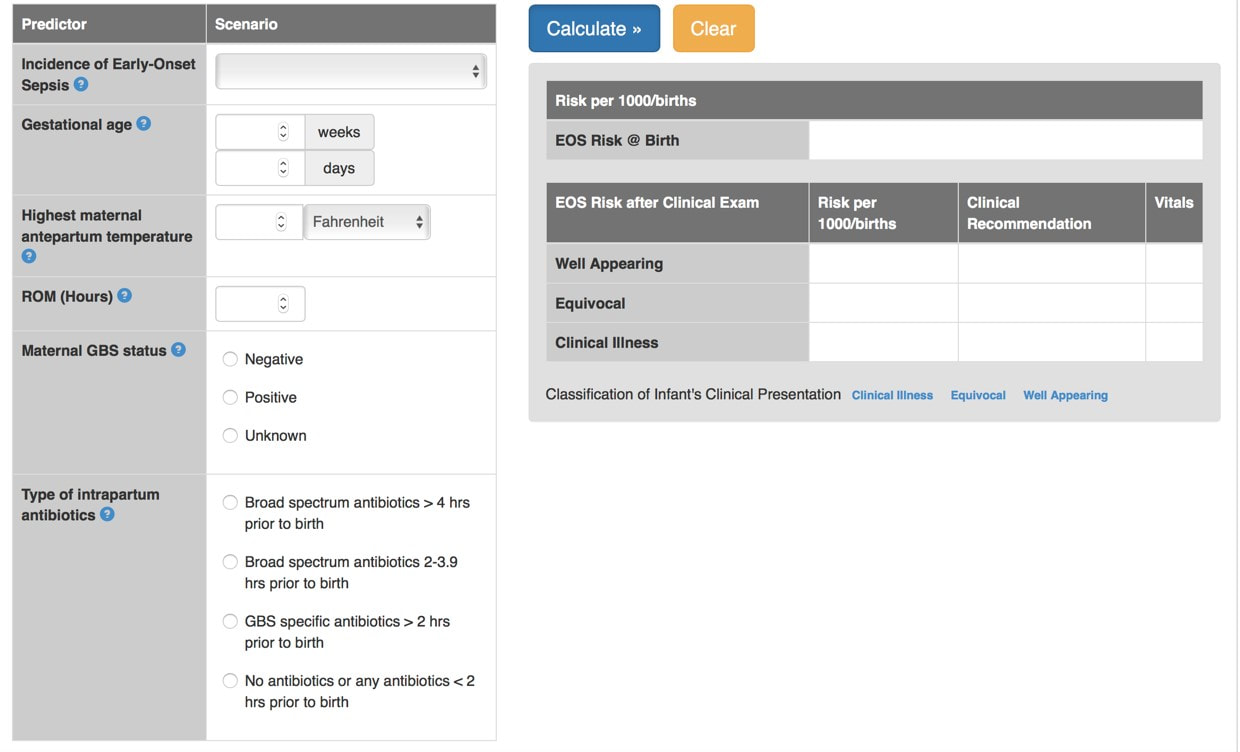
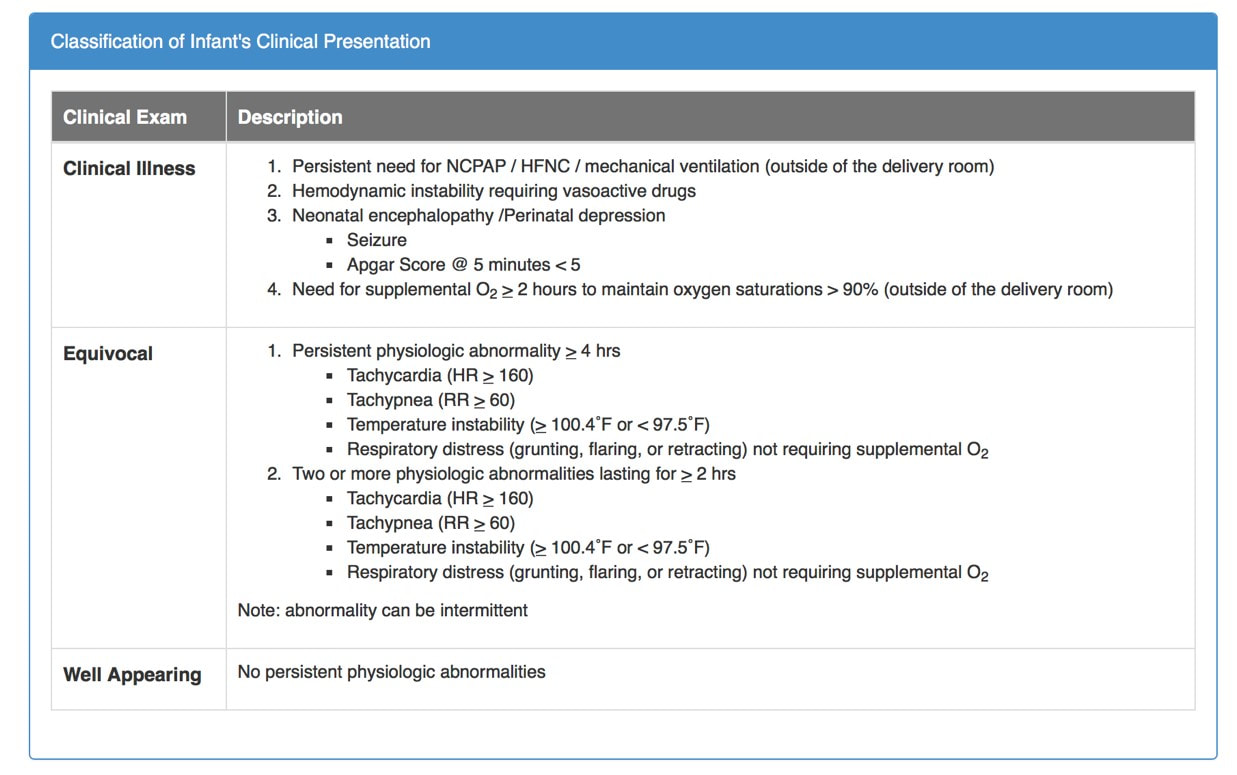











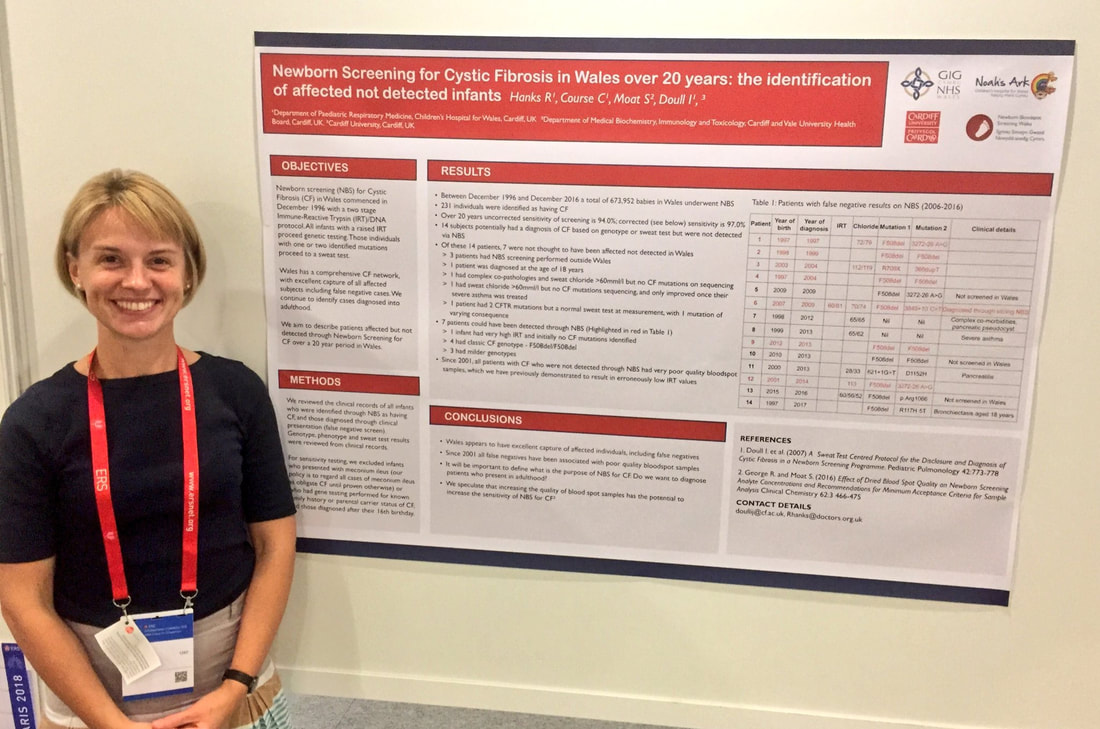

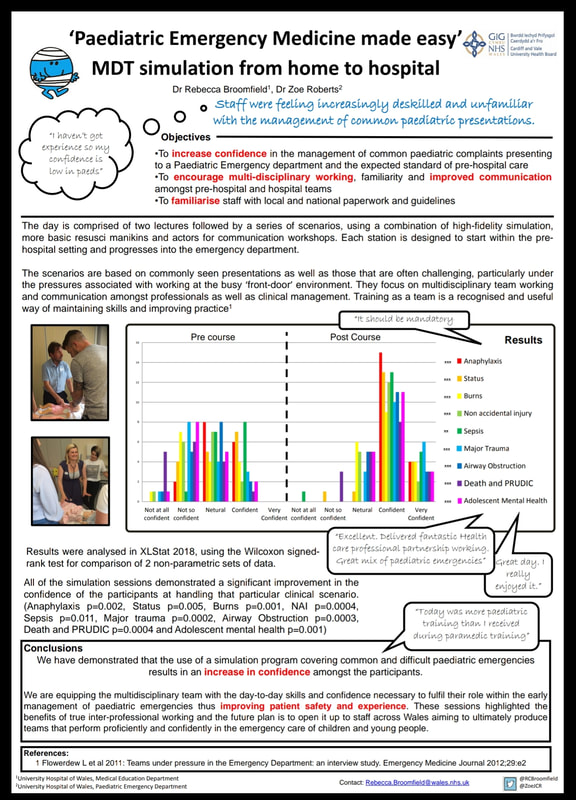

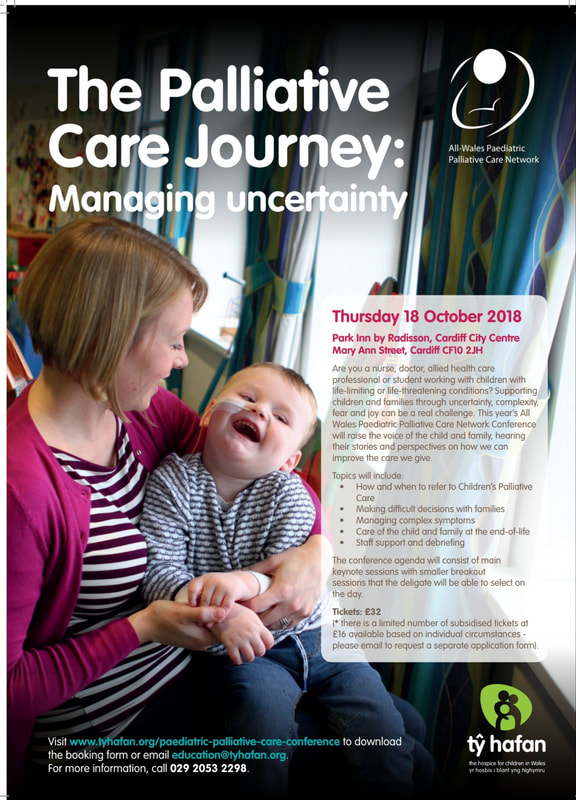


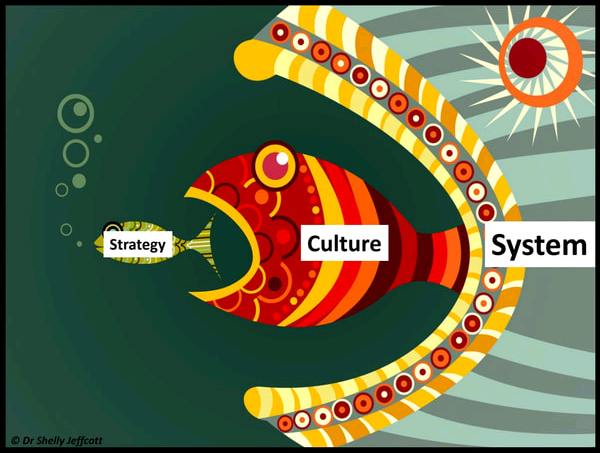
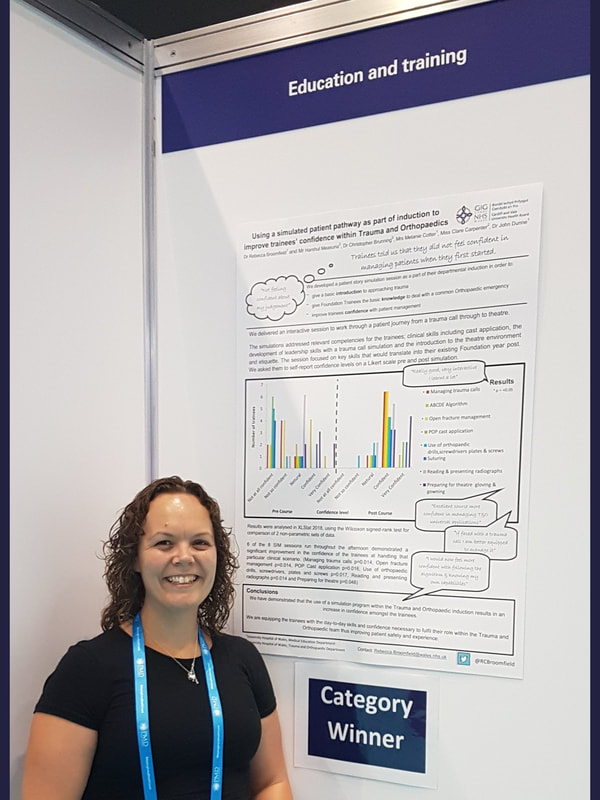




















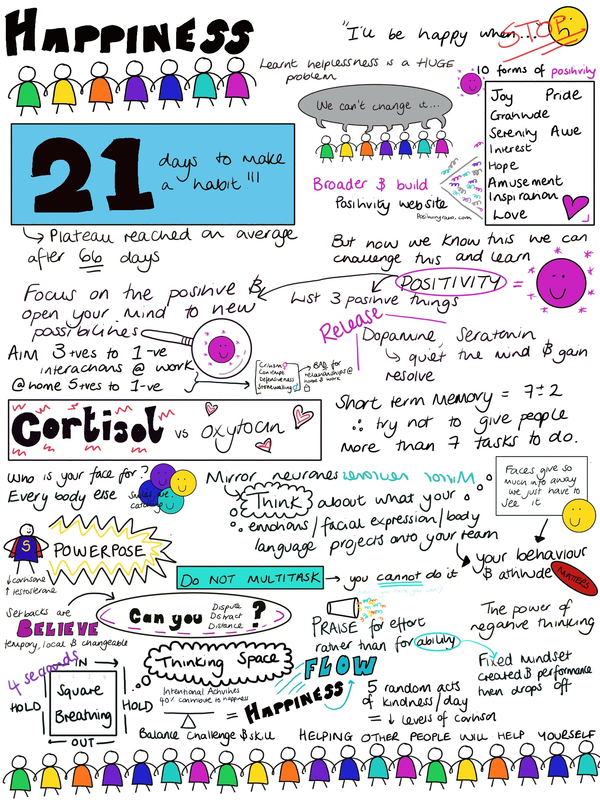

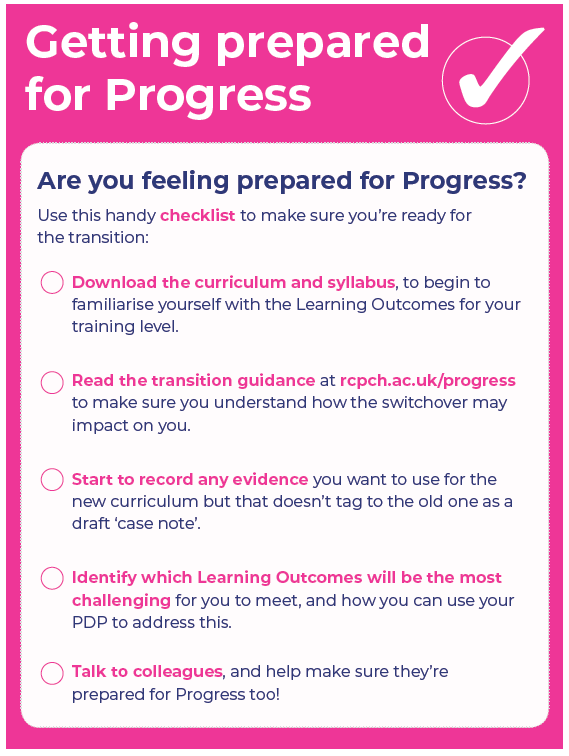













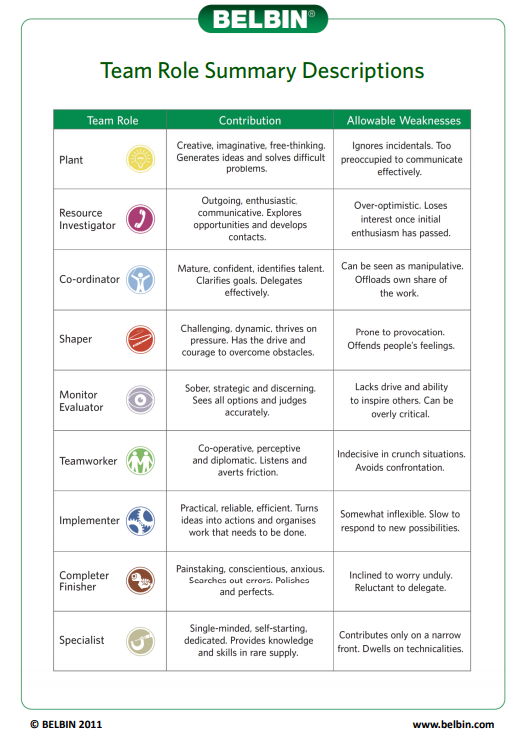


 RSS Feed
RSS Feed
