|
Dr Tom Cromarty Editor Interests: Paediatric Emergency Medicine, Medical Engagement and Leadership, Simulation, Quality Improvement, Research Twitter: @Tomcromarty |
Welsh Research and Education Network
WREN BlogHot topics in research and medical education, in Wales and beyond
Dr Celyn Kenny Editor Interests: Neonates, Neurodevelopment, Sepsis, Media and Broadcasting Twitter: @Celynkenny |
|
‘The Palliative Care Journey: Managing Uncertainty’ Guest blogger Dr Tim Warlow Senior Registrar All Wales Paediatric Palliative Care Network Following the success of last years All Wales Paediatric Palliative Care Network Conference, the team are excited to introduce the much anticipated 2018 conference. This year we will be exploring the palliative care journey from the perspective of the child and family. Hearing from the families themselves, the day will follow their journey from diagnosis through to bereavement. Some of the questions we will be asking include: • When should palliative care be introduced and how do I raise the issue with families? • How do I support families whilst making difficult decisions about their child’s care? • What are the spiritual needs of families at the end of their child’s life? • How do I manage difficult and unfamiliar symptoms at the end of life? • How do I approach uncertainty and grief? • How can Ty Hafan Children’s Hospice help me to provide holistic care to families? When working with families of sick children, many of the most challenging issues we face are also the most rewarding when done well. This day aims to unveil those daunting aspects of care, provide ample opportunity for discussion, and hearing from the expert parents and professionals as to how we can serve our families better. The morning will focus on introducing palliative care and decision making, especially relevant in light of recent high-profile media cases. We will consider how we can involve children better in decisions relating to their care, collaborating with families to ensure they feel listened to and valued whilst navigating legal and ethical uncertainties. Next we will hear from families of children with life limiting conditions themselves. What were the most challenging times, and what actions of professionals were key to their palliative care journey? What was helpful, what was harmful? We will consider how each professional on their journey played a key role in ensuring excellent holistic palliative care and what we can learn from one another. Finally, the afternoon will include a series of breakout groups to provide opportunity to really get stuck in exploring an aspect of the palliative care journey that is a priority for you. There will be time to discuss and ask questions in a smaller group setting. Topics include supporting children and families at the end of life, managing difficult symptoms, supporting grief, bereavement and spiritual care, and how to support staff including debriefing. Last year’s conference was booked up quickly and over 100 delegates had a fantastic day. Now in its fourth year we have built on the lessons of previous years, responded to your feedback, and produced a day which promises to be challenging, rewarding, and a fascinating insight into the lives of our patients and families through their own eyes. Here is some feedback from last year’s conference as a taster of what delegates took away: “Learnt many new things. Was challenged on preconceptions and pre-existing myths of Palliative Care. Enjoyed the professional, but personal element for some speakers / discussions.” “ Excellent day from start to finish, sessions we interesting, informative and thought provoking.” “I was hooked from start to finish” “The case studies/discussion groups with the panel of different professionals involved with the neonate and their families’ journey were excellent and thought provoking. These were great for learning about how processes can work well and can adapt along the way.” We look forward to you joining us in October Key details Date: 18th October 2018
• Location: Park Inn by Radisson Hotel, Cardiff City Centre • Cost: £32 per person (£16 subsidised tickets available for students and upon individual request) • Bookings and information: [email protected]
2 Comments
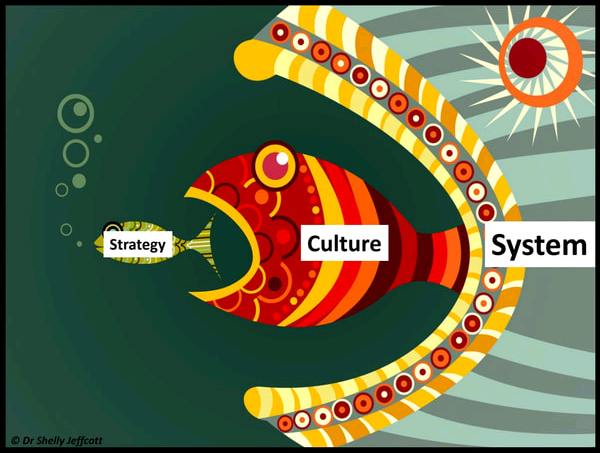
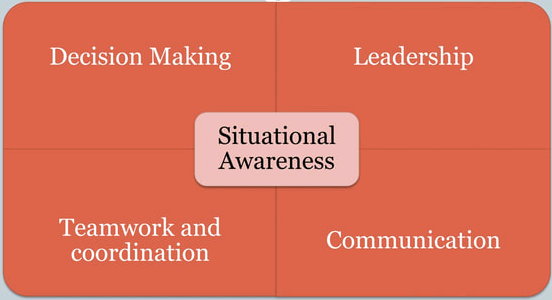
9th-10th July 2018 Dr Rebecca Broomfield The Patient Safety Congress aims to transform the UK’s approach to delivering high quality care. It champions patient safety as the organising principle of a healthcare system which is truly efficient, effective and able to offer the best experience to patients and carers. I was lucky to be able to attend the Conference in Manchester in July. Prior to attending I had minimal experience with the Health Service Journal who sponsor the event and although clearly focusing my training and clinical work on optimising patient safety I knew very little about this movement within healthcare. The HSJ run awards and publish a journal purely focusing on and publishing patient safety initiatives and ways which can all make out practice patient focused and as safe as possible. The conference was busy and if I am completely honest the timetable when I first looked at it was completely overwhelming. There was key note lectures which drew the participants together and then 5 streams running throughout the 2 days which you could dip in and out of to cover the sessions which most interested you and met your personal learning needs. Along with an exhibition centre and poster presentations focusing on 9 different topic areas. Unfortunately due to childcare compromises (working parent problems!) I wasn’t able to travel up to Manchester until the Monday morning so missed the opening keynote speakers which I was reliably informed were excellent and predicted the exit of The Right Honourable Jeremy Hunt from his health secretary post, but unfortunately the predicted replacement Dr Kevin Fong turned out to be less accurate! When I arrived I set up shop in the Human Factors stream. The streams for day 1 were: Human factors, Delivering quality improvement on the frontline, Driving a culture of patient safety, Improving patient safety through governance and compliance and finally Bridging the gap: policy and clinical Practice. The human factors stream was chaired by Martin Bromiley OBE (@MartinBromiley) of medical “Just a routine operation” fame https://www.youtube.com/watch?v=JzlvgtPIof4 – if you don’t know who he is or his story as a healthcare professional then you really should so click on the youtube link and learn about it. What is human factors? As defined by NHS England Human Factors for healthcare are: “Enhancing clinical performance through an understanding of the effects of teamwork, tasks, equipment, workspace, culture and organisation on human behaviour and abilities and application of that knowledge in clinical settings”. Essentially it is about Making it easy to do the right thing The stream started well and I very much enjoyed hearing from 3 speakers talking about how they had introduced human factors within their areas or work and outlining the importance of doing do. Dr Shelly Jeffcott (@drjeffcott) spoke first about the importance of human factors and outlined some goals. She emphasised designing the systems so that it is easy to do the right thing and the importance of integrating human factors training in the medical workforce. Education for Scotland have developed an e-learning package on human factors. It is easy to create an account and access this at: https://turasdashboard.nes.nhs.scot//User/PersonalDetails/Create?openIdApplicationId=e8c7cbb9-34fd-4c87-8c6c-7232cf6786d7 Next up in this session was Mr Simon Paterson-Brown (@spbsurgery) he spoke about the use of training within a surgical environment to develop non technical skills. His sessions Non-Technical Skills for Surgeons have international acclaim and have been widely published. Finally the session ended with Professor George Youngson (@ggyrach) whop focused on thE impact of bullying and discrimination in care systems. Bullying is a huge problem in the NHS and this was outlined during this session Professor Youngson identified that it is still a problem and has done work proving its detrimental effect on patient safety. He encouraged us to speak up for safety and ensure that bullying was addressed in our departments. The stream then moved onto the nudge theory and how we can use this within the NHS. Helping people to make the right decision at the right time thus improving patient safety. During this session there was talk about the noble prize winning book “Thinking fast and slow” by Daniel Kahneman looking at the way people make decisions and how the nudge theory exploits this. By understanding how people behave we can design better policies and systems to improve patient safety. The EAST framework was suggested here: Easy, Attractive, Social and Timely. Any change in behaviour should fit into this framework. And where there is variation in practice it offers a good target for change. After lunch I remained in the Human Factors stream and the session delivered by Abbie Coutts and Professor Bryn Baxendale (@gasmanbax) focusing on situational awareness. During this session it was the first time in this conference that I was exposed to a patient story being used to demonstrate a learning point. This is something which was utilised through the conference, across many different streams and had a truly powerful impact. Abbie Coutts presented her father’s case and observations on why errors occurred. She has used the errors in care which happened to her father to teach the health board which cared for him about human factors. She suggests that this should be taught by people doing the job and understand why errors happen in order to address them rather than just how they happened. Professor Bryn Baxendale then spoke about balancing acts and how to embedded key skills and behaviours into practice. Both speakers focused on normalising excellence and doing the simple things well. The fourth session in the human factors stream again used a patient story presented by Kathryn Walton https://www.youtube.com/watch?v=r7gk1AvZKZA We heard from the patient, the healthcare worker and what happened afterwards. I would encourage everybody to follow the link about and listen to the story. This was an exceptionally emotive story and emphasised. The final breakout session I attended was delivered by The GMC within the Driving a culture of patient safety stream who presented a discussion on the GMC survey and understanding this data in relation to patient safety. The keynote to end day one was delivered by Professor Alison Leary (@alisonleary1) and focused on the fact the “Hope is not a plan” and within medicine what we can learn from other safety critical industries. Professor Leary presented an the fact that the very structure of the NHS is significantly different to other safety critical industries in that we place our most junior inexperienced staff at the front line closest to the operational risk, with the experienced workforce behind the scenes. This is in contrast to other industries who use their experienced work force next to the operational risk and use them to allocate selected work to the junior teams. In the NHS we need to be focusing on rewarding frontline experts to stay where they are on the shop floors rather than moving them further and further away into managerial positions. We need to use good policy and education where the expectations are clear and safety is mandated alongside clear credible leadership. Her closing statement was particularly poignant and a quote from Dr Tracy Dillinger NASA “People defer to hope, but when failure is not an option, hope is not a plan” We went out for dinner in Manchester as a group of leadership fellows and I can 100% recommend The Alchemist for cocktails because they are fantastic, and for those based in South Wales one has just opened in Cardiff (yay!). Back to the conference ...! Day 2 Day 2 opened with the prize giving for the poster competition. I entered 2 posters and this one won its category of ‘Education and Training’ Proof that if you do an interesting improvement project then it’s always worth popping it into a conference because you never know how far it might go. The keynotes opened with Dr Bill Kirkup presenting themes which happen when things go wrong and how we should use these to make sure that as organisations we do not get into situations where things go wrong. He identified the follow themes: - Failure to learn He ended with 5 key points for maintaining patient safety: - Listen to the patient, they are telling you the answer - Honesty not reputation management - Investigate and learn – not suppressing bad news and learning from others mistakes - Dismissing and denial leads to a slippery slope which is harder to stop - Do NOT think “It will never happen here” The second keynote was also focused on investigations but from the Healthcare Safety Investigation Branch and what we can learn from the investigations which they have already processed. It is worth reading the summary documents of these investigations as it is different from a root cause analysis which will take place internally. They look at the route cause but also ask “why?” Again day 2 was split into streams. The 6 streams on day 2 were: Collaborating to achieve patient safety, Delivering improvement on the frontline, Using research to solve the big challenges, Prioritising safety for vulnerable people, workforce the crucial ingredient for safety and Bridging the gap: Policy and the clinical practice. I attended Leading from the top: New research on trust level leadership under the using research to solve the big challenges stream. I left this session feeling quite negative. The panel presented learning which they felt had happened since the Frances Report. Which seemed to be, in their opinions, very little. They appeared to feel that this was a continuing problem with variability in quality and consistency of leadership practises. I feel (esp. as a current leadership fellow) that the Wales deanery is actively promoting and encouraging learning about clinical leadership. And I would signpost anybody to the FMLM website if they want more information on clinical leadership. https://www.fmlm.ac.uk/ I then attended the LEDER program, http://www.bristol.ac.uk/sps/leder/, focusing on what needs to change for people with a learning disability in order to ensure their safety, under the Prioritising safety for vulnerable people. Again this focused on a patient story presenting the experience of the family of Oliver McGowan. (@PaulaMc007) They are campaigning for mandatory training for healthcare professional in how to adapt for patient with autism and learning difficulties. They want to work on preventing these stories and raise awareness for people to make reasonable adjustments. They encourage communication, an overriding theme from this year, with the patients, and their families as they know the patient best. Then, before lunch I moved into the Workforce stream to hear from Leigh Kendall (@leighakendall) Again this presentation focused on a patient story presenting Hugo’s story focusing on preventable harm within a maternity setting. Hugo was born after Leigh suffered from HELLP syndrome at 24 week gestation and lived for 35 days. She is working on improving bereavement information and including bereaved families in the quality improvement processes, alongside communication between healthcare professionals. She again encouraged communication and stated something which will stick with me “You can’t upset us anymore because the worst has already happened” Don’t be afraid to speak to bereaved families they can give you vital information and want to have a voice. Mr Edward Morris then presented the work of the Royal College of Obstetricians and Gynaecologists on Each baby counts (@EachBabyCounts) again focusing on patient stories and human factors to encourage a focus on communication and preventing harm. https://www.rcog.org.uk/eachbabycounts After lunch the conference was again brought back together for keynote sessions. The CQC Chief inspector of Hospitals, Professor Ted Baker, presented an evidence based argument for how Inspections can help us with patient safety. He encouraged us to engage and empower frontline staff to really focus on patient safety and put patients at the centre of what we do. He reminded us to “relentlessly focus on leadership and culture” but also to recognise that healthcare is a high risk area and we have to accept the implications of that fact. He believes that with backing the inspection process can be used to drive forward a culture of patient safety. The Right Honourable Jeremy Hunt MP was due to present next in his role of Secretary of State for Health and Social care, but as he had been relocated and Matt Hancock (@MattHancock) had been in the job for less than 24 hours Professor Bruce Keogh and Dr Aidan Fowler from 1000 Lives stepped up to be part of a panel for the next steps for patient safety. The conference closed hearing from a panel about how their organisations overcame safety challenges. The overriding themes were again all about culture, communication and mindset. If you can get this right then you seem to be on the right track! The Patient Safety Congress was a fantastic, engaging conference and if you get a chance to go I really would. The use of patient stories to focus the attendees was a really useful tool and one which I will take forward with other presentations in the future. It was a really important reminder that we do have the opportunity even as trainees to focus on patient safety and improve outcomes. More information can be found in the HSJ journal https://www.hsj.co.uk/ and on the patient safety congress website https://patientsafetycongress.co.uk/
Guest Blogger Dr Jordan Evans N Engl J Med 2018;378:2275-87. DOI: 10.1056/NEJMoa1716816 If there’s one thing we all know about manging diabetic ketoacidosis (DKA), it’s the importance of being extremely cautious with fluid management due to the risk of causing iatrogenic cerebral oedema right?...Wrong! Once again, like John Snow, we unfortunately ‘know nothing!’. When will the childhood lies end, Father Christmas isn’t real, the Easter bunny’s not real and now this, the most painful blow yet. In this PECARN (Pediatric Emergency Care Applied Research Network) study, published in the New England Journal of Medicine, Nathan Kuppermann et al investigated the influence of intravenous fluid administered on the rates of neurological injury in children with DKA. What was the reason for the study? Brain injury occurs in the region of 0.5% - 1% of DKA presentations. It presents with sudden neurological deterioration. Patients without a marked neurological deterioration may have more mild neurological impairments e.g. memory / cognitive impairment. As all of us were likely taught, brain injury in DKA has long been thought to be iatrogenic, secondary to fluid administration causing cerebral oedema due to osmotic gradients. The evidence for this school of thought is however lacking and evidence has emerged actively disputing it. Alternative explanations have been proposed that there may be something about being particularly unwell with DKA that leads to the neurological injury, possibly inflammatory or vascular changes. The more unwell the patient is the more likely they are to require fluid resuscitation and therefore an association between severe DKA with brain injury and fluid administration could be mistaken as causation. Remember that association is not proof of causation! Oedema may develop secondary to the brain injury itself as it does in other mechanisms of injury such as trauma. Where did the study take place? The study was conducted across 13 centres in the United States. Who did they include ? Children aged 0 – 18 years with a diagnosis of DKA (pH < 7.25, glucose > 16.7 mmol/L. Children with GCS <12 were excluded two years into study (due to concerns of treating clinicians). What did the investigators do? Children presenting to study centres with DKA were randomly assigned to one of the following four groups; 1) 0.9% saline fast administration 2) 0.9% saline slow administration 3) 0.45% saline fast administration 4) 0.45% saline slow administration The fast group were given a 20ml/kg bolus which was then followed with replacement of a 10% fluid deficit with the first half of the deficit volume being replaced over 12hrs and the rest over the next 24 hrs. The slow group were given a 10ml/kg bolus which was then followed by replacement volume for a 5% deficit which was given over 48hrs. The primary outcome was a decline in mental status (GCS <15 on two occasions within first 24 hours of treatment. Patients and parents were blinded but not the clinician. Secondary outcomes; clinically apparent brain injury (neurological deterioration leading to clinical decision to treat for raised ICP, intubation or death), short term memory, memory & IQ at 2 months and 6 months. What were the results? 4912 patients met the inclusion criteria. Due to the complexities of the study of these there were a total of 1389 episodes of DKA included in the study (from 1255 different children). There was a fall in GCS in 3.5% of these epsiodes (48 episodes). There was clinically apparent brain injury in 0.9% (12 episodes). There was no difference between the two groups for any of the outcomes. (Some of the raw results favoured the fast fluid administration group although none of these results reached a statistically significant level). Conclusions Kupperman et al. rightly concluded that ‘Neither the rate of administration nor the sodium chloride content of intravenous fluids significantly influenced neurologic outcomes in children with diabetic ketoacidosis’. Take home message for practice in Wales 1. We no longer need to be as anxious about giving fluid too fast in DKA
2. If you need to give a bolus for shock do so without fear of causing cerebral oedema, this study provides evidence that it’s not harmful. 3. With regards to the fluid deficit replacement although this study shows we could safely give it a little faster stick to current practice of the Wales DKA protocol as it doesn’t show any improvement in outcomes for the faster administration of IV fluids. 4. It’s worth remembering that there is good evidence for using 0.9% saline for maintenance IV fluids in children (to prevent hyponatraemia) so it’s not clear why they chose to have arms in this trial with both 0.9% saline and 0.45% saline. Guest blogger Dr Sandheeah Ramdeny Over The Wall, is an amazing activity camp which is free for children, teenagers and family who are living with serious health challenges. It is a national charity which provide support to kids who are faced with seious health challenges through transformational residential camps across the UK. There are different camps which take place at different times of the year some of the camps focused mainly on the kids living with serious health problems some on the siblings and some on the families. These kids who lives with their health problems are mostly affected by their illness and are unable to participate in fun activities normally enjoyed by their friends and peers. Consequently, these kids then have a reduced self-esteem and self-confidence which can negatively impact on their growth and their development. The main purpose of Over the Wall, is to tackle these issues to allow a transformational change to occur in a safe environment with medical professionals being around to provide the medical care that they need so that the campers return with a new sense of their abilities and ambitions and improved self-confidence. I choose to take part in the health challenge camp which was mainly focused on the kids with serious health challenges which took place in Strathallan, a really nice boarding school located in Perth, Scotland with breath taking landscapes. The medical team were named the ‘Beach Patrol’, which consisted of 5 paediatric Spr, on GP, one paramedic, two nurses. The camp lasted for a week and the first few days were mainly centred around simulation scenarios to deal with the different cases which could arise whilst in camp as well as becoming familiar with the medical condition of the campers and to learn about their individual management plan. There were around 60 campers with a wide range of medical condition ranging from Type 1 diabetic, ALL, sickle cell disease, cerebral palsy, medical condition requiring bowel washout, Haemophilla, Marfan syndrome, Noonan’s syndrome, DiGeorge syndrome, kids with heart failure, patients on daily chemotherapy. Our normal day would start at 07 30 am in the morning and end around 2230 with 2 of us taking turns to do a night shift to provide cover each night. As the medical team, we were involved in giving the campers their medication before breakfast, during lunch and dinner time and accompanying the campers whilst they were carrying out their activities such as ensuring the young Type 1 diabetic would have their blood sugar level monitored and insulin administered accordingly. Each one of us would be closely attached to a camper who could potentially become sick so that we would be able to keep a close eye on them and we would accompany them to all the activities. Most of the activities were based on the campus of the boarding school. For instance, each day would have activities planned such as archery, music, drama, swimming, arts and crafts. These activities would be focused to allow them to realise their potential and us trying to make them believe in themselves and go beyond what they can do. The evenings were based mainly on Talent night where the campers would do an interesting act, play, dance or music to demonstrate each of their talent. There was one day, when the whole team went to Edinburgh to go to the international climbing arena. This was an excellent opportunity to allow campers to reach beyond their capabilities. For instance, on the camper in my group, a lovely 8 year old girl, who was afraid of heights and did not want to attempt any climbing. However, when she saw the other kids having so much fun and me being by her side telling her that I would be here and she could just attempt to climb and that she didn’t have to go too far. She was initially reluctant but the finally agreed. When she started climbing., she realised that she wasn’t scared anymore and was able to climb. When she got down, she was very emotional as she was now able to do something that she could not do. She said that she would never forget this experience. Some of the statements of the campers from Over The Wall, “It is no exaggeration to say that my experience with OTW was on the best weeks of my life. It Is true what they say.” To me, I do believe that Over The Wall provides an amazing opportunity to allow seriously ill children to go beyond the boundaries of their illness and have a positive impact for the rest of their life. For more information go to www.otw.org.uk |
Editors
Dr Annabel Greenwood Categories
All
|









 RSS Feed
RSS Feed
