|
Dr Tom Cromarty Editor Interests: Paediatric Emergency Medicine, Medical Engagement and Leadership, Simulation, Quality Improvement, Research Twitter: @Tomcromarty |
Welsh Research and Education Network
WREN BlogHot topics in research and medical education, in Wales and beyond
Dr Celyn Kenny Editor Interests: Neonates, Neurodevelopment, Sepsis, Media and Broadcasting Twitter: @Celynkenny |
|
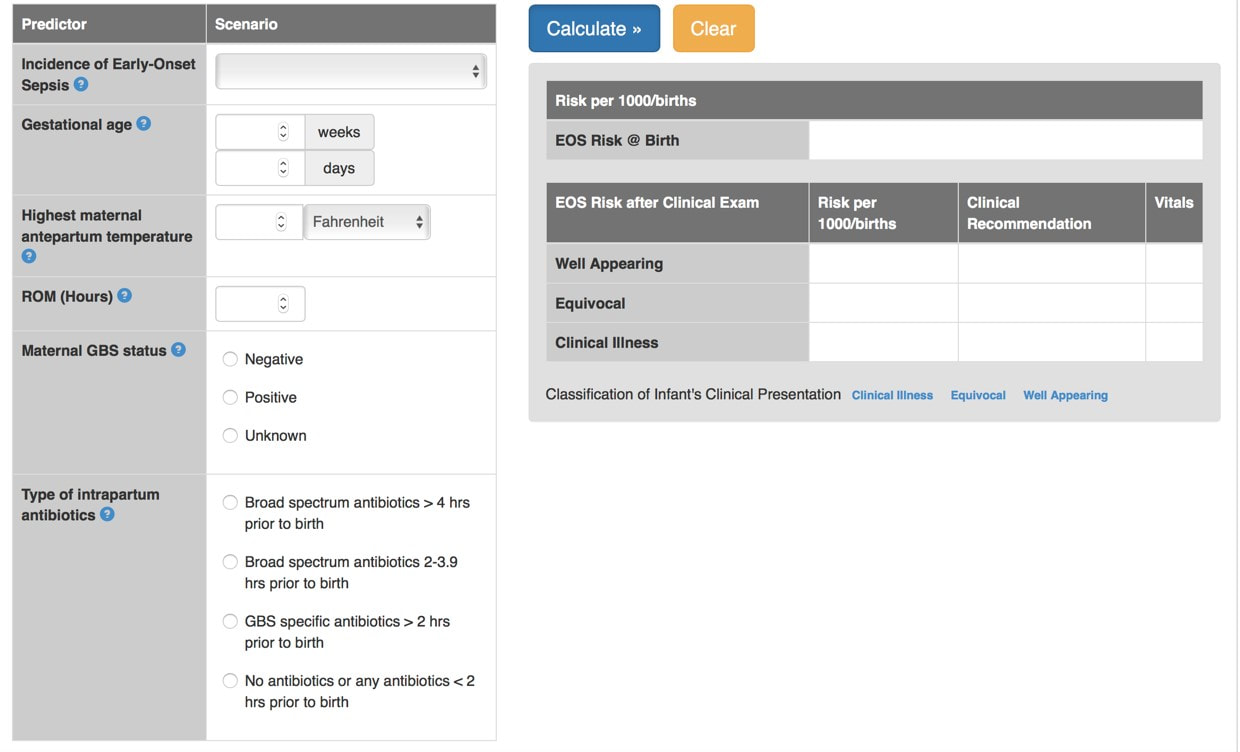
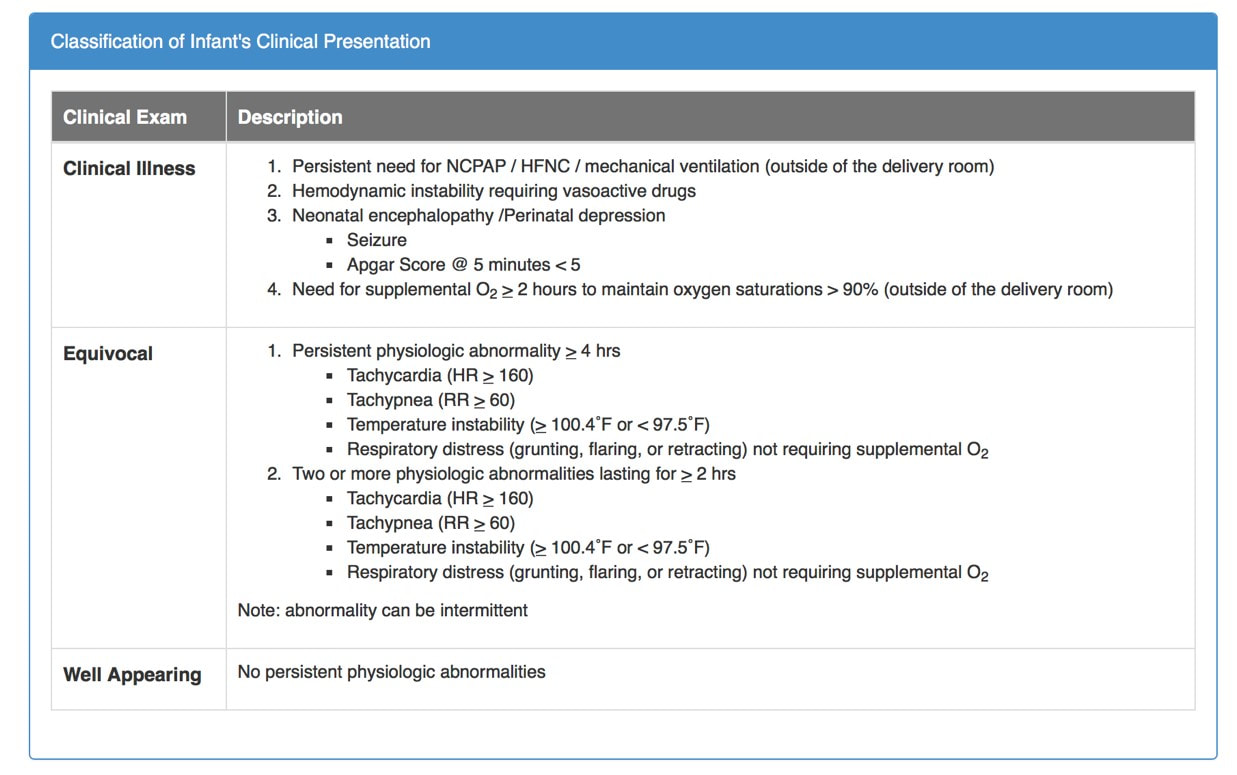
Dr Annabel Greenwood  Earlier this month I attended the Wales Neonatal Network Audit & QI Day and a hot topic for discussion was sepsis and the use of antibiotics. The sepsis risk calculator (SRC) is a fairly new concept due for implementation in neonatal units across Wales early next year…but what does it involve?! What is the sepsis risk calculator? The SRC was established by the Kaiser Permanente Health Group in Northern California, and has reduced antibiotic use in babies by almost 50%. It is a tool for calculating the risk of early-onset neonatal sepsis (EONS) in babies ³ 34/40 gestation. It uses maternal risk factors together with the clinical presentation of the baby to calculate a probability of EONS per 1000 babies. Why is it important? The incidence of EONS is 0.5-0.9/1000 live births in babies ³34/40 gestation, with a 3.5% incidence of mortality. Current guidelines for EONS are not sensitive or specific e.g. the definition of chorioamnionitis can vary, diagnostic tests have poor predictive value for EONS, and 40-50% of cases are not captured by current screening tools. Furthermore, current guidelines do not take into account the clinical examination of the baby. We have a duty as clinicians to improve antibiotic stewardship, avoid unnecessary investigations, and shorten duration of stay in hospital. The calculator in more detail… An initial probability of EONS is calculated based on the population incidence together with risk factors for sepsis including; gestational age, highest maternal antepartum temperature, GBS carriage status, duration of rupture of membranes, and the nature and timing of intrapartum antibiotic administration. The baseline risk is then modified based on the infant’s clinical examination Implementation of the Sepsis Risk Calculator… The calculator is not currently in use in neonatal units across Wales. However, following extensive discussion at the Wales Neonatal Network Audit & QI day, the provisional aim is for implementation early next year. It has already been implemented in some neonatal units across England (Plymouth, Exeter, Bath, Southampton, Oxford), with a reported 40-70% reduction in antibiotic use (depending on the centre So…what do you think? On reflection, after listening to the discussions at the Wales Neonatal Network Audit & QI day and exploring the topic further, I feel the implementation of a sepsis risk calculator on the neonatal and postnatal units is a positive move towards improving our antibiotic stewardship, protecting babies against unnecessary investigations, whilst at the same time easing the workload of the medical team by reducing unnecessary procedures. However, let’s not forget that neither the SRC or current guidelines will pick up unwell babies at birth…There is of course no substitute for clinical acumen!
0 Comments
30th October 2018, RCPCH London Dr Chris Course The RCPCH and the NIHR (National Institute for Health Research) held annual joint study day aimed at promoting and de-mystifying academic training careers. This free study day is fairly new on the RCPCH events calendar, having only been held for the past couple of years, but aims to tackle an area of training which is sometimes perceived as difficult to understand and undertake.
This was my first trip to RCPCH HQ in London, and it was great to actually see the place where its all run from. Despite not being as grand as the Royal College of Surgeons or GPs, it was a modern building with good meeting facilities. I was also a little worried that, not already been on an academic training pathway, I may be a little “out-of-it” or some of the subject matter may not be useful or attainable for me. Thankfully, I was wrong! There was a really good mix of trainees in attendance with a wide range of backgrounds. Some were already undertaking PhDs, some were nearing the end of their training and looking to build a research career, some were already on an academic training fellowship. Meeting all these colleagues with different backgrounds in the “Networking” session during the morning helped me to put my own current aspirations and difficulties into context and to being finding some solutions to these problems. The speakers for the day were an eminent bunch and gave some really useful and insightful talks. Professor Anne Greenough started the day with a broad introduction to academic career paths, and how the new progress curriculum is building research and academia into the training domains, aiming to improve our exposure to clinical research, as well as encouraging the Deaneries to facilitate more academic opportunities. Dr Chris Gale then gave his personal experience of his path into an academic career, giving a “how-to” guide too framing a research question, finding the supervisors and mentors to help develop your project and then how to find the grant money. It was encouraging to hear how perseverance is the key to obtaining the funding, and giving hope that somebody wold fund your project if you’ve had a good idea! The morning was rounded off by Professor Paul Dimitri trying to de-mystify the NIHR – not an easy task! It seems to be a very complex structure, and I can’t say I understand how they work completely, but I’ve definitely got a better idea of where to find more information now. There was also good formation on how to further an academic career as a trainee and consultant after completing your initial projects. The afternoon included workshops from Dr Lauren Kier from the Wellcome trust, covering tips on grant application writing and how to secure that all-important funding, and balancing clinical and academic priorities through your training grades. Following this, there was a presentation covering developing a career in industry, and leaving clinical medicine. I can’t say this talk filled me with inspiration, but it was a interesting to hear the experiences of life outside of clinical medicine with a medical degree. The day was a rounded off with an entertaining talk from Professor Mike Levin, giving an overview of “A journey into research with no plan”, and how an inquisitive mind and a bit of serendipity can help forge an academic career. I’m not sure if the much more structured and formalised training career we have now, with portfolio and ARCP demands, would still allow such a career path, but it was interesting all the same. I would recommend the Academic Trainees Day to anyone contemplating an academic training path or thinking about taking time out of training to do research. Also highlighted in the day was the RCPCH’s Academic Toolkit www.academictoolkit.org which is another useful resource for anyone wanting to know more about academic careers. The day highlighted the challenges and obstacles to an academic career, and how to start overcoming them, and was a good networking opportunity to learn of other peoples experiences. The day showed that an academic career can be a challenging one to start and maintain, but can be incredibly rewarding. Dr Rebecca Broomfield A summary of a year taken out of program to pursue an interest in clinical leadership.  During the last year I have spent my time as a Welsh Clinical Leadership Fellow. While we want to use this blog to promote research and education we also want to highlight opportunities that we have within Wales for trainees. The year as a Leadership Fellow was one of the hardest but most enjoyable of my career. I have blogged on here individually about some of the fantastic opportunities which I was able to attend. I encourage you to look up the posts on the Faculty of Medical Leadership and Management Leaders in Healthcare conference and the blog on the Neuroscience of Leadership course at MIT to name a few. In this summary post I want to give you an overview of why I think clinical leadership is so important and what this year involved Why do it? Is it even important? Leadership is everyone’s business. As you go through your career you will be but into leadership positions even if you don’t think that you are. Everybody within medicine is a leader in some way and therefore surely it is important to learn the skills to be a good one? We teach other things, procedures, history taking, interpretation of investigations so why not teach leadership? I believe there is some weight in the argument that leaders are born, not made in that some people will naturally gravitate to and thrive in leadership positions. But every leader can improve, and therefore good leadership can be taught. If as trainees we are given an opportunity to learn these skills then this can only be a good thing for the future of health care. The Faculty of Medical Leadership and Management Trainee steering group is a fantastic resource for trainees. (https://www.fmlm.ac.uk/about-us/networks-and-groups/trainee-steering-group). They have just published a toolkit which outlines the importance of clinical leadership more eloquently than I can summate in this paragraph. It offers hints and tips to expand your own leadership styles without having to take a year out like I did. This can be found here: https://www.fmlm.ac.uk/members/resources/leading-as-a-junior-doctor The Project When I started this year, I anticipated that the patient improvement project which I had selected to do would be the complete focus of my attention but actually this was a very small part of the lasting impression I have from this year. My project was based within the medical education department at Cardiff and Vale Health Board. I worked with the simulation team changing the way which we collected feedback from our simulation courses, helping with the development of a new simulation suite, designing and leading new simulation courses and co-ordinating a innovative in-situ simulation program to tackle falls. My supervisor Dr John Dunne was fantastic, alongside Miss Melanie Cotter they gave me freedom which I have not had in a structured training program to pursue my own interests and develop my project as we went along. Because of this I probably worked harder than I ever have, but also enjoyed work more than I ever did. My project actually became more of a tool in which to try out different leadership styles and the hints and tips we were learning as part of the PGCert in Leadership and management. It was successful and will leave a sustainable change within the medical education department. As fellows we were all encouraged to take steps to select a project that was outside our comfort zone. While I did have a previous interest in medical education and simulation I am a paediatrican and a lot of my work this year has been done within adult specialities. The projects which we had very varied and extremely different but all offered the same opportunities and similar enough experiences. The PGCert This is the qualification which runs throughout the Leadership Fellow year. It is run by Academi Wales through Trinity St David University. The course gives you a qualification at the end of the year and is a big difference in Wales when compared to the clinical leadership opportunities offered in England, Scotland and Northern Ireland. There were structured sessions spaced throughout the year which were attended by a wide variety of participants outside the fellowship program (clinical directors, speech and language directors and dentistry leaders to mention a few.) These focused on a variety of different areas within clinical leadership. Teaching different leadership styles, exploring coaching qualifications and self reflection with tools such as Myers-Briggs. The best session was the team building session in Elan Valley – again on this site there is a blog post dedicated to this experience. As a tip to this years Welsh Clinical Leadership Fellows – write your project up before you go back to clinical rotations! Right now, when I’m writing the essays, I wish I’d followed this advise from the year before me 😊 The Good I have been able to develop myself more in this year than in the whole of training so far. I have had the opportunity to analyse my behaviour looking at my preferences, understand when they might not be the best option and how to make them work for me. I have been taught the tools to look at difficult situations from different perspectives and recognise that not everybody thinks like me! – This in itself seems simple, obviously not everybody thinks the same but I was really able to explore just how different other peoples viewpoints were. By being able to see and appreciate these, not necessarily agree, you can avoid a great deal of conflict and confusion. Resulting in, as well as from, poor leadership. But I was also taught how to deal with conflict, how to turn challenge and opposition into a unifying aspect rather than a dividing one. I have learnt to ask for forgiveness, not permission and have been given the confidence to express my opinion. I have explored my own personality and learnt to look after myself. I hope to work in the emergency department and these skills will be invaluable as I go through my career to increase my emotional intelligence and resilience. The Bad It was HARD work. The first few months finding your feet and trying to work out what direction you wanted your project to go in were really difficult. As trainees we come from very structured environments, rotating from job to job, thinking in 6 month blocks and ticking off targets to pass the ARCP. This year was different, at the start there were no targets, you had to make and develop them yourself. You had to become used to managing your own diary. Not having to clock in and clock out was very liberating but also intense. As a group we handled this either by working every hour never really clocking off, in order to justify our time or by spending a while drifting around not really achieving much with he vast amount of time offered to us. This evened out in the end as we learnt the skills which came with the freedom. It was your responsibility to create opportunities rather than somebody handing them to you. And networking is a skill which can only be achieved through practise and comes easier to some than others. On a personal note, I was also away for large chucks of time from my family home. I have 2 small children aged 5 and 3 and part of this year was to have the flexibility to see them more frequently. I’m not sure I achieved that, being on a plane to Boston while my daughter was on stage at St David’s Hall in her first ballet show was a particular low point. (Thanks go to my Mum for stepping into that!) In Summary The pros far outweigh the cons. I have learnt so much more about who I am. What is good about my leadership style but also what I need to work on. My biggest learning point from this year is to respond not react, something that I didn’t even recognise I was doing until this year. I have had the opportunity to develop a long lasting quality improvement project, which is sustainable even after I have left my post. But I worked hard, I created my own opportunities and spent less time with my family than I would have liked. But ….. Would I do it all again? … Absolutely! If you are interested in applying for the Welsh Clinical Leadership Year and want me information please do contact me, I’d be more than happy to chat over coffee.
|
Editors
Dr Annabel Greenwood Categories
All
|








 RSS Feed
RSS Feed
