|
Dr Tom Cromarty Editor Interests: Paediatric Emergency Medicine, Medical Engagement and Leadership, Simulation, Quality Improvement, Research Twitter: @Tomcromarty |
Welsh Research and Education Network
WREN BlogHot topics in research and medical education, in Wales and beyond
Dr Celyn Kenny Editor Interests: Neonates, Neurodevelopment, Sepsis, Media and Broadcasting Twitter: @Celynkenny |
|
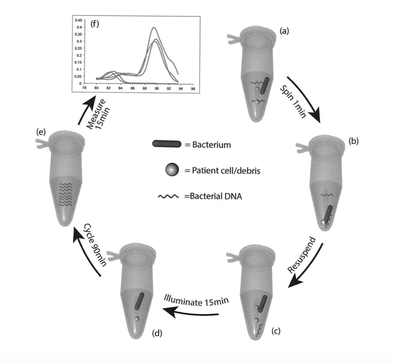
Annabel Greenwood ST4 As a Neonatal Registrar, it is not uncommon to be faced with the situation of an equivocal or borderline CSF result when testing for neonatal meningitis. Even when considered together with the clinical picture, it can often be difficult to interpret. Should the baby be started on antibiotics? And if so, for how long? A diagnostic conundrum. It was therefore an exciting prospect to hear that our Neonatal Unit was participating in the ‘PCRctic Study’ for the diagnosis of neonatal meningitis. But what exactly does this study involve I hear you cry?!... What is the PCRctic Study?A multi-centre prospective study designed to enhance the diagnostic accuracy of neonatal meningitis. Why is it important?Neonatal bacterial meningitis is a serious illness that can be fatal if not treated. Early diagnosis is key. However, the diagnosis of neonatal meningitis is often challenging, both clinically and microbiologically, resulting in uncertainty regarding antibiotic initiation and duration of treatment. The negative predictive value of bacterial culture is low and can be inaccurate in confidently excluding bacterial meningitis. What does it involve?"PCRctic" is a novel assay based on 16S rDNA PCR technology. It aims to detect a single intact bacterium whilst eliminating free DNA from dead and/or contaminating bacteria, therefore enhancing diagnostic accuracy, eliminating false positive results, in a rapid, cost-effective fashion. This new diagnostic assay could lead to reduced antibiotic use and hospital stay for many newborn babies tested for meningitis. How does it work in practice?CSF is collected in the standardised way. At least 5 drops are to be collected in each bottle; two of which are standard universal containers, and one an Eppnedorf tube. Parents are consented before inclusion into the study. The samples are then sent to the lab for further analysis…. What does the future hold?PCRctic has already shown promising results for the diagnosis of neonatal bacterial meningitis. The study is currently ongoing across a number of tertiary neonatal units in the UK. Such novel molecular techniques have the potential to replace bacterial culture and enhance our antibiotic stewardship. Want to learn more...'Multi-centre diagnostic accuracy study of PCRctic - a novel 16s rDNA PCR assay for exclusion of neonatal bacterial meningitis' Dr A Abelian, Betsi Cadwaladr University Health Board
0 Comments
Dr Roisin Begley, ST8 PEM I recently attended the RCPCH annual conference in Birmingham and to nobody’s surprise spent the Tuesday PM at the Association of Paediatric Emergency Medicine (APEM) session.
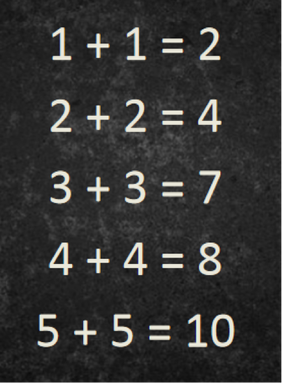
The key talks this year were themed on adolescents. These can be a particularly challenging group for us to cater for at times in the ED. The first speaker was Dr David James, PEM consultant in Southampton. He covered why adolescents are different and why we need to give them special considerations. Key messages were: new thinking/definition of adolescence is from 10-24 years. This has come from the paper in the lancet ‘The age of adolescence’ by Prof Susan M Sawyer et al. The adolescent brain is still developing and lots of the risky behaviours associated with adolescents can be attributed to this. Neuroscientists have shown ‘Evidence points to a dissociation between the relatively slow, linear development of impulse control and response inhibition during adolescence versus the nonlinear development of the reward system, which is often hyper-responsive to rewards in adolescence. This suggests that decision-making in adolescence may be particularly modulated by emotion and social factors, for example, when adolescents are with peers or in other affective (‘hot’) contexts’ (Decision Making in the Adolescent Brain, Sarah-Jayne Blakemore & Trevor W Robbins, 2012) So what is our role in this….. Dr James explains, as paediatrician’s we have a role to use the health encounters to identify risk-taking behaviour and perform psychological assessment: the HEADSS screening tool (Home, Education/employment, peer group Activities, Drugs, Sexuality, and Suicide/depression). The aim is then to signpost on to services locally for support. (ie drugs and alcohol, sexual health clinic, bullying services). Locally in Wessex they have developed an app to help with this. Web based version. iOS and Android on the way. Dr David James runs a RCEM day called the ‘forgotten tribe: adolescent in the emergency department’ if you want further insight. The second speaker was Dr Damien Wood, who explained his role in the eating disorder team in the Nottingham region. He was accompanied by Emily (an ex patient) who told us what it was like to life with an eating disorder and her experience of healthcare. She said ‘mental and physical health shouldn’t be seen as separate- it should just be health’. Emily recommended we all watch: Things Not To Say to someone with an eating disorder. The third speaker was Dr Annette Langseth, Consultant paediatrician at The CYP Haven. Her key messages were that we need to feel comfortable and confident talking to CYP (Children and Young People) about sex. If we feel uncomfortable or ‘judgey’ then they will not feel able to have conversations to us, disclose honest information or ask important questions. So get used to saying ‘vagina, anal and sex toys!' So lastly from me…. I missed this talk and seriously regret it. Dr Mike Farquhar gave a plenary talk on the Wednesday about his experience of growing up LBGT+ in the UK today, but you can get highlight of this issue through his twitter story: ‘ you can exhale now’ and by following him @DrMikeFarquhar and @RainbowNHSBadge. Key themes from this year’s annual conference were investing in the workforce and the future paediatrician with many plenaries and breakout sessions having a focus on staff wellbeing. Considering the ever increasing number of articles regarding dissatisfaction and junior doctor burnout, and the well-known case of Dr Bawa-Garba it was a pleasure to see the college taking on board the struggles of trainee wellbeing and taking the occasion to explore this further. It was an enjoyable experience to have the opportunity to listen to so many inspirational speakers and hear their experiences and to discuss the projects that they had been involved with. For the early risers, Tuesday morning began with a 5K run or a yoga session – I have to admit that I wasn’t there for either due to being on a train but I thought a nice session to include in the programme and begin the day with, and so I hear enjoyable. "Learning from Excellence"Dr Adrian Plunkett, Consultant Paediatric Intensivist in Birmingham, gave the initial plenary session on “Learning from Excellence” for what proved to be a highly motivational talk. He discussed how for so long the focus of health care has been avoiding harm and improving care, by learning from errors already made. He feels it is almost ingrained within us as part of our training to find the mistake, rather than focussing on the positive. He gave the example of a series of sums, and asked the audience what we saw: Honestly, what did you focus on first? The one wrong calculation, or the four that were correct? His take was that we should be taking the time to appreciate and reward excellence and hard work as a way to learn, rather than focussing on what an individual or organisation has done wrong. “Success has a much greater influence on the brain than failure” - Earl Miller (MIT Neuroscientist) Dr Plunkett wants us to ask ourselves, when regarding our peers and colleagues:
His group were the first to spearhead the emerging certificates of appreciation and now has a whole group focussed studying excellence in healthcare to help create new opportunities for learning and improving resilience and staff morale. For those interested www.learningfromexcellence.com and I believe a conference in the planning for February 2020. "The Cost of Caring"Dr Hilary Cass (previous RCPCH president) and Dr Caroline Elton (psychologist and author of “Also Human”) lead a stimulating seminar exploring how the traditional view of patient-centred care wasn’t enough, and more consideration needed to be given to the health professionals providing that care. The “Triple Aim” was an initiative designed to optimise health performance by focusing on (unsurprisingly) three aims - enhancing patient experience, improving population health, and reducing costs. BUT... It is increasingly felt that this is not enough and many organisations are now moving towards the “Quadruple Aim” with the fourth aim being the goal of improving the work life of health care providers. Dr Cass spoke about doctors, and particularly paediatricians being over-represented in those that access professional counselling services. Anecdotally, she describes paediatricians being at higher risk of stress, burnout and depression than some specialities but at lower risk of addiction to alcohol or drugs. Dr Elton discussed her book which many members of the audience had read and appreciated and then discussed her own practice, particularly focusing on career planning for doctors and helping doctors make the right decisions for them when trying to balance the work and lives. www.careerplanningfordoctorsanddentists.com "How does burnout affect patient care?"Dr Judith Johnson (psychologist) discussed causes of burnout and expressed what the majority of healthcare workers are feeling. Many causes of burnout were identified and discussed – excessive workload, low staffing levels, poor leadership, lack of support and lack of resources. These are known, accepted and still people have difficulty challenging that this isn’t right or appropriate. She gave the example of the Mid-Staffordshire inquiry “when staff are burnt-out terrible things can happen”. Burnt out and disengaged staff were present on all levels resulting in a catalogue of events and lack of care. "Wellbeing"Dr Dan Magnus (PED Consultant, Bristol) kicked off the trainees’ session with a lively discussion on wellbeing within medicine. Opening with a comparison between doctors and the crew of Apollo 13. I’ll admit I was slightly alarmed by this statement as I didn’t think things were that bad, only to realise later I’d mixed up Apollo 13 with the Challenger spacecraft disaster, and rather than our careers coming down in flames it was more – “Medicine you got a problem”.
Dr Magnus has done much work, particularly in ED, looking at the need for recovery after shifts and traumatic scenarios. Taking 10 minutes and having a cup of tea after a difficult event is not enough. He described working in Toronto where doctors don’t work more than 2 long day shifts or nights in a row (living the dream)! www.yougotthiswellness.com/ He describes three essential components of wellbeing within the NHS – belonging, competence and autonomy. Perhaps surprisingly he’s not particularly a fan of resilience training “encouraging doctors and medical staff to ‘be more resilient’ is just a crafty way of diverting attention from understaffed rotas and deteriorating working conditions in an effort to get individuals to be more accepting of clinical environments”. He highlights one of the main barriers to improving wellbeing as establishing what people want as every doctor or health professional will have a different take on what’s important to them. Saying that the general view is: better rotas, better facilities for rest and relaxation and more civility and kindness in the workplace”. He identified 5 key statements for improving wellbeing:
www.emtraineesassociation.co.uk/fatigue-shift-work--rotas http://www.emtraineesassociation.co.uk/rest Overall, an enjoyable conference with lots of food for thought!
This talk focused on Dr Rebeccah Slaters work on how noxious information is transmitted to the neonatal brain.
Her research focuses on how the brain behaves at rest and then differs with noxious activity with the aim of improving neonatal pain management. Throughout the discussion the speakers explored how to assess pain in neonates such as scoring systems and assessing facial expressions; although this is much harder in more preterm infants. Speakers then suggested possible analgesics such as sucrose, morphine, fentanyl or light touch. Dr Slater discussed her POPPI trial - which assessed if morphine was a suitable analgesic for ROP screening in infants however this trial was quickly stopped due to safety concerns. The rest of the discussion then focused on ethical issues surrounding pain management for example in patients with HIE, those requiring multiple and frequent blood tests or those having ROP. This series of talks demonstrated the difficulty in assessing neonatal pain but also the rapidly increasing knowledge and evidence. It did raise the question of which analgesic is best and when it is needed with ongoing evidence hopefully able to answer this more. |
Editors
Dr Annabel Greenwood Categories
All
|












 RSS Feed
RSS Feed
