|
Dr Tom Cromarty Editor Interests: Paediatric Emergency Medicine, Medical Engagement and Leadership, Simulation, Quality Improvement, Research Twitter: @Tomcromarty |
Welsh Research and Education Network
WREN BlogHot topics in research and medical education, in Wales and beyond
Dr Celyn Kenny Editor Interests: Neonates, Neurodevelopment, Sepsis, Media and Broadcasting Twitter: @Celynkenny |
|
Dr Annabel Greenwood ST5 When a flyer advertising the Welsh Paediatric Cardiovascular Network (WPCN) Autumn Meeting popped up in my inbox, I jumped at the chance to attend in the hope of broadening my (somewhat limited!) paediatric and neonatal cardiology knowledge. I’m sure many fellow trainees would agree with me when I say that the subspecialty of paediatric cardiology can at times feel a little overwhelming and complex, so any additional learning opportunities in this field are certainly invaluable. This year’s Autumn meeting was held at the Radisson Blu Hotel in the centre of Wales’ capital city, and was attended by a range of representatives from the paediatric multidisciplinary team with an interest in cardiology. The principal theme of the day was pulmonary artery hypertension (PAH), and the morning session was particularly neonatal-focussed, emphasising the relationship between prematurity and PAH. To set the scene, the day began with a case presentation of an ex-premature baby with chronic lung disease and a patent ductus arteriosus who subsequently developed PAH. Then followed a talk on cardiovascular outcomes in chronic lung disease (CLD) of prematurity. Professor Kotecha, Consultant Neonatologist at UHW, discussed the effects of CLD of prematurity on the left and right sides of the heart independently. With regards to the left-side of the heart, he considered the theory that those born prematurely will have higher systolic blood pressures later in life. This was based on the concept of arterial stiffness, and that prematurity and low birth weight are inversely related to arterial stiffness, and also that lung function is inversely related to development of arterial stiffness. However, he then went on to discuss the results of an ongoing respiratory study, the ‘RHINO’ Study, (Respiratory Health Outcomes in Neonates), whereby children aged 7-12 years, born prematurely at <34/40 gestation, were assessed in terms of their lung function, including spirometry measurement pre and post-bronchodilator therapy. The study found that there was no significant difference in peripheral systolic BP between those born prematurely with CLD, those born prematurely without CLD, and term controls. There was, however, a significant difference in peripheral diastolic pressure (higher in preterm CLD patients). This difference could perhaps be explained by measurement error or even steroid use. As for the right-side of the heart, pulmonary pressures increase in those born prematurely, but the key point to note is that by improving lung function and a child’s overall general health, then pulmonary pressures won’t be such a major issue. Dr Kevin Poon, Consultant Neonatologist at Royal Gwent Hospital then took us through the echocardiographic assessment of PA pressure. He highlighted the echocardiographic parameters used to assess PA pressures, and also surrogate markers of raised PA pressure. The following measurements can be used routinely to assess PA pressure:
These are measurements that I am on the whole unfamiliar with, given my limited exposure to performing echocardiograms, however, it was very useful to learn more…and of course, the key message was to ‘leave the fancy stuff’ to the cardiologists! After a brief refreshment break, Karina Parson-Simmonds, Children’s Cardiology Nurse Specialist at UHW, presented about the ‘6 Minute Walk Test.’ This is a test to determine the distance a person can walk at a constant, uninterrupted, unhurried pace in 6 minutes, and is widely used to assess exercise capacity of paediatric patients with CV disease. It can also be used to monitor disease progression, to evaluate patients’ exercise tolerance pre/post-operatively or to measure response to an intervention, and can provide longitudinal data for a patient if repeated at intervals over a period of time. It is not however ‘gold standard,’ as this remains the cardiopulmonary exercise test, and the BORG index score (rating of perceived exertion) is subjective, possibly causing discrepancy in results. Continuing with the multidisciplinary theme, Dr Lena Thia, Paediatric Respiratory Consultant at UHW, then discussed the respiratory management of the child with CLD and PAH. There are a number of respiratory causes of PAH, all associated with hypoxia;
Co-existing cardiac disease predisposes to developing PAH in CLD, and infants with Trisomy 21 with or without structural lung or heart disease are at increased risk of developing PAH. Key investigations to consider are;
With regards to optimising respiratory management;
The final session of the morning was an impromptu session by Dr Dirk Wilson, Consultant Cardiologist at UHW, as the planned speaker was unable to attend. This was a fantastic session on ECHO interpretation of common structural defects (ASD, VSD, AVSD), with the use of ECHO videos to enhance learning. Unfortunately due to on-call commitments, I was unable to stay for the afternoon session, however, Dr Maria Mendoza (Neonatal Clinical Fellow at UHW), has kindly provided us with a great summary… "The afternoon was a fun, interactive session amongst all participants of the meeting to culminate everything we learned during the day. Each table consisted of a multidisciplinary team of consultants, trainees, nurses or cardiac physiologists where a well-informed discussion was made possible. Different cases were presented and each team was able to analyse the case together, view the different imaging results available such as ECG, Chest X-ray and Echocardiogram findings and come up with a diagnosis and subsequent management. Some of the cases were Hypoplastic Left Heart Syndrome, Possible Noonan Syndrome with Pulmonary Stenosis, Atrial Septal Defect and Hypertrophic Cardiomyopathy. We also discussed the risk of acquiring RSV especially during the winter season and which babies are at risk and need RSV prophylaxis. Overall, it was a very high-yield discussion of different clinical cases with many learning points." So in summary... What was good about it?
What was not so good?
Would I recommend?
Date for the diary….
2 Comments
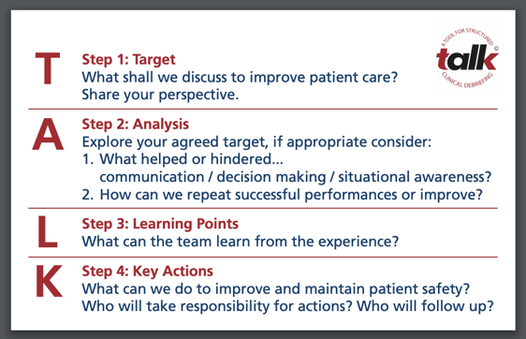
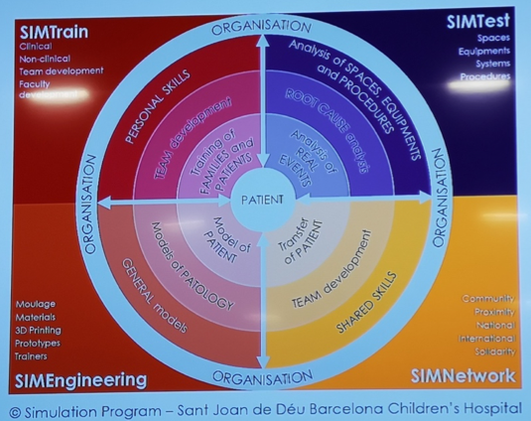
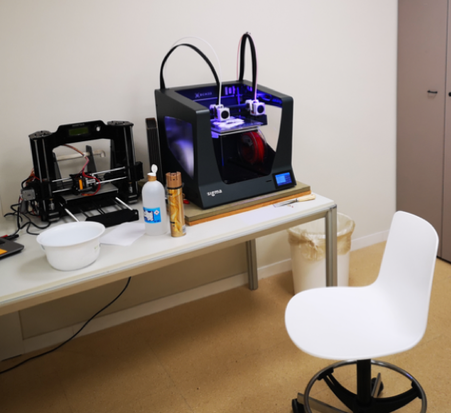
 Dr Tom Cromarty ST6 An experience at Sant Joan De Déu hospital in Barcelona Earlier this month I travelled to Barcelona with the EU funded TALK Debrief research project. This is part of the Research and Innovation Staff Exchange (RISE) programme, where Medical staff from Cardiff (Wales), Barcelona (Spain) and Stavanger (Norway) visit each other’s hospitals to learn and help with the implementation with TALK debrief, as well as experiencing other healthcare systems. TALK is designed to guide structured team self-debriefing after any learning event in clinical environments. The Structure can be seen in the figure below, with more information and FREE resources are available at TALKdebreif.org Whilst on my latest placement in Barcelona, I was able to attend the only specific Children’s Hospital in Barcelona called Sant Joan de Déu (SJD). This large tertiary referral hospital is mostly public funded and is going through a series of renovations. I was fortunate enough to visit the brand new PICU which in Spanish is called the Pediatric UCI (Unidad de Cuidados Intensivos), and experience the innovative Simulation centre. I was particularly impressed with the Simulation team which was created and lead by José María Quintillà Martínez. Over the past 15 years he has been incredibly passionate about simulation in healthcare, starting off with a very low fidelity mannequin and no support, to now having an integrated simulation service. José and his team were incredibly enthusiastic about Simulation, ensuring that the focus stays on the intended output and the methodology, rather than the expensive shiny technology. After developing a relationship with the world leading Boston Children’s Hospital Simulator programme, José and his team have developed a Simulation service that has the backing of the hospital board and is fully integrated with the hospital, rather than a stand-alone medical education tool. Other than Simulation courses, which they run on >150 days of the year, the majority of the time for hospital staff, the team was recently involved with the architectural planning of the new PICU. Having created a mock bed space in the Simulation centre, they replicated the clinical scenarios which would need the most people and equipment, such as an unwell patient requiring ECMO (Extra Corporeal Membrane Oxygenation) or Dialysis. They modified the design and size of the room, from the location of sinks, equipment & monitors, to establish the optimum environment with the floorspace available. Once the ward renovations had been finished, they again brought in the Simulation team to practice common procedures and daily routines. This meant that the teething issues which inevitably come up, were corrected without a patient in sight or put at risk. This forms part of the SIMTest function of their integrated Simulation Program which can be seen below. SIMTrain is the traditional work of Simulation in Healthcare, however the team in SJD aim to develop personal and team skills, as well as training patients and families. Trainers from the Boston Simulation programme visit the hospital to train a multidisciplinary group (Doctors, Nurses and Physios), forming a core Simulation faculty who can practice and train others in their departments. The PICU had five nurses and five doctors trained up, who would run a two-hour scenario on three occasions every Thursday. The simulation philosophy is so embedded, that any new department being renovated (including PICU and NICU) has a separate ‘Simulation’ room (see below), specifically reserved and always ready for use. This also enables teams to put rented equipment and new protocols to the test before investing in them and practicing on patients. Permanent Simulation room on the PICU unit José’s team have used the Kerr-Patrick education model to validate learning from Simulation, currently working on levels 3 and 4 to demonstrate changes in behaviour and patient outcomes. The backing they receive from the organisations leaders has enabled them to hire an innovation team, subsequently creating the 3D4H (3D for health) unit. After a complicated oncological surgery was abandoned due to the challenging anatomy, the team used imaging to create a 3D version of the patient’s head. This meant the surgical team could make an accurate surgical plan and even practice the surgery as many times as possible. By saving money on theatre and anaesthetic time, this method saves time, money and makes the procedure safer for the patients. As the specialist centre for MPS (Mucopolysaccharidosis) in Spain, they receive many referrals for management and perform up to fifteen maxilla reconstructive surgeries per year. These patients have complicated upper airway anatomy, making the intubation difficult. 3D4H printed a number of typical MPS heads with accurate upper airway anatomy and put this onto a traditional high-fidelity mannequin for simulations. This enabled anaesthetists to practice this complicated skill a number of times, demonstrating their proficiency before the patient had even arrived. The 3D4H team have developed been used in a number of other ways.
Simple 3D printer Trachy and various skins printed from 3D4H team Integrated Simulation is a new way of designing and improving medical environments, teams and the care they provide, by exploring and learning from reality before it happens! I was completely inspired by the number of functions which their Simulation team performed as an integrated service with the hospital, and the incredible number of cost-effective uses for 3D printing. 3D printing is being used more and more in medicine, with the materials becoming cheaper and technical printing skills advancing every year.
How could you use Simulation or 3D Printing where you work? Perhaps Barack can inspire you? Davide Paccagnella, ST3 Paediatric Trainee When I attended the 4th Annual Paediatric Medication Error Prevention (PMEP) Study day (which took place in Morriston Hospital, on 8th October 2019), I already knew that it was going to be a great experience! For the past four years, Morriston has achieved great results in the field of medication error reduction and prevention. They have done this by forming a revolutionary tripartite alliance between Paediatrics, Nursing and Pharmacology. It all makes sense – by nature, prescribing, administering, checking and supplying medication is a multi-disciplinary exercise, and improving the safety of these processes can only be achieved by working together across different specialties. This annual study day has become increasingly popular, year after year, with almost 100 registered attenders this time around. Which meant that, on the day, the lecture theatre was nearly full, making me feel like I was attending a national conference as opposed to a local study day! The morning was kick-started by Professor Philip Routledge, CBE, from the All Wales Therapeutics and Toxicology Centre. His keynote address provided us with a global perspective on drug manufacturing, testing and marketing. When it comes to prescribing, I did not know that the largest avoidable cost, worldwide, is non-adherence to prescribed medication! Prof. Routledge also highlighted important steps (often taken as a result of tragedy) that helped make drugs safer over the course of time. Some of these stories were very moving and sobering. Overall, it was a brilliant lecture, and I’m certainly hoping that Prof. Routledge will consider returning to Swansea to inspire us all, again, next year. We were privileged to have Alana Adams, Principal Pharmacist from the Welsh Medicines Information Centre, and Dr Alison Thomas, Medical Director of YCC Wales, who came to give us an overview of the Yellow Card Scheme. Perhaps unsurprisingly, it turned out that not many audience members had filled a Yellow Card out before – this lecture was therefore a necessary reminder of just how important it is to provide this information, and what reactions need to be reported. Judith Morgan, Interim Acute Care and Leadership Adviser from the Royal College of Nursing, talked about the “Swampy low lands of Practice” when managing medicines. It was a collection of striking examples of mismanagement, and highlighted the fact that even the most experienced healthcare professionals can make mistakes under time- and workload pressure. In the afternoon, we took part in a number of workshops, aimed at equipping us with the necessary skills to recognise, learn from, and take steps to avoid errors. I found all workshops useful, but I particularly enjoyed two: firstly, the one focusing on “change in action”, which highlighted the “power of habit” and made me realise just how difficult it can be to achieve a sustained change. The “seven steps” to deliver change were discussed, and thanks to the interactive nature of this session, I felt I could learn a great deal from colleagues. Secondly, the workshop focusing on personal reflections was particularly eye-opening as real-life events were discussed by the individuals directly involved – this led to a stimulating discussion, and some take-home messages we could all embrace. In summary, this study day was a great opportunity to reflect, learn, and network with colleagues from different specialties, working across Wales. I’d like to thank the founders of the tripartite alliance, Dr Pramodh Vallabhaneni, Rachel Issac, and Bhavee Patel, for their ongoing ground-breaking work in the field of medication errors prevention, and for organising such an inspirational event! |
Editors
Dr Annabel Greenwood Categories
All
|










 RSS Feed
RSS Feed
