|
Dr Tom Cromarty Editor Interests: Paediatric Emergency Medicine, Medical Engagement and Leadership, Simulation, Quality Improvement, Research Twitter: @Tomcromarty |
Welsh Research and Education Network
WREN BlogHot topics in research and medical education, in Wales and beyond
Dr Celyn Kenny Editor Interests: Neonates, Neurodevelopment, Sepsis, Media and Broadcasting Twitter: @Celynkenny |
|
Mike Bailey IT Director, Cardiff and Vale University Health Board  Cardiff and Vale have recently purchased the Patients Know Best patient portal (PKB). PKB is licensed such that any patient of Cardiff and Vale UHB secondary and tertiary services can use it. Primary care is licensed separately, and that cost is under consideration. Mike Bailey: PKB is presented as a website, accessible from any patient devices that feature one of the common internet browsers (PC, laptop, tablet, phone) and is responsive, even where there is a low signal strength. PKB addresses a number of our strategic priorities. We are committed to “Information for You” and as such, PKB will provide patients with access to as much of their clinical data as possible. This will include (past and current) diagnosis, meds, care plans, live results, appointments, letters, images, reports. This should mean that patients will genuinely want to use PKB and positively support patient sign-up rates. There are also a number of operational gain that PKB will facilitate: · Empower the Person. Through various functionality, including online care plans that can be shared with the patient’s care network, support the patients in taking an increased ownership and role in their care. · Facilitate significant elements of service redesign. Including community-based services. Self-reporting, for instance, will enable a significant reduction in outpatient attendance. The capacity freed up in outpatients can be directed to further improvements such as early, supported discharge, with an open ticket back to the ward if becomes necessary. · Facilitate operational savings (time/resource/cost). Very similar activity within Sussex & Surrey IBD process, reduced priority admission waiting time from 6 weeks to 1 week. Reduced admissions (average 5 day stay) by 90% and reduced surgery by 80%. Cheaper medications were also utilised as condition did not reach the same level of severity. · Home First. In addition to early supported discharge, PKB will facilitate the use of online questions and telephone/video conferencing to reduce the need for patients to attend site. · Outcomes that matter to people. Trials within CAV Audiology have demonstrated that when patients are able to complete pre-clinic questionnaires at home, in their own time, the response are much more meaningful and hence enable improved focus on the required care and support. By facilitating a fully informed consent, patients are able to fully understand post treatment impact and actively make a decision on the pathway that suits their needs. This significantly reduced DNAs at the outset of treatment and at the latter stages, when patients fully realise the pending impact on an impending procedure. · Reducing health inequalities. ENT and Audiology have demonstrated that the time saved via unnecessary appointments and improved processes has allowed specialist nurses to target those, often elderly and isolated patients, which have disengaged from their services. PKB also enables patients to delegate access to their records within PKB to their circle of care, thus enabling increased support, through better informed carers - who can see appointments, care plans, letters, meds, help to self-report etc. · Compliance. ENT and Audiology have confirmed that issuing compliance related questionnaires and surveys via PKB has resulted in a significantly higher return rate. · Prehabilitation. PKB can automatically receive and display data from smartwatches and related apps, in order to, with the patients’ permission, track exercise, diet and sleep, as part of prehabilitation programme or just general wellbeing. · Provide cashable savings (letters). Letters to patients will be accessible within PKB, rather than via traditional postage. This is much cheaper than current methods. Even if a patient does not open a letter, it can be rerouted to an outsourced provider, which will send a paper letter cheaper than can be produced internally within CAV. There are many other benefits, specific to each specialty. Initial rollouts will include Gastro, ENT and Audiology. ENT and Audiology already have PKB but, now that we have purchased a full license, we will now be integrating PKB with UHB and NWIS systems to full enable the above benefits. Whilst we await the completion of the integration work, we are also launching PKB for the national Talipes service. This will launch during May 2019, before integration is available but will provide a significant improvement over the current paper-based data collection process Aurey Tong: Whilst we await the completion of the integration work, we are also developing PKB for the Cardiff and Vale Talipes service. This is for parents whose children have congenital talipes equinovarus. The aim is to empower parents via information and support. They will have an electronic version of the talipes passport, a library of resources including top tips, and the opportunity to support each other.
0 Comments
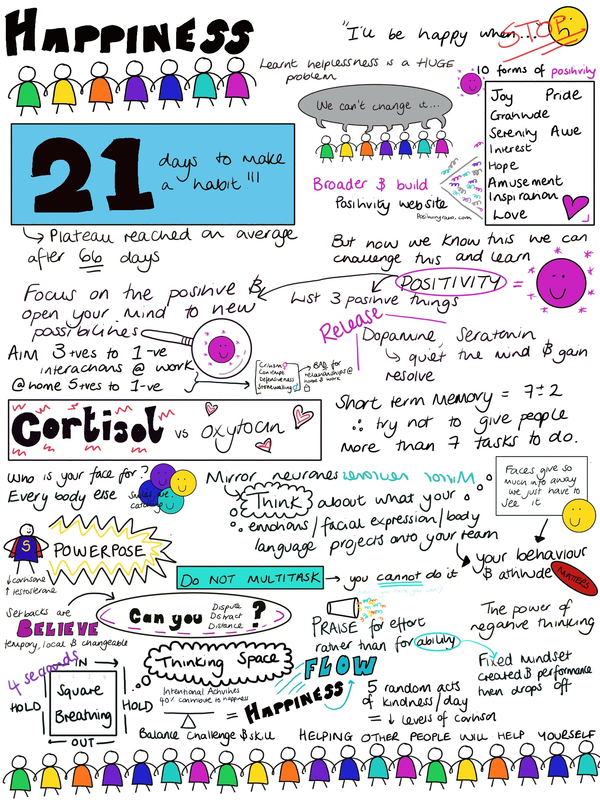
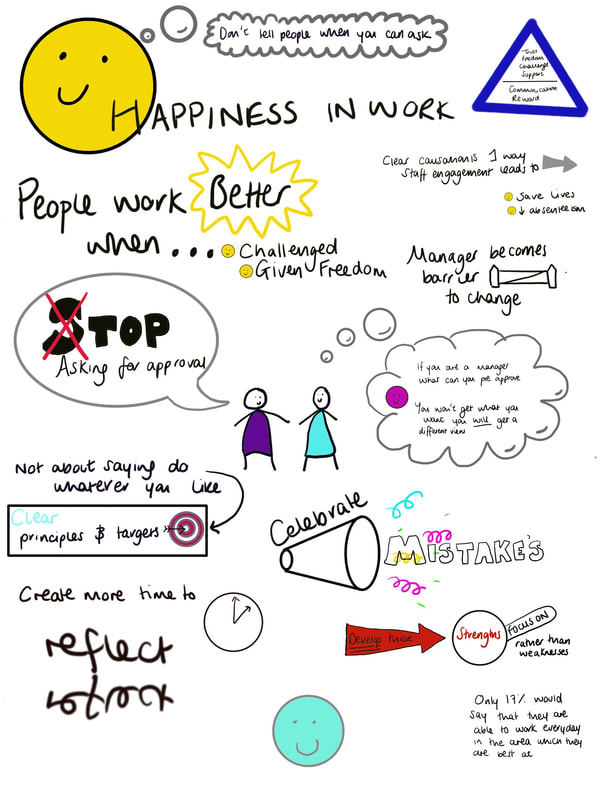
Dr Rebecca Broomfield Why is it important? The environment created in the workplace is vitally important to the wellbeing of the staff who work there. In clinical medicine this also translates into the wellbeing of patients and ultimately their safety. So what can you do, as a leader, to ensure that your workplace environment is as positive and functional as it could be? This topic was first visited during the Faculty of Medical Leadership and Management (FMLM) conference in Liverpool and covered in the Leadership blog in December. It was covered here by Henry Stewart. He runs the Happy company, which has been listed as one of the 20 best workplaces in the UK for five successive years (www.happy.co.uk). Henry Stewart has also written “The Happy Manifesto” He has identified that people work better when they are challenged and given freedom. As a manager we should be enabling people to innovate, and rather than focusing on weaknesses we should develop our strengths. Mistakes should be celebrated and, within the boundaries of clear principles and targets, team members should be given freedom and ownership of projects. The topic has come up time and time again within the Leadership program I am currently enrolled on. Happier workplaces function better, lead to greater innovation and better results. What can you do? Within a quality improvement program provided by Cardiff and Vale Health board, we recieved a afternoon workshop to discover how we can use positive psychology to improve our own happiness and that of our workplace. This was delivered by Mark Hodder. People tend to currently live with the mindset "I will be happy when....I've lost weight/I have a promotion/I own a bigger house" Thus success creates happiness. Rather than this way of looking at happiness what would happen if we looked at it from the opposite direction, shifting our paradigm and focusing on happiness bringing success? Learnt helplessness is a huge problem, but now we know this we can challenge this and learn positivity. When driving home from work try thinking of 3 positive things which happened that day. They don't have to be big things, just build it into your daily routinue. In work in order to build positive relationships we need 3 positive interactions to every negative one. Can you within your workplace build in positive feedback or interactions. How often do you praise people or say thank you? Could you do this more? Think about how you motivate your team. For praise to be most beneficial it should be given for effort rather than ability. By praising for ability you run the risk of creating a fixed mindset which then has the potential to cause a drop off in performance. Effort and recognising hard work by saying "Thank you" or "I can see you have put a lot of work into ..." A growth mindset is created promoting positivity and providing motivation. When you encounter a problem or a difficulty could you Dispute, Distract, Distance? This technique creates a mindset that setbacks are tempory, local and changeable rather than spiralling into a negative perspective or allowing negative feelings to dominate a workplace. Problems are actively dealt with. What about your face? Consider who your face is for? .... (clue it's not for you!) Your face and body language are ways of communicating to other people. Faces have so much to give away we just have to focus on them and see it. In the same way, we need to be aware of what our face is saying about us and how we can use this to our advantage - smiling is contagious! When we are interacting with people often their facial expressions and body language mirror our own, therefore our behaviour and attitude matters. Think about what your daily facial expressions project about your emptions onto your team. And finally ..... helping other people will help you. 5 random acts of kindness a day have been shown to reduce cortisol levels and thus reduce stress, see how many you can build into your day. Further reading: The Happy Manifesto: Make Your Organiszation a Great Workplace By Henry Stewart
The Chimp Paradox: The Mind Management Programme to Help You Achieve Sucess, Confidence and Happiness By Prof Steve Peters http://www.markhodder.net/ - Links to articles from the workshops and contact details for Mark Hodder. Dr Rebecca Broomfield Photo credits to Dr Sara Long, Dr Kathryn James, Dr Laura Potts Leadership course run in MIT Boston USA As Clinical Leadership Fellows we were privileged to have the opportunity to attend a Leadership Course at Massachusetts Institute of Technology. 5 of us hopped on a plane at the end of March and flew over to Boston in order to attend Applied Neuroscience: Unleashing Brain Power for You and Your People We flew in the day before the course and in true tourist fashion made the most of the first day getting over jet lag before the course began. None of us had been to Boston before and despite venturing out to an Irish bar with live music on our arrival we were all up bright and early on the Monday morning. (Thanks jet lag!) We grabbed our lonely planet guides and re-embraced our travelling student identities to explore a fantastic city. We spent the day following the Freedom Trail - Boston has a very limited history but what it does have it exploits amazingly! The trail lead us through the start of the American Independence and British invasion. We stopped off in the harbour at lunch time and took a (freezing cold!) boat trip too see all the islands. We continued our trail and then extended it to include a viewing of the bronze duck statues in the main park. We watched the sunset in the tallest building in Boston with cocktails that were stronger than they tasted! Day 1 The course was facilitated by Dr Tara Swart (@TaraSwart) She holds a BSc in Biomedical Science and PhD in Neuropharmacology from Kings college London. She read Medicine at Oxford University gaining a BM BcH qualification. She is an executive coach and is passionate about disseminating simple, pragmatic neuroscience-based messages that change the way people work. This course was not aimed at medics, and I do feel that we would have benefited from a slightly more rigorous focus on the scientific evidence for some of the science taught on the course, however, this was not it's aim and in fact may have alienated some of the audience who were present. Having looked into the evidence presented since the course, there is a significant scientific knowledge base behind the methods taught. There has never been a room where, as a medic, Imposter Syndrome has a more appropriate setting. The course was full of chief executives and people who have multi-million pound contracts in their back pockets and more staff working underneath them imagined possible! However, the problems encountered and the neuroscience to increase behaviors and lead change were relevant to both the medical and the commercial setting. The insight which mixing with leaders from completely different worlds to our own has allowed us to gain was worth attending the course alone. Right from the word go this course was structured differently to the majority. We sat on circular tables with 4-5 other delegates but at the back of the room were juggling balls, skipping ropes and standing desks. There were refreshments available through the whole day (although, caffeine was removed at 14:00 - it reduces your sleep quality after this time) and at the start we were actively encouraged to access refreshment as needed and walk around the classroom freely. While the skipping only occurred in the breaks some people did take advantage of the juggling balls and juggled at points throughout the teaching. While we learnt on the course that social safety is the area of culture in the workplace and wellbeing which has the biggest impact on the brain the next biggest area is physical activity. By standing up and engaging in a physical activity such as skipping or juggling we were actively engaging our brains and increasing our neuroplasticity, which is the brain's ability to reorganize itself by forming new neural connections throughout life. Brains tend to hold onto old pathways, in order to create new pathways you need to rest, fuel, hydrate and oxygenate your brain. by exercising you increase the release of brain derived neurotrophic factors (BDNF) which helps with the formation of new pathways. Neuroplasticity is an important concern when thinking about the neuroscience of leadership. We do not unlearn habits or behaviour, this is not possible but we are able to overwrite these pathways. Translated for use in leadership this could be as simple as giving people an alternative option rather than simply managing an undesirable or ineffective behaviour by saying "don't do that". Making new neural connections for behaviour is tough, but it is the first time which requires the most effort. As you repeat the same pattern of behaviour you strengthen this pathway and therefore make it more automatic. There are 2 areas of the brain involved with learning new behaviours; the cortex - which is learning by instruction and the limbic system which is learning by experience. Knowledge/organisation of reality happens in the pre-frontal cortex but feeling and managing anxiety is under the control of the limbic system. A brain stem reflex is often change preventing within behaviour modification. Logic is not enough in order to modify behaviour and promote change you need to connect the 2 systems. How can we use neuroscience to our advantage in the workplace? The top 7 emotional drivers within the workplace are:
Communication is one key area where neuroscience can give us the edge over others. Using your limbic system to promote bonding and enhance the emotions above can give you an edge in leadership. Trust is the number 1 emotion but trust uses more resources than mistrust, and is therefore more difficult to employ. Can you use neuroscience to create a better bond and increase trust? Yes, and it's as simple as eye contact. When you next communicate face to face with somebody try actively looking with your right eye into their left eye. This will activate their right limbic system which has been shown to create a strong bond. A bond enables colleges to feel more valued and creates a better working culture and environment. I've been trying this out since I returned and I feel that it has enabled me to shortcut some relationship building and create a quicker more valuable relationship. As far as I know, nobody has thought I've been looking at them strangely or even been aware that I am trying out this technique so even if it initially feels awkward for you it's worth a try! Face to face communication is always better, so make the effort to do this when possible. The role of stress .... The right ventral lateral pre frontal cortex is active in stress and has a role in regulating emotions. This area responds to pain - notably physical pain causes the release of natural painkillers whereas psychological pain does not, it also contains cortisol receptors. Cortisol is a fight or flight response hormone. It has a natural morning spike and then maintains low levels throughout the day accept in crisis or when there is a threat to survival. Having too much cortisol can lead to physical manifestations from yourself or the team which you are leading. These include poor sleep, irritability and craving chocolate/caffeine. The physical symptoms can detract from your brain power and demand attention, too much cortisol can also decrease your immunity and increase your abdominal fat thus impacting your physical health. Emotion biases all decisions and stress/fear biases decisions to the emotional system through the cortisol pathways. Interestingly some studies have shown that cortisol levels can be transmitted to others in a similar way to pheromones. Therefore a leader who has high levels of cortisone has the potential to expose others to them as well as themselves. Stress is just one of the recognised threats to your brain power in work, others include uncertainty and uncontrollability. As a leader you do have the power to influence these for your team. Can you adapt your leadership in order to make your team feel more in control of the tasks which they are performing? You can definitely reduce uncertainty. We did a good exercise on the course which focused on re-framing our responses. As a leader when a suggestion is made by a member of your team the automatic response is to say "No". In order to say yes it requires more mental energy as a leader but improving your ability to this can increase the level of control which your team feel they have and promote the positive emotional drivers outlined above. We were tasked in pairs of making a suggestion to overcome a problem to our partner. Initially they had to respond with "No" Then we had to re-ask the question and they had to a respond with "Yes, but .." thus entertaining the idea but outlining the potential barriers stopping this from happening. As the questioner we than had to once again make the same suggestion but our partner needed to respond with "Yes, and..." Using "Yes, and .." reduces the social isolation of your team and increases the attachment and bonding created. Oxytocin, which is released when creating a good bond, shapes the neutral circuitry of trust adaption. Reward and attachment emotions regulate emotion and improve decision making. Thus by utilising this type of leadership within your team you can promote good decision making and reduce stress. There is lots to gain A 10% improvement in performance is equivalent to an extra 23 working days annually. Other key points from day 1
During the course all food was provided and the menu was created to promote healthy eating and ensure that the nutrients provided promoted brain agility. It was followed up with an evening reception - I'm not sure where the wine fits into a healthy lifestyle but it was definitely welcome after all the information provided during the course. Our thanks also have to go to Mr William Fleming, a fellow course participant who took us out to sample the local seafood in the evening, but also allowed us to pick his corporate brain with ideas that could benefit our leadership styles and leadership within the NHS. (I think/hope he learnt a little bit from us too!) Day 2 During day 1 we were taught that people are 15% more productive on the days that they do 30 minutes of aerobic exercise in the morning. While i'm not sure this counts as aerobic exercise, we took this on board and as a group of Clinical Fellows all attended the precourse early morning yoga session. The picture above is the view from the glass walled classroom we were practicing in, this rivals the morning session of beach yoga I took part in while travelling for the most breathtaking yoga view. It was a calming start to the day, followed by a breakfast of foods, as yesterday specifically selected to enhance wellbeing and increase brain agility. We were more focused on day 2 on our own strengths and weaknesses and what we can do to improve our leadership while increasing our own resilience and mental toughness. If we can maintain our mental toughness and resilience as leaders then we promote a culture within our organisation that it is important to do the same. "Nobody would get into a car without filling it up or maintaining it - Why do we not do this with ourselves?" Maximise your potential Prior to the course we completed a Neurozone questionnaire. This is a detailed questionnaire which enables you to focus on small changes you can make to maximise your own potential and therefore improve your leadership. Two of my areas for focus are improving my sleep and increasing the diversity of my exercise. Both of these require a small change but have the potential to have a big impact on my reserves. Culture Culture and patterns of behaviour and beliefs frequently impact perception, cognition and actions. You have a responsibility as a leader to use your skills to create a culture where your team members thrive. Your actions as a leader speak louder than the word which you use. My take home messages ...
What am I doing differently since the course?
Further reading: “Neuroscience for Leadership: Harnessing the Brain Gain Advantage” Tara Swart, Kitty Chisholm & Paul Brown We had a day to play with before flying home, part of my year is focusing on simulation and medical education. Therefore I took advantage of being in Boston to visit the 'Centre for Medical Simulation' which has a worldwide reputation. There was a course going on that day and so I got to see their sim suite in action and speak to their faculty. It was very interesting to note that they are also focusing on the educational value of simulation and how we can evidence this. Their facilities are excellent and it was exciting to be able to spend a short time there.
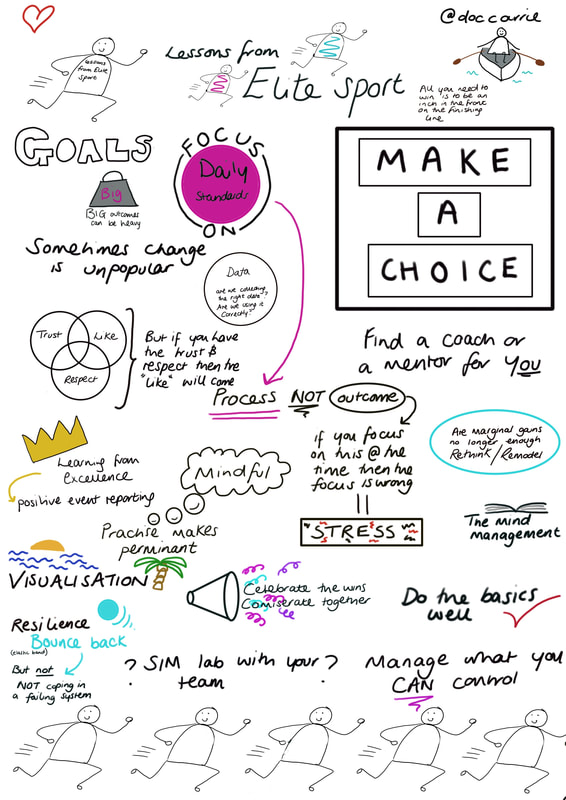
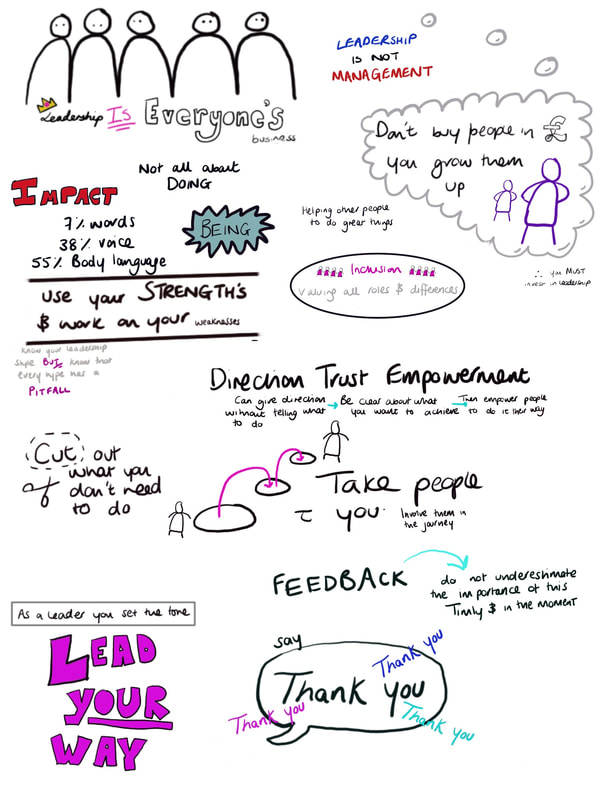
The afternoon was spent at the Boston Tea Party museum learning about leaders who promoted a change by making a stand - very relevant to the topics which we had been covering, and yet another leadership perspective. Boston was fantastic, I would recommend it as a city break. The course was an amazing opportunity to understand some of the rational behind current leadership techniques and put a neuroscience basis to their implementation. I have a lot of areas to work on to maximise my own leadership potential and am looking forward to trialling these out over the coming years. Leaders in Healthcare Conference 30th October – 1st November 2017, ACC Liverpool By Rebecca Broomfield I am currently taking a year out from the Paediatric training program and doing a Clinical Leadership Fellows placement through the Wales deanery. As a part of this year we come under the umbrella of the Faculty of Medical Leadership and Management (FMLM), it was under this disguise we managed to sneak ourselves into the FMLM’s annual conference "Leaders in Healthcare". I went to this conference with an initially pessimistic outlook. I truly believed that a lot of the information provided would be over my head, in a language that I didn’t understand, from managers who were slightly out of touch. I am humble enough to eat my own thoughts and I would thoroughly recommend everybody tries to attend an FMLM conference at some point in their career, indulge me and read on to discover why! As per conference structure, which I am becoming more and more familiar with, Day 1 began with a welcome – another choir, (starting to think this is a new trend .... perhaps someone could do a study?) followed by a Key note speaker. Seriously, this was an impressive start. We heard from Nicky Moffat in a keynote entitled “Leadership is everyone’s business” Nicky Moffat has a background in the military and spoke about the importance of not buying in people for leadership roles but investing in people and growing them up from within. She voiced an important message of inclusion; that every person has a role to play, as a leader your role is to value these differences and figure out how to make them work. You do not have to be able to do everything, but you do have a responsibility to those who you lead to dedicate time to your own personal development. You set the tone, so make sure that you lead your way. She was inspirational to listen to and it was particularly interesting to hear from somebody whose career was outside of medicine but was experienced in a structured, high-pressured environment. After a brief pause for coffee, we split into smaller group sessions. I went for a workshop entitled “Joy in work”. It was run by Henry Stewart, a man who introduced himself as “Chief happiness officer”, which I love, who wouldn’t want that to be their job title??! He runs the Happy company, which has been listed as one of the 20 best workplaces in the UK for five successive years (www.happy.co.uk). Henry Stewart has also written “The Happy Manifesto” a book that has made it onto my Christmas wish list (along with many others from this conference alone.) The company motto is “Don’t tell when you can ask” He has identified that people work better when they are challenged and given freedom. As a manager we should be enabling people to innovate, and rather than focusing on weaknesses we should develop our strengths. Mistakes should be celebrated and, within the boundaries of clear principles and targets, team members should be given freedom and ownership of projects. The style of the session was relaxed, he actively encouraged participation, and provided a significantly different perspective on workplace than my experience of the NHS. Lunch provided an opportunity to network with other conference attendees. There was a wide range of people present, many with backgrounds in significant leadership positions within the NHS. My after lunch session focused on collaboration across barriers and introduced me to the concept of Compassionate Leadership, which will be a blog post for the future. I didn’t want to stick to hearing from people with leadership roles within the NHS, so I headed to a second afternoon session delivered by Carrie Thomas, who herself is an ST4 in emergency medicine, but was delivering a session on how we can learn lessons from elite sport. She directed the audience to focus on the daily standards, looking at the processes rather than focusing on the outcome. She advised learning from excellence, managing what you are able to control and utilising visualisation to drive you forwards. Remember that you are a team and it is vitally important to work together, not only should you commiserate together but you should celebrate the wins. Day 1 ended with an incredibly passionate and moving talk from Gulwali Passarlay (his book “The Lightless Sky” has also made it onto my wish list!). Guwali started with a thank you and a reminder not to forget the little things you do as clinicians daily as they are the important things. He spoke about his incredible journey as a child refugee travelling alone from Afghanistan across 12 countries, to end up in Britain, go to university and carry the Olympic torch in 2012. It served as an acute reminder of our privileges. His story was about overcoming adversity and never giving up. He reminded his audience that having an experience was one thing, but how you used that experience was another; you have a choice. At the start of day 2 Dr Bruce Keogh, hopefully an man who needs no introduction, delivered the opening keynote. He started by stating that we do not want to loose our NHS by mistake and received a standing ovation at the end of his talk. He outlined the history of the NHS and spoke about innovation. I’m not entirely sure that I agreed with some of what he said, but that is probably best left out of this blog for fear of entering a political minefield that I am unable to control or step back from. He did make a very valid point however, stating that people do not fear change, they fear loss. I will be taking this forward as a part of this year, and my future career. An important role as a leader is to engage people, bring them with us, inspire them to innovate and together we will be able to make a difference. As per day 1, day 2 then broke into smaller group sessions. I attended a resilience workshop. This started by recommending everybody watch ‘Inside Out’, which already had me engaged and listening. The workshop ran through 4 stages of coping and looked at each of these. They explained that resilience found ways to bypass stages, and therefore you progress through these stages quicker, or even skip some stages when faced with conflict or a challenging situation. The focus on the ability to define the problem, which would enable you to employ the correct solution. For example, it is important to be direct in complex situations. Building resilience is based on 4 key pillars; confidence, social support, purposefulness and adaptability. They encouraged assessing your own resilience, a tool to do this can be found here; www.robertsoncooper.com/iresilience/ and focusing on one weakness to improve. It was an interesting session, and do now go and watch ‘Inside Out’! After lunch I focused on 'Changing Culture'. Culture is important within a workplace because it impacts the mood and atmosphere which in turn affects performance. Leadership is about gestures and choices which we make all of the time and these influence the culture within our teams. Culture itself cannot be managed, it is a behaviour pattern which becomes established and over time this is reinforced and amplified by visible artefacts. Changing culture is what we are ultimately trying to achieve with our quality improvement projects. Small gestures can create tipping points which is known as the butterfly effect. Within culture change, the leader is in charge but not in control, this is complexity thinking which involves non linear relationships which cannot be predicted. However, machine thinking is the predominant discourse in the NHS; the NHS can be managed and the leader has complete control. The down sides to machine thinking is that everything falls to the leader, participants and team members are passive which leads to significant amount of stress and pressure. A switch from machine thinking to complexity thinking will change the culture. It is hard but as clinical leaders we should be brave! Make that change, a small shift can have a much wider impact. All of us are leaders and we need to recognise this. The final small group session I attended was on coaching – I am exploring this more on a personal level and will during, the course of the year, write a blog solely focused on this theme.
The Leaders in Healthcare conference closed with a keynote from Deborah Rowland: “How to lead mindful change” The most important message I will take from her session is that good leadership starts with knowing yourself. Invest in yourself as a leader, understand your strengths and weaknesses and recognise them without judgement. When you have spotted something you are able to change it, if you don’t look for it and recognise it, then you cannot. Her four key messages for developing your own leadership style were: Perceiving (tuning into the system), Noticing (staying present), Integrating (all aspects, including difficulty) and Choosing (respond, don’t react). To run through all of these points would take a blog post in it’s own right so instead I will direct you to her book, ‘Still Moving’ which is a challenging but useful read. In conclusion, despite my initial reservations, the Leaders in Healthcare conference was an extremely simulating and enjoyable two days. I never felt during sessions that voicing my opinion was not as valid as the opinion of somebody with significantly more leadership experience than myself. The conference has inspired me to continue to develop myself as a leader, and to first reflect on my own skills and weaknesses which will enable me to be better equipped to help guide the NHS through the challenging times ahead. I would encourage everybody to take a look at the FMLM website and available courses and opportunities www.fmlm.ac.uk |
Editors
Dr Annabel Greenwood Categories
All
|














 RSS Feed
RSS Feed
