|
Dr Tom Cromarty Editor Interests: Paediatric Emergency Medicine, Medical Engagement and Leadership, Simulation, Quality Improvement, Research Twitter: @Tomcromarty |
Welsh Research and Education Network
WREN BlogHot topics in research and medical education, in Wales and beyond
Dr Celyn Kenny Editor Interests: Neonates, Neurodevelopment, Sepsis, Media and Broadcasting Twitter: @Celynkenny |
|
Dr Tom Cromarty Welsh Clinical Leadership Fellow, Paediatric ST5 Trainee Having been a Leadership Fellow for at least three months now, I am beginning to appreciate some of the key traits which great leaders develop and demonstrate. The opportunity to attend leadership conferences enables me to be immersed with people enthusiastic about medical leadership. People who are passionate about improving the lives of medical staff and the patients they serve. The “Leaders in Healthcare” conference was run by the Faculty of Medical Leadership and Management or “FMLM”. The FMLM aims to professionalise medical leadershipand improve patient care. Trainee membership is £84 per annum and you receive a whole lot of bang for your buck if you use all that is on offer. The conferenceconsisted of 3 days of masterclasses, keynotes and plenary sessions with a diverse set of speakers. 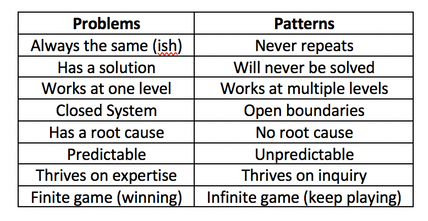 To be honest the most reassuring reflection from the conference was that there are no ground breaking new short cuts, evidence or cheats to employing great leadership. https://hbr.org/2018/11/the-fundamentals-of-leadership-still-havent-changed. Often with the best presentations, your practice is challenged, and usually more questions are generated than answered. Below I have put together a few small summaries of my favourite sessions over the week. I hope you enjoy them, there are also some exercises at the end to try. Political Astuteness: aka “Influence in Organisations” The world in which we work can seem vast, that’s if we are even given the chance to look up and have a glance for ourselves. Early on in a career, often the overwhelming thought is “I don’t do politics”. The usual pattern then follows with “Wowza, I need to know about politics” (to change things for the better) and finally “I need to tell everyone about how to master politics at work” (so we can all change things). This realisation is a like a loss of innocence. It’s easy to think you are just a sheep, but the world is complicated, and you NEED to develop political astuteness to be effective in the world. Directing individuals through authority or using a badge/label to exert power is not leadership, it is management and poor management at that. Leadership on the other hand is the ability to influence individuals. Influence cannot be bought or attained through hierarchy. The internal values one holds, shape their external behaviours. Your behaviours are the markers on which you are judged by others. For this reason, influencing power can be developed by and exerted at anylevel. “Does she/he do what they say?” As an individual you decide…“Am I going to be influenced by him/her?” Patterns not Problems: Working with Intractable Issues Types of problems:
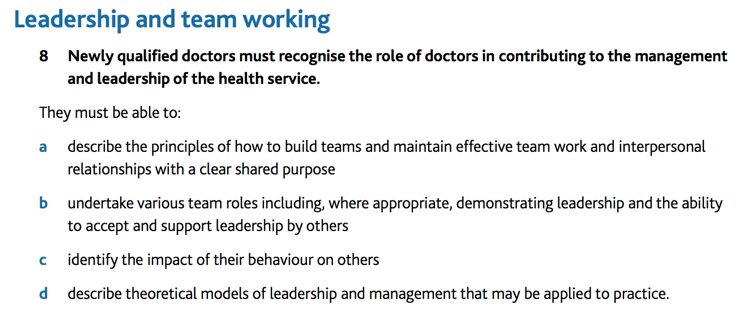
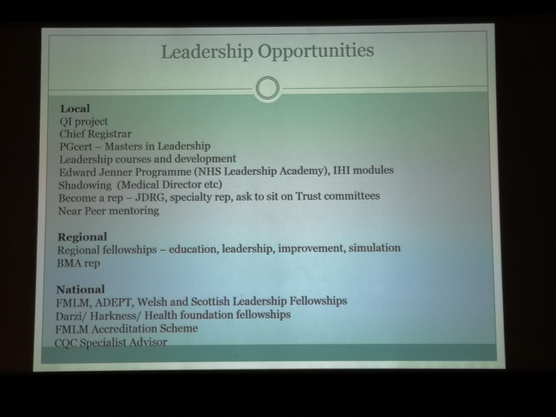
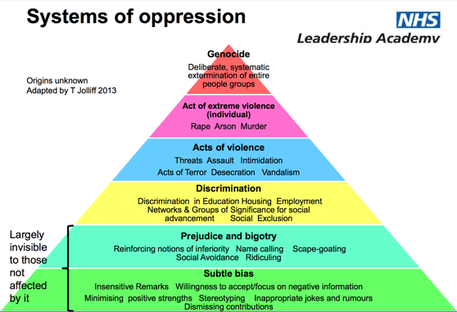
Stephen Powis, National Medical Director of NHS England “In uncertain times, the only known is that there will be change, and it looks like it will be YOU doing the leading!” Digital revolution: Not just AI, but intra-operability, health/medical data, wearables. Link to the global health agenda.Genetic revolution: Need masses of space. Currently leadership is seen as aposition for individualsrather than a behaviour for everyone. We must stop the unhelpful “I’m just a….” attitude and the notion of“Don’t get ahead of yourself there Dr. X, you don’t need to be doing that yet”. Leaders need to aim to regularly add value to the people around them, and everyone can do that, every day. “It will never be someone like me” But think “Control your own destiny” it needs to be done by someone, why not make it you? Read theBMJ Leaderfor leadership tips, research and evidence. Matthew Hancock – Health Secretary England The NHS needs a leadership culture change. We must stop apportioningblame but start really harnessing a culture of learning from mistakes. Anyone who says they have never made a mistake simply isn’t telling the truth. And the truth is at the heart of honest reflection, learning and moving forward. We want staff to challenge without fear and encourage complaints as these are opportunities to improve. Ideally, we want to give away the directive and hierarchical power and consequently empower all individual healthcare workers. This is what we are! This is where were going! This is how were going to get there! Ends with a challenge: What are you going to do? Tim Swanwick - Leadership in the Undergraduate Years “Leadership is a contact sport which brings about change. This cannot be done from the comfort of a desk or department headquarters. The key to developing leadership skills is to get outside of your comfort zone, that’s when you learn the most. Seek out opportunities and go for it. Lead the way to your own future.” “Management makes sure the ship is stable, Leadership sails it in the right direction.” It seems like it wasn’t too long ago where communication skills were thought of as innate. If you had them, you’d be a GP, if you didn’t then you’d be a surgeon or a pathologist (I jest of course but you get the point). Thankfully, at least for the past 15 years, medical schools have recognised that everyone needs to be taught these key skills and consequentially there have been significant improvements. Communication workshops with breaking bad news and explaining diagnosis and management plans have upskilled all doctors and made a massive impact on the care delivered to patients and their families. The tide is changing, leadership & management is being asked about in medical school interviews. Specific leadership skills curriculums are being introduced into universities across the country next year. “What if every newly qualified healthcare professional graduated thinking as a leader.” GMC document 2018 – “Outcomes for graduates”. 1stdomain in the curricula. https://www.ted.com/talks/angela_lee_duckworth_grit_the_power_of_passion_and_perseverance?language=en The science of Leadership & Management is not new. There are 15,000 members of the American Academy of Business who have been researching L&M for many years. The BMJ Leader could bring business school world evidence to medicine. His best advice: Go and get some honest feedback, it will be perhaps the most useful gift you will receive from a colleague?!? Try asking this… “Tell me one thing that I do which is negative?” It takes a degree of bravery for you to ask and reciprocal bravery for them to answer honestly as well. He also insists that we should all have mentors. One can have multiple mentors, e.g. a leadership and speciality mentor. They offer a sounding board for example, difficult interactions with a colleague. They can guide you and order your thinking. Consider the following as some of the more “formal” leadership opportunities: Other Resources: NHS Improvement: Developing People Improving Care Great project in Scotland: Project Lift: NHS Scotland https://www.projectlift.scot/ Diversity And Inclusion in Healthcare Do you know what the 9 protected characteristics of the Equality Act 2010 are? Do you know what “BAME” stands for? This was a really interesting session recognising that even if there is diversity in the workforce or patients, these groups may still lack full inclusion or equality. Leaders need to learn how to o address these issues and respond to unconscious bias. How to hear some difficult messages, and how to respond positively. All too often issues are not confronted as “Oh this is making me feel uncomfortable” or “Of course we’re not, that can’t happen here”. We all need to be “Power aware, Identity aware and Self-aware”. The mindset we embrace in the workplace that liberates other people. Often organisations only take a stand when it gets to “Discrimination” stage, as the lower levels are largely invisible to those not affected by it. We need to upskill leaders so that everyone is aware of what is happening, the behaviour is addressed sooner, everyone has the courage and permission to call out bad behaviour. Courage is the most important of all the virtues, without courage you can’t do any of the other virtues consistently. “The behaviour we walk past is the behaviour we accept” Barriers to successful inclusion:
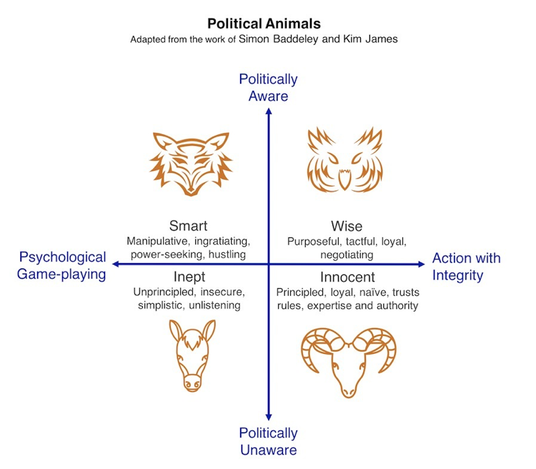
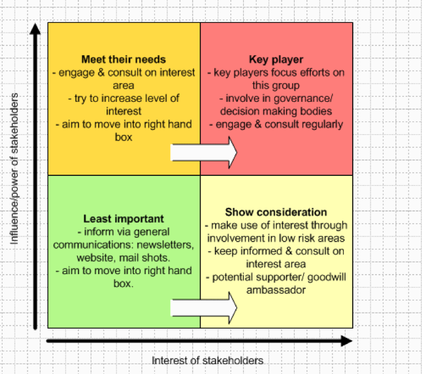
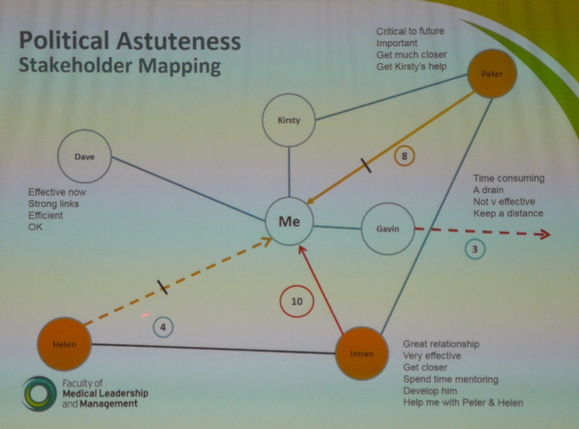
“The only person I can change is myself, how I show up might encourage others to shift their focus, their attention and their behaviour” If you are reading this, you are part of the generation that can make the change! Malala Youssef – Nobel Peace Prize award speech– “Let this end with us” Richard Watson – Futurist: Mega Trends and Technologies2017-2050 It seems that Richard and many others who look to the future can only be sure on one thing, “it is UNCERTAIN and there will be many ways of doing things”.Now for someone who is highly paid for their predictions this seems like a great way of hedging your bets. He also highlighted the worrying change in society with the dominance of screen delivered information and a sedentary lifestyle. Previously children would have been told “behave or you will have to go inside!”, now it is the opposite! He described a world where devices know more about you than you do about yourself. Anybody who says they know exactly what the future holds is lying. However, we spend too much time worrying about it. We NEED to spend time as communities figuring out what we want to happen, using a proactive and positive mindset. It doesn’t matter if we are wrong. We must all have a collective vision of where we want to go, build narratives around the vision and step towards it. I agree with Richards aim of… “Every day waking up and trying to get better, making things better for ourselves and others” Another interesting person is Yuval Noah Harari: 21 Lessons for 21stcentury - interview Professor Megan Reitz: Professor of Leadership and Dialogue Speaking Truth to Power – Have a look for yourself here– it was an excellent 60 mins. Megan delivered a fantastic session about “That moment!” The one a person decides, shall I say something or not, and educated us on the act of “Speaking up”. All the scandals in healthcare organisations of recent times have something in common. People knew bad stuff was going on, but they didn’t speak up, and this resulted in patients coming to harm. One reason is the belief that it is always someone else’s responsibility and absolving oneself from responsibility. “They” aren’t speaking up, “they” need to show courage. Another issue is that often those very people who say the one time they did build up the courage and spoke out, they weren’t listened to and it made no difference. What if you experimented, what difference would it make at a collective level? Think about an occasion where you decided to say something, or not. Megan uses T.R.U.T.H to discuss the issues about these decisions. TRUTH: Trust, Risk, Understanding, Titles, How-to Trust: The value of your own opinion Risk: Realizing the risks of speaking up to powerful people and the ensuing struggle Understanding: Will I be perceived negatively, will I upset someone,“Will I belong”? Titles: We label inherently. Depending on the context, convey levels of authority How-to: Knowing what to say, when, how and to whom Megan then describes a number of traps and behaviours we all fall into which stop us from having the conversations we know we should have! Speak-Up Traps: We doubt ourselves – Imposter syndrome. Check the voice, notice when it comes in. Engage with it, am I going to listen to it this time. The Blind Spot: You will not listen unless you trust the value of their opinions. Can I empathise with how risky it might feel for this person to be speaking up? What titles do I have on me to affect what kind of information this person is telling me? Individuals ALWAYS think they are better at listening than other people. Listen-up traps: It’s easy to forget that no matter how lovely and approachable we seem as juniors, decades later, given some labels and titles, we are all quite scary. Make sure you don’t send“Shut up” signals and not “speak up” signals by knowing your face (and the rest of your body language signals, and environment you create). Today and every day, we make choices about what to say and when to stay silent. When we really help someone else to speak up or silence them. Choices feel mundane but if you add them up together it is what defines you. How you speak up and listen up represents the values you hold and the culture in which you work. If you think about it and act accordingly, you will change habits and change cultures. Some exercises and information to peruse at home in your own time! Exercise 1: Personal Values Think about your own values! What matters to you? How do you display your values at work? Much of the conflict at work results from a mis-alignment of core values. Spend some time writing down your beliefs. What behaviours demonstrate your values? None of these have anything to do with medicine or your background/grade. Exercise: Search for 50 personal values on the internet. Step 1: Make 3 groups of importance to you (High, Medium, Low) Step 2: Place each of the 50 values in a group Step 3: Take the “High” group and again split these into high, medium and low. Step 4: Group similar values together until you have 3-5 left. Step 5: Welcome to your values, enjoy them, be true to them, live them! Check out…Harry Kramer, Values in Leadership. One moves around the grid, depending on what is being demanded of us. Who else is there? Personal circumstances? Ideally there is a sweet spot (in Green) of moving around all areas, aiming to avoid the inept/donkey. How do you bring people and landscape together in your head and put it onto paper? Stakeholder mapping, mind mapping, network mapping. Another tool: Understanding people landscape map(Like Nike said… just do it) Length of the line: how far they are away from you Arrow direction: if you want them to be closer or further from you Dotted lines: are relationships you want to develop Small circles: /10 effort to build relationship (realistically) Stops: how far you want to bring them closer Wordsadd a narrative: Rich picture without words doesn’t show much Update it regularly, do it for different work groups. Use it for work networks, family situations, family events. For example, see diagram below: Do you know the 9 protected characteristics in the UK workplace? Age, Disability, Gender Reassignment, Marriage and Civil Partnership, Pregnancy and Maternity, Race, Religion or Belief, Sex, Sexual Orientation. A reflective exercise to do at the end of any teaching session, activity or experience. Take for example this blog (which I’ll admit has a lot crammed into it). Try and think of at least one behaviour in each of the following headings... Start doing: something you don’t do but think you should actively work to do more of. Stop doing: something you currently do but will actively try to do less of or stop doing. Continue doing:Something you are doing already but will do more of it because it works.
0 Comments
Assim Ali Javaid – ST3 Paediatric trainees in Wales are a lucky bunch in many ways but one of my personal favourites is the chance to spend your ST3 year as an academic year. As far as I know, Wales Deanery is the only one that offers this option. Everywhere else you’re either on an official Academic Training Fellow Programme or not. Wales Deanery has been running the Academic ST3 Year option for the last 3 years and it offers paediatric trainees in Wales a chance to explore interests in research and/or teaching before formally entering Level 2 training. This is done alongside providing out of hours clinical cover at the University Hospital of Wales (UHW), usually as the Specialty SHO on call. There is only one Academic ST3 post available per year and it is largely up to the trainee who gets the post how they use the year. As such, every trainee who has had the post for the last 3 years has had a different experience.
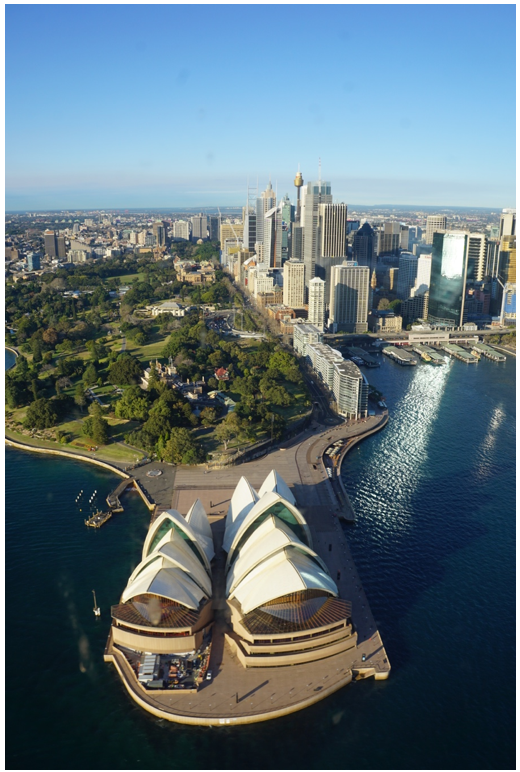
In my case, I have an interest in research and teaching and wanted to explore something related to Paediatric Emergency Medicine. After discussing options with various consultants, I decided to join Professor Alison Kemp’s team and explore burns injuries in children from a safeguarding perspective. Alongside this I have offered to cover a clinical trial being carried out by the UHW Research Unit, taken up multiple teaching opportunities and started a Postgraduate Certificate in Medical Education. With all this on my plate, my day-to-day work varies greatly and I don’t have a typical “day” of work. In order to give you an idea of what I’ve done with this year I’ll briefly mention the different roles I’ve taken on. It’s worth remembering though, that this is a very flexible year and there are a number of other ways to use the time. The bulk of my work is based in research. The burns team I work with has a database of around 4,000 burns cases with huge amounts of usable data recorded for each case. After deciding on a couple of research questions with Professor Kemp, most of my time is spent reading through the relevant literature, working with the database and trying to answer it. Proposing and answering research questions uses an entirely different set of skills to managing patients on the ward and one of the main advantages to this year is getting a chance to exercise a set of cognitive functions we rarely get to use in clinical practice. For those unfamiliar with statistical analysis, as I was, this can be pretty daunting at first but as you have no in-hours clinical commitments, there is plenty of time to learn how to work with biostatistics. This would essentially be all I did during the day if I hadn’t chosen to take up a number of extra activities to break the monotony of research. During most weeks I will have two to four half day sessions dedicated to doing some of this extra work. I provide clinical cover for a trial being carried out at the Research Unit in UHW, for which my job is writing prescriptions, doing blood tests, interpreting ECGs and assessing any children who become acutely unwell while participating in the trial. Alongside this I spend a lot of time teaching. There are numerous teaching opportunities with UHW or Cardiff University and, I should point out, all are available for anyone to help with. However, the advantages of being an Academic Trainee is that, first, you have the time available to do a lot of teaching and, secondly, you’re often one of the first trainees to come to mind when Consultants or registrars are looking for help with teaching. So far this year I’ve been involved with teaching clinical skills to medical students, facilitating ethical debates between medical students, providing teaching to medical students on paediatric emergencies and paediatric prescribing, helping with mock paediatric exams for medical students at UHW, being a clinical tutor to final year students doing a module in Patient Safety, doing paediatric simulation training with final year medical students and providing teaching sessions for paediatric trainees due to sit their MRCPCH written or clinical exams. There are considerable out of hour’s responsibilities too. The Academic ST3 usually goes on to the Specialty SHO on call rota, which is 50% banded at present, providing out of hours cover for Surgery, Neurology, Cardiology, Respiratory, Renal and Oncology. However, another great advantage to being an ST3 at UHW is the option to step up and cover your on call shifts as the Registrar instead. UHW is a nice place to do this as you’ll be paired with registrar covering General Paediatrics (usually more senior than yourself) and there’s an onsite PICU registrar for help also. Of course stepping up to Registrar is entirely optional and the post is based on the assumption of SHO level cover. If you’re considering applying for the Academic post for ST3 there is only one place available per year, so it can be competitive. In order to qualify, the applicant has to be on course to have completed their membership exams, i.e. all the written papers and the clinical exam, by the end of ST2. If that’s the case, what you need to consider is whether this is what you’d like to do with your ST3 year. Trainees who aren’t particularly interested in research or teaching, those who want to get as much SHO level clinical experience before entering Level 2 training or those who want to skip ST3 altogether and go straight to ST4 probably have little to gain from spending their ST3 year on an Academic post. It’s also not particularly great for those who want to gain early experience in a particular sub-specialty in UHW, with a possible future SPIN or Grid application in mind. However, this is a fantastic post for anyone with an interest in research and/or teaching, for those looking to improve their CV for a future Grid application or those who just want a bit of a break from constant clinical practice. It’s a rare chance to experience something outside of clinical practice, without having to take time out of the programme in order to accomplish it. Personally, I can’t recommend the Academic post highly enough! An OOPE in Sydney, Australia. Dr Thomas Cromarty I have just returned from an OOPE and wanted to share my experience of living and working in Australia. After embarking on the best training scheme of them all (Paediatrics) in 2012, I worked around South Wales from ST1-5. The Welsh Paediatric Training Programme Director is keen to produce well rounded paediatricians and encouraged me take the opportunity in Westmead Children’s Emergency Department, Sydney. I could tell you about all the trips we went on: Visiting my dad in Canberra, Campervanning around Tasmania, watching the tennis in Melbourne, taking selfies with the quokkas on Rottnest island (Perth), surfing in Margaret River, watching the Commonwealth Games in the Gold Coast, swimming with turtles on the Great Barrier Reef and night treks in the Daintree rainforest. But that will just make you jealous and me sad, so I’ll try and give you unbiased view of my reflections on a year working there instead. “Big surf” in the Australian Life Saving Ironman @ Queenscliff Life Saving Club Nat and I with the Rottnest star of the show aka “The Quokka” It would make a mockery of a blog if I didn’t start by mentioning the Work:Life balance situation! My partner and I lived 500m the beach in a place called Queenscliff near Manly. Our end of the beach was quiet, had waves most of the time and was pretty much perfect. We lived on the top floor of an apartment block which included a roof top terrace aka skin cancer zone. As an “outdoorsy type” I was in heaven. There were running, cycling and triathlon clubs, surfing beaches, SUP, yoga studios, open water swimming and even Dragon Boat racing! You name it, it was expensive, but it was available. Unfortunately, I worked 40km away in the west of the city which meant that I had my old friend, traffic, to contend with on a regular basis. I worked 4 x 10 hour shifts per week in the Paeds ED, with most shifts mirroring the peak attendance times of 14:00-00:00. Despite the commute, there was no chance of me moving to other side of the world and not living by the Ocean! The Work: Positives
Dr Smarty Pants, hard at work… at Westmead Children’s Hospital The Work: Negatives
I produced a PDP of goals to achieve throughout the year, these included upgrading my USS skills as well as confidence managing paediatric trauma and minor injuries. I found this particularly useful and would encourage everyone to take some time to establish some short, medium, and long term goals for life both in and outside of work. I think it is essential for all medical staff to experience working in a number of different settings. This enables them to be exposed to a number of working environments and behaviours, choosing which to adopt into their personal style, facilitating their journey to becoming a more effective clinician and leader. My year working abroad will undoubtedly be different to yours and you need to decide if it is right for you (and your significant others!) What I would say though is if you don’t try it, you’ll never know… What’s the worst that could happen?! The start of “Hells Bells” 24 hour adventure race in Noosa, Queensland Helicopter trip over Sydney CBD Fair Dinkum, I had a ripper of a year out and am looking to continue that growth of skills this year as a Clinical Leadership Fellow in Cardiff and Vale, engaging junior doctors in leadership and QI development. If you want to get involved with this project, have any questions about taking a year out or just want to see some more photos please don’t hesitate to contact me at [email protected]. Favourite phrases:
Patient’s parent: She’s been crook for days mate? Doctor: Nah no worries mate, she’ll be right! |
Editors
Dr Annabel Greenwood Categories
All
|










 RSS Feed
RSS Feed
