|
Dr Tom Cromarty Editor Interests: Paediatric Emergency Medicine, Medical Engagement and Leadership, Simulation, Quality Improvement, Research Twitter: @Tomcromarty |
Welsh Research and Education Network
WREN BlogHot topics in research and medical education, in Wales and beyond
Dr Celyn Kenny Editor Interests: Neonates, Neurodevelopment, Sepsis, Media and Broadcasting Twitter: @Celynkenny |
|
Guest blogger Dr Sandheeah Ramdeny Over The Wall, is an amazing activity camp which is free for children, teenagers and family who are living with serious health challenges. It is a national charity which provide support to kids who are faced with seious health challenges through transformational residential camps across the UK. There are different camps which take place at different times of the year some of the camps focused mainly on the kids living with serious health problems some on the siblings and some on the families. These kids who lives with their health problems are mostly affected by their illness and are unable to participate in fun activities normally enjoyed by their friends and peers. Consequently, these kids then have a reduced self-esteem and self-confidence which can negatively impact on their growth and their development. The main purpose of Over the Wall, is to tackle these issues to allow a transformational change to occur in a safe environment with medical professionals being around to provide the medical care that they need so that the campers return with a new sense of their abilities and ambitions and improved self-confidence. I choose to take part in the health challenge camp which was mainly focused on the kids with serious health challenges which took place in Strathallan, a really nice boarding school located in Perth, Scotland with breath taking landscapes. The medical team were named the ‘Beach Patrol’, which consisted of 5 paediatric Spr, on GP, one paramedic, two nurses. The camp lasted for a week and the first few days were mainly centred around simulation scenarios to deal with the different cases which could arise whilst in camp as well as becoming familiar with the medical condition of the campers and to learn about their individual management plan. There were around 60 campers with a wide range of medical condition ranging from Type 1 diabetic, ALL, sickle cell disease, cerebral palsy, medical condition requiring bowel washout, Haemophilla, Marfan syndrome, Noonan’s syndrome, DiGeorge syndrome, kids with heart failure, patients on daily chemotherapy. Our normal day would start at 07 30 am in the morning and end around 2230 with 2 of us taking turns to do a night shift to provide cover each night. As the medical team, we were involved in giving the campers their medication before breakfast, during lunch and dinner time and accompanying the campers whilst they were carrying out their activities such as ensuring the young Type 1 diabetic would have their blood sugar level monitored and insulin administered accordingly. Each one of us would be closely attached to a camper who could potentially become sick so that we would be able to keep a close eye on them and we would accompany them to all the activities. Most of the activities were based on the campus of the boarding school. For instance, each day would have activities planned such as archery, music, drama, swimming, arts and crafts. These activities would be focused to allow them to realise their potential and us trying to make them believe in themselves and go beyond what they can do. The evenings were based mainly on Talent night where the campers would do an interesting act, play, dance or music to demonstrate each of their talent. There was one day, when the whole team went to Edinburgh to go to the international climbing arena. This was an excellent opportunity to allow campers to reach beyond their capabilities. For instance, on the camper in my group, a lovely 8 year old girl, who was afraid of heights and did not want to attempt any climbing. However, when she saw the other kids having so much fun and me being by her side telling her that I would be here and she could just attempt to climb and that she didn’t have to go too far. She was initially reluctant but the finally agreed. When she started climbing., she realised that she wasn’t scared anymore and was able to climb. When she got down, she was very emotional as she was now able to do something that she could not do. She said that she would never forget this experience. Some of the statements of the campers from Over The Wall, “It is no exaggeration to say that my experience with OTW was on the best weeks of my life. It Is true what they say.” To me, I do believe that Over The Wall provides an amazing opportunity to allow seriously ill children to go beyond the boundaries of their illness and have a positive impact for the rest of their life. For more information go to www.otw.org.uk
1 Comment
Princess of Wales Hospital, Bridgend, Friday 8thJune 2018 Annabel Greenwood Paediatric ST3 Trainee Broadly speaking, I feel our exposure to safeguarding training in the early years of paediatric training is limited.
Before you know it, you are the registrar on-call, out of hours, contacted with a complex child protection referral. As a junior paediatric trainee about to transition to middle-grade training, I will inevitably at some point, be faced with this scenario, and if I’m to be completely honest, the thought has previously caused a slight degree of tachycardia, hyperventilation and perspiration on my part, at the uncertainty of such a situation! I therefore searched for a way to dispel my fears and came across a child protection simulation course set-up by Dr Emily Payne, ST8 Community Paediatric Trainee in Wales. This fantastic one-day, multiagency simulation course has certainly enhanced my confidence in the management of child protection cases and I would certainly recommend the day to my fellow trainees. The course facilitates approximately 6-10 trainees, a perfect sized group to allow plenty of opportunity to ask questions and share our experiences with each other. The day began with a couple of short lectures, setting the scene for the day, addressing some key safeguarding principles, including the rights and responsibilities of all doctors, and an outline of the child protection process. We also discussed the ‘ACE’ (Adverse Child Experiences) Study, which has demonstrated that for every 100 adults in Wales, 47 have suffered at least one ACE during their childhood, and 14 people suffered 4 or more events. ACE are stressful experiences occurring during childhood that directly harm a child e.g. sexual, physical or emotional abuse, or effect the environment in which they live e.g. domestic violence, mental health, parental separation. It has been shown that ACE impact across the life course, e.g. affecting neurodevelopment in the early years, potentially causing social, emotional, and cognitive impairment, and perhaps leading to the adoption of high-risk behaviours and crime later on in life. Later in the morning we divided into pairs for 3 workshop sessions focusing on physical, emotional and sexual abuse respectively. These informal, small-group workshops were based on a clinical scenario and provided an excellent opportunity to voice any queries or concerns we had regarding the different categories of abuse. In the afternoon, we worked through a number of simulation child protection scenarios with actors playing the role of the child’s parents, making the situation as realistic as possible. At the end of each scenario we re-grouped to provide feedback and discuss the case in more detail. I felt that this was a completely safe environment to practice leading challenging safeguarding scenarios, and found it extremely useful to receive constructive multiagency feedback, from doctors, social workers and the police. The day was brought to a close with a simulated strategy meeting, and we all played the role of a different member of the multiagency team. This provided a fantastic insight into the role of each member of the team, and demonstrated how everyone works together to collate the evidence in order to generate an accurate account of events, to ensure the safety of the child. I thoroughly enjoyed the course and feel that I will now make the transition to middle-grade training with enhanced knowledge and confidence to manage challenging safeguarding scenarios. Dr Annabel Greenwood (ST3), inspired by Dr Ian Morris (Consultant Neonatologist, UHW)
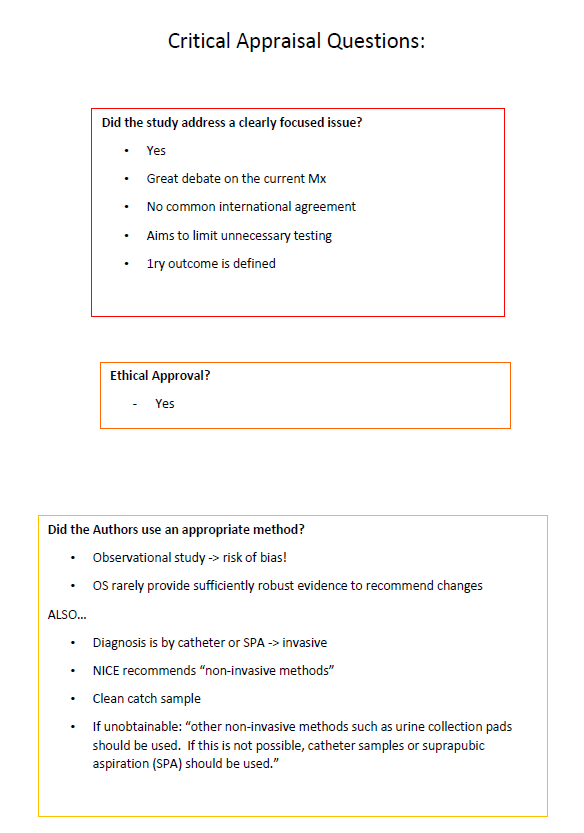
Relevance– How important is the content of the article to me, my patients, and my practice? The title and the abstract will help you answer these questions. Internal validity– How sound is the study? i.e. how accurate is the study? Look at the methods to help ascertain this. External validity– How applicableis the article to my practice? i.e how much can I generalize it? The methods and results sections will help you assess the external validity. Now, with those 3 key principles in mind, let us picture the scene… You’re an ST7 trainee, approaching the end of your paediatric training, years of hard work and dedication behind you, your CCT within touching distance. You’re at your START assessment, the last hurdle before consultancy, and now for your critical appraisal station. Twenty minutesto read the article AND then appraise?! How on earth am I going to do this I hear you cry?! Stay calm, take a deep breath, and burst forth the 9 key questions that will help you ace the station! Describe the study What is the type of study (principal method) What type of question is being asked? (e.g. Diagnostic? Therapeutic? Economic?) Where was the study carried out? (is it multicentred or single study) What are the key features?
Describe the research question
What is the relevance of the question? This is usually described in the introduction. Is it an important question? Is it worth reading on? Does it correlate to your clinical practice/scenario? Describe the methods Use the PICO template, but expand…. What are the inclusion/exclusion criteria? Is there any masking or blinding? Are there any secondary outcomes? Comment on the internal validity i.e. how accurate is the study? Use various checklists e.g. CONSORT, STROBE, PRISMA Is there a risk of bias? Summarise the primary results Summarise the key secondary results(briefly) Comment on the External validity– i.e. describe the generalizability of these findings Were the inclusion/exclusion criteria reflective? Limitations? Consider the paper in conjunction with other studies i.e. how does it fit with the evidence out there? Conclusion Overall, does this paper help you answer your clinical question? Important to look at the clinical context! ….And just like that, you did it! 9 logical, concise steps to critical appraisal for the START assessment. Of course, this is only a suggested approach, but one which I will most certainly be adopting for future critical appraisals. Now, where did I put that journal?.....
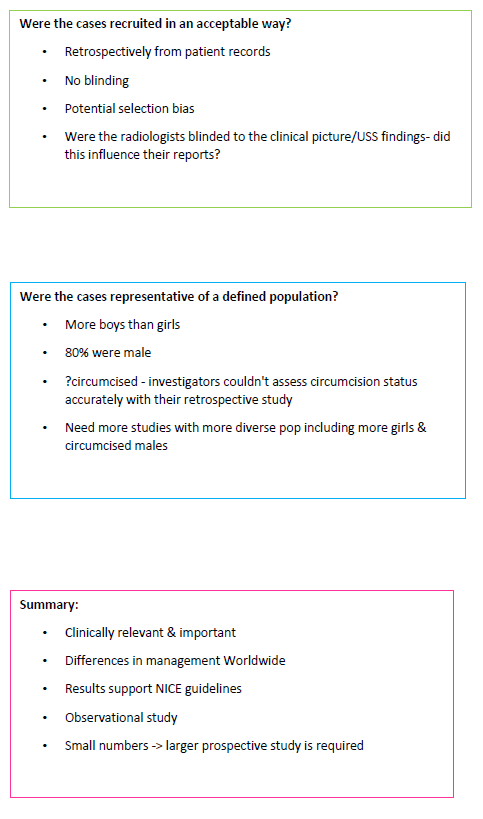
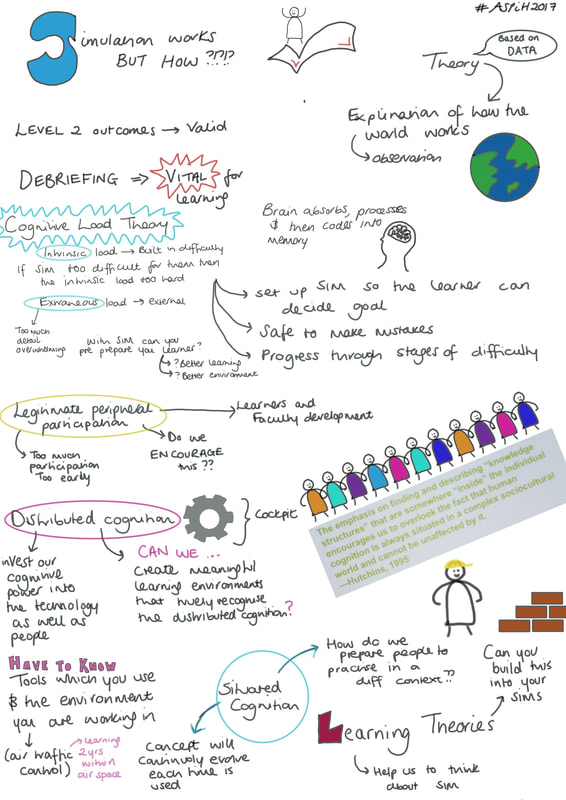
 Association for Simulated Practise in Healthcare (ASPiH), 6th – 8th November 2017, Telford International Centre By Rebecca Broomfield As a part of my Clinical Leadership Fellow year I am focusing on the evaluation of simulation as a teaching technique, attempting to relate this to improved patient safety and improved patient outcomes. Anybody who knows me knows that I love a simulated scenario as a teaching session, it’s not everybody’s cup of tea but it really fantastic opportunity to learn. I therefore jumped at the chance to attend the ASPiH conference. I started by attending a pre-conference workshop session based on Evaluation of Simulation. I was actually unaware that pre-conference workshops happened. A lot of big conferences have a day prior to the main event which they run focus groups or workshops that people can attend to be taught and explore ideas with like minded others. My workshop covered a lot of educational theory behind simulation and how you can use this to evaluate your simulation sessions. Key learning points included the fact that a poor evaluation undermines the development of new approaches. The evaluation itself is “a systematic acquisition and assessment of info to provide useful feedback about some [object]”, therefore while evaluation of the session is often an afterthought and a quick Likert score which nobody reads or bothers to fill in correctly, it really should be an important part of the structure of the simulation session. We also discussed how to structure your evaluation and a way to form a measurable outcome. The actual conference kicked off on the Tuesday morning. There were key note sessions delivered at different points in the day and there were split sessions with a choice of what to attend between these. The keynotes were all interesting a relevant to current trends in simulation. Cherrie Evan’s talk on delivering simulation based education in Africa was an eye opener and inspiring to see how correctly administered simulation can really make a significant difference in patient safety and improve outcomes. Her work was through an organisation called Jhpiego and focuses on the safety of a mother and newborn at delivery. Dr Gabriel Reedy delivered a session on the educational theory behind education, which is particularly relevant to my project. All the keynotes can be found at: http://www.youtube.com/playlist?list=PLzm6Ad9XIwxmnblhwSbEcjceDNpUFW1iu - I’d also recommend watching Dr Al Ross’ talk on Resilience within healthcare if like me you’ve become a bit disillusioned with the term resilience and its meaning. In between the keynotes there was so much going on, it was almost overwhelming. Sessions ran throughout the day with presentations about many different aspects of simulation from setting up in-situ simulations with an emergency department, evaluation of simulation sessions and development of simulations focusing on wellbeing and resilience. The sponsors were around with lots of new technology and we got to play with all the new simulation models. There is a particularly interesting baby and child model which is amazingly lifelike and provokes significant emotion (I automatically checked the veins on this model immediately after picking it up!) I also got to observe a session using a interactive tent to have a projected environment in which to run a simulation. The situation that I observed was a building site with an injured builder. The walls were displaying images of a new housing estate and there were building site noises being played throughout. The tent feeds into the educational theory of distributed cognition suggesting that we need to be investing cognitive power into the technology as well as the people.
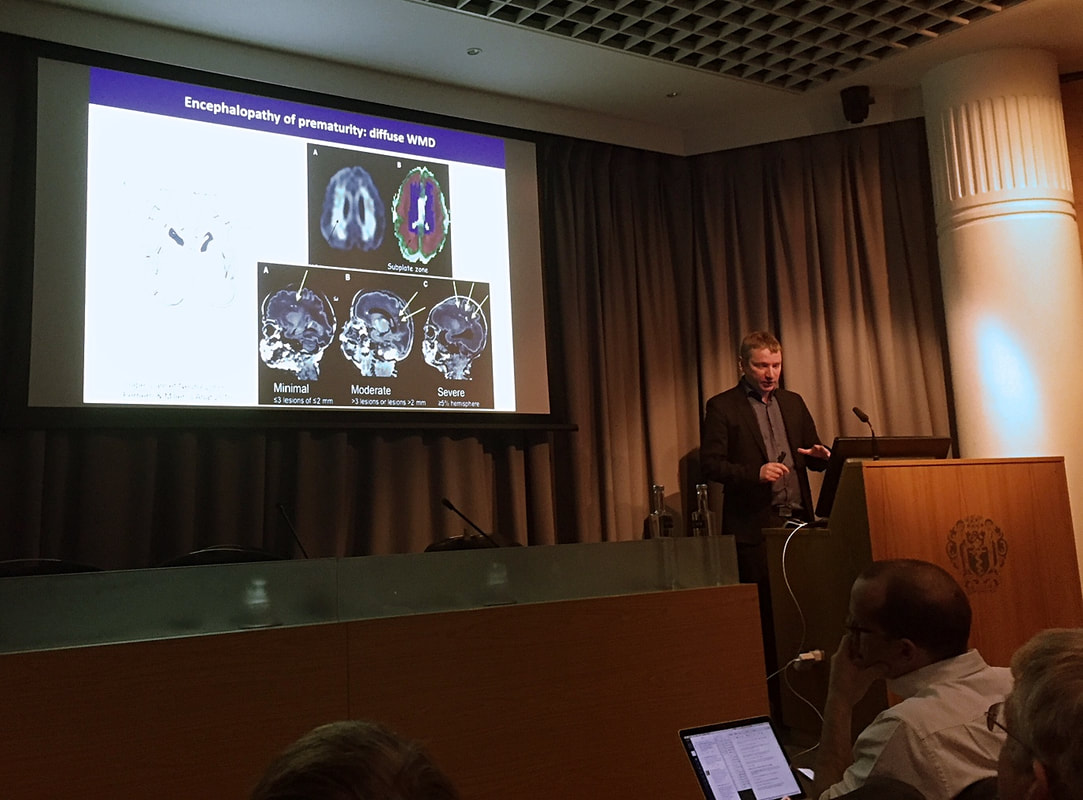
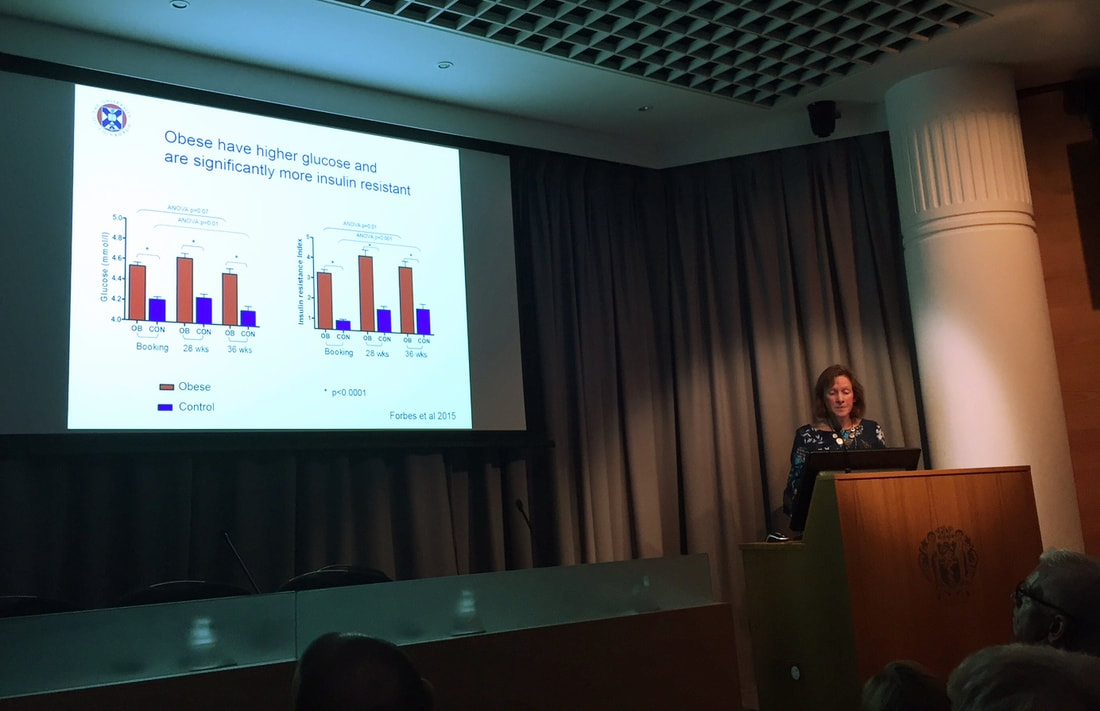
ASPiH is working hard to provide a standardised quality simulation teaching nationwide and as such they have developed their standards documents which can be found here: http://aspih.org.uk/standards-framework-for-sbe/. These outline the standard expectations for running a good simulation education program. It is looking into developing an accreditation system in order to promote good quality simulation. We know that simulation teaching is good, we now need to prove it and regulate its delivery in order to standardise experiences. I am even more excited about simulation teaching and its huge potential since attending this conference. I tweeted throughout the days including sketchnotes of some of the sessions I attended, if you are interested in these they are on my twitter feed for the conference dates. I am planning on attending the Paediatric specific International Pediatric Simulation Society (IPSS) conference during May in Amsterdam, if anybody fancies joining me you’d be welcome. If you want more information on ASPiH then visit their website here: http://aspih.org.uk/ 9th November 2017, Royal Society of Medicine, London By Chris Course On 9th November, the Neonatal Society held their Autumn Meeting at the Royal Society of Medicine in London. The program included oral presentations of submitted abstracts as well as invited guest speakers. There were a variety of topics covered, from studies looking at postnatal dexamethasone use upregulating surfactant proteins in preterm lamb models, surgical outcomes of preterm infants with congenital diaphragmatic hernia over a twenty-year period, increasing demands on neonatal unit for management of hypoglycaemia and breastmilk exposure influencing preterm brain development. The Widdowson lecture was given by Professor Pierre Gressens of King’s College and concerned the genomics of preterm brain injury. To be honest, some of the technicalities of the science and molecular pathways went a bit over my head, but there seemed to be some promising preliminary results on upregulating pro-repair inflammatory pathways and suppressing the damaging and immunomodulatory pathways by using tiny engineered pieces of DNA to protect the preterm brain’s white matter. Might seem a bit removed from clinical practice now, and seemed to be still a way from trials in human subjects, but then again, in a decade who knows what we’ll be doing on the wards! The keynote lecture came from Professor Rebecca Reynolds of Edinburgh University, who gave a fascinating talk on maternal health determining offspring life-course outcome. She went through data showing that it had been identified in the 1960’s that areas with high infant mortality ratios at the turn of the last century, went on to become areas with high rates of cardiovascular deaths in later life. Over the years, various studies have been conducted looking at the fetal programming effects of raised cortisol (secondary to maternal stress) reprogramming the fetal hypothalamo-pituitary-adrenal axis, and raised BMI/poor maternal diet/lifestyle leading to impaired insulin sensitivity in the fetus. Cohorts have been followed-up which show these infants have higher rates of type 2 diabetes and poorer neurodevelopmental outcomes/behavioural problems. There’s also a cohort of mothers in Finland that’s been followed up based on the amount of liquorice they consume…. Might seem odd, but apparently, it’s a popular snack in Finland, but suppresses an enzyme in the placenta that prevents too much cortisol passing into the fetus. It really highlighted how what we do in early life, and even before conception, can affect us for the rest of our lives! It did however also make me aware that in our role as paediatricians/neonatologists we have an opportunity to change long-term health for the better too. For anyone who hasn’t been to the Royal Society of Medicine, it’s a suitably impressive venue (befitting the name really) just behind Oxford Street, which was perfect for a leisurely lunch and a spot of early Christmas shopping during the society’s business meeting. And the day was rounded off with a drinks reception – what’s not to love! The day really brought home how diverse the neonatal research world is, and how much work is going on to try and improve understanding of physiology, diseases and develop new treatments. The Neonatal Society hold three meetings a year. The Autumn and Spring meetings are one-day, held in London, are free to attend and don’t require prior registration. The Summer meeting changes location around the UK (and sometimes ventures into Europe), with next year’s being held in Dublin in June. Abstracts are invited to be submitted for all the meetings, and are a great opportunity to get projects presented at a high-quality, national meeting – good for the CV/portfolio! Additionally, once you have presented at a society meeting, you are eligible to apply for membership.
For more information, check out www.neonatalsociety.ac.uk St Brides Hotel, Saundersfoot, Friday 10th November 2017 Hosted by Glangwili General Hospital & Bronglais Hospital By Annabel Greenwood This Autumn’s WPS meeting took place in the absolutely stunning location of St Brides Hotel in the picturesque seaside town Saundersfoot. Nestled in the clifftop, overlooking the breath-taking rugged Welsh coastline, it provided the perfect backdrop for an invigorating day of presentations, discussions and networking. The day began with the invitation lecture from the esteemed Dr Trevor Brown, Consultant Paediatric Allergist at Ulster Hospital, on cow’s milk allergy (formerly cow’s milk protein allergy). Ever a diagnostic and management paradox for GPs and general paediatricians, this in-depth discussion covering IgE verus non-IgE mediated reactions, clinical presentation and potential management options was invaluable. The morning session presentations were abundant in variety and interest, including projects and audits from Cardiff University Medical Students, Welsh Paediatric trainees, and Consultants. Of highlight during this session was the fantastic prize-winning project presented by our very own WREN co-chair Dr Siwan Lloyd on head injury following infant falls on the postnatal ward – a case series. The variety in the approach to investigation and management of such patients was fascinating, especially given the high rate of CT head abnormalities of those imaged. The subsequent departmental guideline implemented at UHW will certainly help standardise care and provide more clarity and direction for management. Almost time for lunch, but of course not before the brilliant Guest Lecture from Detective Superintendent Anthony Griffiths, Head of Public Protection, Dyfed Powys Police – ‘Child Protection: The Challenges for Policy and Multi-Agency Working.’ This lecture provided an invaluable insight into the challenges often faced by the police in child protection cases. The videos and images used were extremely powerful and emphasized the great difficulties in tracking down offenders in today’s society, particularly given the huge smart phone and social media influence. After an action-packed morning of presentations and lectures it was time to refuel with a mouth-watering lunch overlooking the absolutely spectacular scenery. Coffee could be taken onto the balcony, and what a treat it was to catch up with friends and colleagues with the sound of the waves crashing onto the shore below. There was also the opportunity during this lunchbreak to visit the exhibitor stands, the main theme being cow’s milk allergy, in-keeping with the invitation lecture earlier in the day, and there were a variety of different formulas to sample at these stands (some of which far more palatable than others!!) The afternoon session was equally interesting and stimulating, including presentations inspiring and empowering trainees, highlighting the importance of blogging, social media and trainee-led initiatives to encourage learning and champion change. The final Guest Lecture of the day was provided by the highly-regarded Dr Julian Forton, Consultant in Paediatric Respiratory Medicine and Cystic Fibrosis, UHW, on ‘the new C21 Curriculum at Cardiff University School of Medicine.’ It was absolutely fascinating to learn how the curriculum and course structure has evolved since my days in medical school! The aim is for a more case-based, small group learning approach with early clinical exposure. The exam format was also an interesting change, whereby all years take the same end-of-year exam, with the focus being on demonstrating improvement and development each year. As the sun was setting at the end of a wonderful day, it was time for the evening entertainment in the form of the ‘celebrating trainee event’ followed by the formal evening dinner. This year the Best Trainee prize went to Dr Siwan Lloyd in South Wales (taking a clean sweep of prizes!) and to Dr Stacey Killick in the North. Best Educational Supervisor went to Dr Zoe Roberts…congratulations to all!
The day was wrapped up with a splendid evening of dinner and dancing (thank goodness for the spa to recover the next morning!) Once again, WPS has delivered an outstanding conference! It provides an excellent platform to showcase your work, and to become inspired by colleagues and friends. It also provides the opportunity to learn from lead professionals in their specialised field, and to celebrate the achievements of others. We certainly are lucky to have such a wonderful paediatric society in Wales! Now, who’s joining me for the Spring meeting?!.... |
Editors
Dr Annabel Greenwood Categories
All
|


















 RSS Feed
RSS Feed
