|
Dr Tom Cromarty Editor Interests: Paediatric Emergency Medicine, Medical Engagement and Leadership, Simulation, Quality Improvement, Research Twitter: @Tomcromarty |
Welsh Research and Education Network
WREN BlogHot topics in research and medical education, in Wales and beyond
Dr Celyn Kenny Editor Interests: Neonates, Neurodevelopment, Sepsis, Media and Broadcasting Twitter: @Celynkenny |
|
Huw Davies, ST3 Paediatric Trainee, Wales I attended the conference entitled "The Importance of a Supportive Environment for Healthcare Professionals". Awareness of burnout, mental health difficulties, and bullying affecting doctors and others in healthcare is at last increasing. We heard several moving accounts from those at all stages of training. A common thread was that all our speakers could objectively be considered high flyers, on the surface coping well with tough jobs. Yet all had felt like failures inwardly: because they were bending under demands of critically understaffed rotas; because they felt responsible for a tragic patient death; because they had been targeted for victimisation, for no evident reason. They had all looked around at peers seeming not to struggle, and thought "what must be wrong with me, that I can't cope". As a profession, our high standards and sense of duty make it hard to take stock and realise that we ourselves need help. Our speakers all mentioned this as the hardest and the most critical step.
The stories we heard stimulated round table discussions discussing what we had heard - how can individuals and institutions value and support our professionals and maintain their resilience throughout a medical career. We had access to well presented research data from the posters on display. I would highly recommend to anyone to raise these issues with their colleagues - those not giving them thought might well be the ones in most need. I hope this conference is replicated again soon and that these voices are heard at local levels too.
0 Comments
Dr Tom Cromarty Welsh Clinical Leadership Fellow, Paediatric ST5 Trainee Having been a Leadership Fellow for at least three months now, I am beginning to appreciate some of the key traits which great leaders develop and demonstrate. The opportunity to attend leadership conferences enables me to be immersed with people enthusiastic about medical leadership. People who are passionate about improving the lives of medical staff and the patients they serve. The “Leaders in Healthcare” conference was run by the Faculty of Medical Leadership and Management or “FMLM”. The FMLM aims to professionalise medical leadershipand improve patient care. Trainee membership is £84 per annum and you receive a whole lot of bang for your buck if you use all that is on offer. The conferenceconsisted of 3 days of masterclasses, keynotes and plenary sessions with a diverse set of speakers. 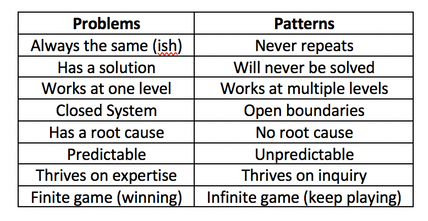 To be honest the most reassuring reflection from the conference was that there are no ground breaking new short cuts, evidence or cheats to employing great leadership. https://hbr.org/2018/11/the-fundamentals-of-leadership-still-havent-changed. Often with the best presentations, your practice is challenged, and usually more questions are generated than answered. Below I have put together a few small summaries of my favourite sessions over the week. I hope you enjoy them, there are also some exercises at the end to try. Political Astuteness: aka “Influence in Organisations” The world in which we work can seem vast, that’s if we are even given the chance to look up and have a glance for ourselves. Early on in a career, often the overwhelming thought is “I don’t do politics”. The usual pattern then follows with “Wowza, I need to know about politics” (to change things for the better) and finally “I need to tell everyone about how to master politics at work” (so we can all change things). This realisation is a like a loss of innocence. It’s easy to think you are just a sheep, but the world is complicated, and you NEED to develop political astuteness to be effective in the world. Directing individuals through authority or using a badge/label to exert power is not leadership, it is management and poor management at that. Leadership on the other hand is the ability to influence individuals. Influence cannot be bought or attained through hierarchy. The internal values one holds, shape their external behaviours. Your behaviours are the markers on which you are judged by others. For this reason, influencing power can be developed by and exerted at anylevel. “Does she/he do what they say?” As an individual you decide…“Am I going to be influenced by him/her?” Patterns not Problems: Working with Intractable Issues Types of problems:
Stephen Powis, National Medical Director of NHS England “In uncertain times, the only known is that there will be change, and it looks like it will be YOU doing the leading!” Digital revolution: Not just AI, but intra-operability, health/medical data, wearables. Link to the global health agenda.Genetic revolution: Need masses of space. Currently leadership is seen as aposition for individualsrather than a behaviour for everyone. We must stop the unhelpful “I’m just a….” attitude and the notion of“Don’t get ahead of yourself there Dr. X, you don’t need to be doing that yet”. Leaders need to aim to regularly add value to the people around them, and everyone can do that, every day. “It will never be someone like me” But think “Control your own destiny” it needs to be done by someone, why not make it you? Read theBMJ Leaderfor leadership tips, research and evidence. Matthew Hancock – Health Secretary England The NHS needs a leadership culture change. We must stop apportioningblame but start really harnessing a culture of learning from mistakes. Anyone who says they have never made a mistake simply isn’t telling the truth. And the truth is at the heart of honest reflection, learning and moving forward. We want staff to challenge without fear and encourage complaints as these are opportunities to improve. Ideally, we want to give away the directive and hierarchical power and consequently empower all individual healthcare workers. This is what we are! This is where were going! This is how were going to get there! Ends with a challenge: What are you going to do? Tim Swanwick - Leadership in the Undergraduate Years “Leadership is a contact sport which brings about change. This cannot be done from the comfort of a desk or department headquarters. The key to developing leadership skills is to get outside of your comfort zone, that’s when you learn the most. Seek out opportunities and go for it. Lead the way to your own future.” “Management makes sure the ship is stable, Leadership sails it in the right direction.” It seems like it wasn’t too long ago where communication skills were thought of as innate. If you had them, you’d be a GP, if you didn’t then you’d be a surgeon or a pathologist (I jest of course but you get the point). Thankfully, at least for the past 15 years, medical schools have recognised that everyone needs to be taught these key skills and consequentially there have been significant improvements. Communication workshops with breaking bad news and explaining diagnosis and management plans have upskilled all doctors and made a massive impact on the care delivered to patients and their families. The tide is changing, leadership & management is being asked about in medical school interviews. Specific leadership skills curriculums are being introduced into universities across the country next year. “What if every newly qualified healthcare professional graduated thinking as a leader.” GMC document 2018 – “Outcomes for graduates”. 1stdomain in the curricula. https://www.ted.com/talks/angela_lee_duckworth_grit_the_power_of_passion_and_perseverance?language=en The science of Leadership & Management is not new. There are 15,000 members of the American Academy of Business who have been researching L&M for many years. The BMJ Leader could bring business school world evidence to medicine. His best advice: Go and get some honest feedback, it will be perhaps the most useful gift you will receive from a colleague?!? Try asking this… “Tell me one thing that I do which is negative?” It takes a degree of bravery for you to ask and reciprocal bravery for them to answer honestly as well. He also insists that we should all have mentors. One can have multiple mentors, e.g. a leadership and speciality mentor. They offer a sounding board for example, difficult interactions with a colleague. They can guide you and order your thinking. Consider the following as some of the more “formal” leadership opportunities: Other Resources: NHS Improvement: Developing People Improving Care Great project in Scotland: Project Lift: NHS Scotland https://www.projectlift.scot/ Diversity And Inclusion in Healthcare Do you know what the 9 protected characteristics of the Equality Act 2010 are? Do you know what “BAME” stands for? This was a really interesting session recognising that even if there is diversity in the workforce or patients, these groups may still lack full inclusion or equality. Leaders need to learn how to o address these issues and respond to unconscious bias. How to hear some difficult messages, and how to respond positively. All too often issues are not confronted as “Oh this is making me feel uncomfortable” or “Of course we’re not, that can’t happen here”. We all need to be “Power aware, Identity aware and Self-aware”. The mindset we embrace in the workplace that liberates other people. Often organisations only take a stand when it gets to “Discrimination” stage, as the lower levels are largely invisible to those not affected by it. We need to upskill leaders so that everyone is aware of what is happening, the behaviour is addressed sooner, everyone has the courage and permission to call out bad behaviour. Courage is the most important of all the virtues, without courage you can’t do any of the other virtues consistently. “The behaviour we walk past is the behaviour we accept” Barriers to successful inclusion:
“The only person I can change is myself, how I show up might encourage others to shift their focus, their attention and their behaviour” If you are reading this, you are part of the generation that can make the change! Malala Youssef – Nobel Peace Prize award speech– “Let this end with us” Richard Watson – Futurist: Mega Trends and Technologies2017-2050 It seems that Richard and many others who look to the future can only be sure on one thing, “it is UNCERTAIN and there will be many ways of doing things”.Now for someone who is highly paid for their predictions this seems like a great way of hedging your bets. He also highlighted the worrying change in society with the dominance of screen delivered information and a sedentary lifestyle. Previously children would have been told “behave or you will have to go inside!”, now it is the opposite! He described a world where devices know more about you than you do about yourself. Anybody who says they know exactly what the future holds is lying. However, we spend too much time worrying about it. We NEED to spend time as communities figuring out what we want to happen, using a proactive and positive mindset. It doesn’t matter if we are wrong. We must all have a collective vision of where we want to go, build narratives around the vision and step towards it. I agree with Richards aim of… “Every day waking up and trying to get better, making things better for ourselves and others” Another interesting person is Yuval Noah Harari: 21 Lessons for 21stcentury - interview Professor Megan Reitz: Professor of Leadership and Dialogue Speaking Truth to Power – Have a look for yourself here– it was an excellent 60 mins. Megan delivered a fantastic session about “That moment!” The one a person decides, shall I say something or not, and educated us on the act of “Speaking up”. All the scandals in healthcare organisations of recent times have something in common. People knew bad stuff was going on, but they didn’t speak up, and this resulted in patients coming to harm. One reason is the belief that it is always someone else’s responsibility and absolving oneself from responsibility. “They” aren’t speaking up, “they” need to show courage. Another issue is that often those very people who say the one time they did build up the courage and spoke out, they weren’t listened to and it made no difference. What if you experimented, what difference would it make at a collective level? Think about an occasion where you decided to say something, or not. Megan uses T.R.U.T.H to discuss the issues about these decisions. TRUTH: Trust, Risk, Understanding, Titles, How-to Trust: The value of your own opinion Risk: Realizing the risks of speaking up to powerful people and the ensuing struggle Understanding: Will I be perceived negatively, will I upset someone,“Will I belong”? Titles: We label inherently. Depending on the context, convey levels of authority How-to: Knowing what to say, when, how and to whom Megan then describes a number of traps and behaviours we all fall into which stop us from having the conversations we know we should have! Speak-Up Traps: We doubt ourselves – Imposter syndrome. Check the voice, notice when it comes in. Engage with it, am I going to listen to it this time. The Blind Spot: You will not listen unless you trust the value of their opinions. Can I empathise with how risky it might feel for this person to be speaking up? What titles do I have on me to affect what kind of information this person is telling me? Individuals ALWAYS think they are better at listening than other people. Listen-up traps: It’s easy to forget that no matter how lovely and approachable we seem as juniors, decades later, given some labels and titles, we are all quite scary. Make sure you don’t send“Shut up” signals and not “speak up” signals by knowing your face (and the rest of your body language signals, and environment you create). Today and every day, we make choices about what to say and when to stay silent. When we really help someone else to speak up or silence them. Choices feel mundane but if you add them up together it is what defines you. How you speak up and listen up represents the values you hold and the culture in which you work. If you think about it and act accordingly, you will change habits and change cultures. Some exercises and information to peruse at home in your own time! Exercise 1: Personal Values Think about your own values! What matters to you? How do you display your values at work? Much of the conflict at work results from a mis-alignment of core values. Spend some time writing down your beliefs. What behaviours demonstrate your values? None of these have anything to do with medicine or your background/grade. Exercise: Search for 50 personal values on the internet. Step 1: Make 3 groups of importance to you (High, Medium, Low) Step 2: Place each of the 50 values in a group Step 3: Take the “High” group and again split these into high, medium and low. Step 4: Group similar values together until you have 3-5 left. Step 5: Welcome to your values, enjoy them, be true to them, live them! Check out…Harry Kramer, Values in Leadership. One moves around the grid, depending on what is being demanded of us. Who else is there? Personal circumstances? Ideally there is a sweet spot (in Green) of moving around all areas, aiming to avoid the inept/donkey. How do you bring people and landscape together in your head and put it onto paper? Stakeholder mapping, mind mapping, network mapping. Another tool: Understanding people landscape map(Like Nike said… just do it) Length of the line: how far they are away from you Arrow direction: if you want them to be closer or further from you Dotted lines: are relationships you want to develop Small circles: /10 effort to build relationship (realistically) Stops: how far you want to bring them closer Wordsadd a narrative: Rich picture without words doesn’t show much Update it regularly, do it for different work groups. Use it for work networks, family situations, family events. For example, see diagram below: Do you know the 9 protected characteristics in the UK workplace? Age, Disability, Gender Reassignment, Marriage and Civil Partnership, Pregnancy and Maternity, Race, Religion or Belief, Sex, Sexual Orientation. A reflective exercise to do at the end of any teaching session, activity or experience. Take for example this blog (which I’ll admit has a lot crammed into it). Try and think of at least one behaviour in each of the following headings... Start doing: something you don’t do but think you should actively work to do more of. Stop doing: something you currently do but will actively try to do less of or stop doing. Continue doing:Something you are doing already but will do more of it because it works. Dr Chris Course The European Respiratory Society held their annual Congress for 2018 in Porte de Versailles conference centre, Paris. The European Respiratory Society is a non-profit organisation which aims to promote lung health and drive standards for respiratory medicine globally. In addition to publishing the European Respiratory Journal and educational handbooks, the annual congress is the largest respiratory conference in the world, covering topics on respiratory health and disease from fetal life to old age. Having registered months ago, (with an excellent discount on the registration fee for the honour of being under 40!) the congress program arrived in my inbox a few weeks ago, and to say it was overwhelming was an understatement. There were numerous concurrent sessions, across three floors of the conference venue, with special seminars and workshops on topics from non-invasive ventilation in adults, to bronchoscopy, lung ultrasound and inhalers for COPD. Having a paediatric/neonatal interest made it much simpler, as once you had filtered out all of the adult program, there was a manageable range of choices! The whole conference ran across four to five days, with the majority of the paediatric program running across the middle three days. The quality of presentations was high, and the speakers were clearly eminent in their field. Despite being a “European” conference there were speakers from across the world. I had gone with Professor Sailesh Kotecha and members of the research team at the School of Child Health, Cardiff University, and Professor Iolo Doull from the Paediatric Respiratory Medicine team in Cardiff. The first day we attended sessions on Prematurity and Lung Disease which included work presented by David Gallacher (Neonatal GRID trainee, Wales) from work he conducted with the School of Child Health at Cardiff University looking at pro-inflammatory cascades in the Preterm lung. Presentations also included work on Ureaplasma treatment for Preterms, animal models looking at effects of different durations of mechanical ventilation on long term alveolar structure and the Forced Oscillatory Technique for real-time assessment of preterm baby’s lung mechanics. The afternoon had an excellent Paediatrics Year in Review session looking at the top literature from the last year, the highlight of which was Dr Ian Balfour-Lynn (Royal Brompton, London) presenting the last year’s work on Cystic Fibrosis disease modifying drugs like Ivacaftor and Orkambi. The second day started with the Paediatric Grand Round where challenging cases and unusual diagnoses were presented and discussed, and this brought a good contrast to some of the talks from the first day on mechanistic and translational science. This as followed later in the day with a Lungs on Fire session where quick fire case presentations and questions were put to a panel of experts and the audience with the opportunity for us to vote along – this gave me confidence that some timers no-one knows what the right answer should be! Another session looked at the infectious causes of wheeze and asthma and our current knowledge in their manipulation. Talks included work on the microbiome of the upper airways, and our current evidence base for the treatment of pre-school wheeze, and it looks like Montelukast is out again! A running theme across the first two days was the quantity of work looking at azithromycin for the treatment of a range of conditions, and although lots of the evidence was convincing, I was occasionally left wondering if it’s the current fashionable treatment or a drug with further unexplored potential. The second day ended with the paediatric dinner, which started with a boat trip down the Seine, followed by dinner at the foot of the Eiffel Tower. This was a great evening and opportunity to escape the conference venue. As much as I enjoy a good conference, the inside of a presentation hall is pretty much the same wherever you are, and it was nice to get out and see a little of the City of Lights. Dinner was interesting (the starter consisted of a mixture of tuna steak and strawberries…) but so was the opportunity to meet new people from across Europe and the world. The last day (slightly tired!) we got in nice and early, mainly because our posters had to go up! After a coffee and a croissant, we headed to the first session on Prenatal Origins of Respiratory and Atopic Disorders which included data from the COPSAC (Copenhagen birth cohort) studies and animal models looking at how maternal smoking, and interestingly “vaping” may affect offspring into adult life. It also highlighted the scientific, economic and clinical difficulties in managing such large birth cohort studies and how replicating results can be challenging. Following this, we attended a session on Advances in Primary Ciliary Dyskinesia. This covered pathophysiology of this rare and little understood disease and highlighted how genetic are changing diagnosis. However, it was rightly pointed out after the presentations that, much as with Cystic Fibrosis, the phenotypic variance of these genotypes is still not clearly understood, and the continuing importance of expert interpretation of histological samples and formation of centres of excellence to manage this condition. We ended the ERS by having a walk through the exhibitors hall. There was a great ‘Game Zone’ where we could play with video laryngoscopes, bronchoscope and thoracic ultrasounds and it was great to have a go with bits of kits that we’d seen or heard about but had little experience with. Tutors were on hand thankfully to guide us through the finer details! We also had a look through the commercial and pharmaceutical exhibition areas, which looked more like a new car show at times (not sure a hologram is really required to advertise an inhaler) and there was a paucity of the free pens, but there were plenty of places to sit and have a quiet five minutes, which was much needed by this point! Overall, the ERS Congress was a fantastic experience. Definitely the best organised, highest quality, best value meeting I’ve ever been to, and would thoroughly recommend to anyone with a respiratory interest. Next year the congress is heading to Madrid, check out www.ersnet.org for more information
Faculty of Medical Leadership and Management Wales Regional Conference 2018 13th September 2018 Dr Rebecca Broomfield  While I have completed my year as a Welsh Clinical Leadership Fellow (Blog post teaser … more on that in Novembers posts!) I still very much have an interest in leadership and how we can rise to the current challenges facing the National Health Service. Therefore I was excited to learn that the FMLM were hosting a conference just up the road in Cardiff. It was a heavily packed program and the day flew by in a flash. The FMLM Chief Executive Mr Peter Lees spoke to us about the aims and targets of FMLM and how they plan to achieve this. He was followed by Wales' very own Chief Medical Officer Dr Frank Atherton who opened with "If we don't seize the opportunity as medical leaders …. who will?" He emphasised the need for whole system change not jus on an individual level and that as an NHS in Wales we do not simply need more. We need to harness ideas and bring them together. We need to keep patient safety at the centre of everything we do and bring those who resist change with us through the changes which need to occur. Following the CMO is always a tough gig but it was managed superbly by Dr David Samuel (A fellow Leadership Fellow Alumni) and Dr Sian Lewis. They reminded us of the need for diversity in the workplace and within medical leadership teams. They asked us to do a tabletop exercise to emphasise this point. Each member of the team picked a O or a X card. We were not able to tell each other which symbol we were. Then everybody shut their eyes and the X's were instructed to open their eyes and read the instructions. The task was to plan a holiday but to do so without giving any value or time to the O members of your table. Then the O's reopened their eyes and the task of organising a holiday was given to the table. I was an X. It was incredibly difficult to ignore and not give value to peoples suggestions. It felt awkward and non productive to an effective team working environment. The O's felt undervalued, and eventually gave up suggesting things and went off into their own discussion, effectively planning a whole other holiday. The exercise was trivial but raised a good point - are you really inclusive in your leadership? Do you consciously or unconsciously bias against somebody and importantly how does that effect the team. Post a quick coffee stop we heard from Mr Nigel Edwards (Chief executive, Nuffield Trust) about integrated care and Dame Clare Marx (Current Chair of FMLM, former President of the Royal College of Surgeons, soon to be Chair of the GMC and a dynamic powerful woman) She spoke about the importance of clinical leadership and the fact that we need to change. She suggested that we need to exchange hierarchy for connectivity and that clinical leadership can impact to increase quality, social performance and make financial gains. She believes that positivity has a big impact on your team and that we have a responsibility to coach clinical leaders and help people to develop themselves. Following this we had the unique opportunity to have a panel discussion on current leadership challenges and how we can embrace them and continue to move forward within Wales. We asked for their key Leadership message: Dr Frank Atherton - To use management experience from outside of Medicine and promote interdisciplinary working. Dame Clare Marx - The only thing you can control in life is yourself, the way you work and the way you behave. Understand what it is you have the ability to control. Mr Nigel Edwards - Connect what feels real, we are missing a narrative "tell a story" After lunch we were encouraged by Ms Katie Laugharne (Head of Welsh affairs at the GMC) and Dr Madhu Kannan (Current Welsh Clinical Leadership Fellow within the GMC) to think about Leadership expectations and impact. How the things you do day to day have an impact and how small things, like tea!, can really matter. We were encourage to think about how our leadership style was viewed by members of our teams and if that was the way we wanted it to be. After a quick coffee break we learnt from Mr Christian Servini about what the future generations act was enabling people to do in Wales and the impact this was having on Well-being. Then to end the day a quick fire 5 minute presentation round where we heard about improvement projects which were having an impact around Wales. My project (poster below) was one of those presented. If you are at all interested in Clinical Leadership I would encourage you to take a look at the FMLM website and consider going to the annual conference. Leaders in Healthcare details of this can be found here: https://www.fmlm.ac.uk/events/leaders-in-healthcare-2018
NH Gent Belfort Hotel, Ghent, Belgium 22-24th June 2018 Annabel Greenwood ST3 Trainee, Wales Deanery The 4th INAC was held in the beautiful and charming city of Ghent, Belgium. The INAC was established to provide a global platform for neonatologists and budding-neonatologists across the world to come together and share their work on the recent advances in neonatal medicine. This year’s meeting was hosted by the Belgian Society of Neonatal Medicine, led by their President, Professor Filip Cools. An exciting programme was awaited, packed full of brilliant talks delivered by highly esteemed neonatologists, and included a showcase of diverse abstracts from all over the world. Delegates attended from over 50 countries across five continents. The conference itself was perfectly situated, set upon a quaint cobbled street, running alongside the iconic canal that winds its way through the vibrant city. From a personal perspective, I was extremely excited to present my work on organ donation on an international stage. Organ donation in neonatal medicine remains a fairly new concept, and I felt privileged to have the opportunity to fly the flag for organ donation, raising awareness and sharing my knowledge and experiences with others at such a prestigious event. I was fortunate enough to be joined by my colleague and friend, Dr Chris Course, on the trip, who was presenting the WREN Project we collaborated on with Dr Zoe Howard, on postnatal antibiotic use across Wales. Our project fitted in perfectly with one of the principal themes of the conference, namely antibiotic stewardship. There was a particular emphasis on neonatal neurology over the course of the weekend, and it was fascinating to learn of the latest developments in such a complex and challenging field. Professor Jose Honold discussed the concept of a ‘Neuro NICU’, a collaborative approach between neurologists, neonatologists, radiologists, neurosurgeons, neurophysiologists, and specially trained neonatal neurology nurses, using specialised equipment to optimise the management of conditions such as high grade IVH, meningitis and encephalitis, seizures, HIE, and those with congenital cerebral malformations. Another highlight was learning about the recent advances in neonatal lung ultrasound by Dr Luigi Cattarossi, to help guide the diagnosis and management of a number of lung diseases including RDS, TTN, pneumonia and pneumothoracies. This quick and focused bedside diagnostic approach has been shown to be as reliable as CXR in demonstrating lung pathology, resulting in less exposure to radiation for the neonate. It was also of great interest to learn about the challenges faced in neonatal medicine in developing countries, and demonstrated the importance of the implementation of simple interventions e.g. bubble CPAP, in making a huge difference in the survival of preterm infants with respiratory distress. Aside from the conference, there was plenty of time to relax and explore the local delights of Ghent. The city was electric as fans set-up camp in the square to cheer-on their country in the Football World Cup! I certainly enjoyed sampling the local delicacies, Belgian waffles being a particular highlight! As the weekend drew to a close, I reflected on what had been a truly fantastic conference. The INAC 2018 provided an excellent platform for learning and certainly inspired new project proposals and ideas to take back to Wales! Next year's conference is planned to be in Tijuana, Mexico with a pre-conference in San Diego, so a little further afield, but another couple of top destinations for sure!
Princess of Wales Hospital, Bridgend, Friday 8thJune 2018 Annabel Greenwood Paediatric ST3 Trainee Broadly speaking, I feel our exposure to safeguarding training in the early years of paediatric training is limited.
Before you know it, you are the registrar on-call, out of hours, contacted with a complex child protection referral. As a junior paediatric trainee about to transition to middle-grade training, I will inevitably at some point, be faced with this scenario, and if I’m to be completely honest, the thought has previously caused a slight degree of tachycardia, hyperventilation and perspiration on my part, at the uncertainty of such a situation! I therefore searched for a way to dispel my fears and came across a child protection simulation course set-up by Dr Emily Payne, ST8 Community Paediatric Trainee in Wales. This fantastic one-day, multiagency simulation course has certainly enhanced my confidence in the management of child protection cases and I would certainly recommend the day to my fellow trainees. The course facilitates approximately 6-10 trainees, a perfect sized group to allow plenty of opportunity to ask questions and share our experiences with each other. The day began with a couple of short lectures, setting the scene for the day, addressing some key safeguarding principles, including the rights and responsibilities of all doctors, and an outline of the child protection process. We also discussed the ‘ACE’ (Adverse Child Experiences) Study, which has demonstrated that for every 100 adults in Wales, 47 have suffered at least one ACE during their childhood, and 14 people suffered 4 or more events. ACE are stressful experiences occurring during childhood that directly harm a child e.g. sexual, physical or emotional abuse, or effect the environment in which they live e.g. domestic violence, mental health, parental separation. It has been shown that ACE impact across the life course, e.g. affecting neurodevelopment in the early years, potentially causing social, emotional, and cognitive impairment, and perhaps leading to the adoption of high-risk behaviours and crime later on in life. Later in the morning we divided into pairs for 3 workshop sessions focusing on physical, emotional and sexual abuse respectively. These informal, small-group workshops were based on a clinical scenario and provided an excellent opportunity to voice any queries or concerns we had regarding the different categories of abuse. In the afternoon, we worked through a number of simulation child protection scenarios with actors playing the role of the child’s parents, making the situation as realistic as possible. At the end of each scenario we re-grouped to provide feedback and discuss the case in more detail. I felt that this was a completely safe environment to practice leading challenging safeguarding scenarios, and found it extremely useful to receive constructive multiagency feedback, from doctors, social workers and the police. The day was brought to a close with a simulated strategy meeting, and we all played the role of a different member of the multiagency team. This provided a fantastic insight into the role of each member of the team, and demonstrated how everyone works together to collate the evidence in order to generate an accurate account of events, to ensure the safety of the child. I thoroughly enjoyed the course and feel that I will now make the transition to middle-grade training with enhanced knowledge and confidence to manage challenging safeguarding scenarios. 22nd June 2018, Swansea Marriot Hotel Gill Smith, ST4 Paediatrics Trainee, Wales Deanery The spring 2018 WPS meeting was held in a very sunny Swansea. The sun shone down on the beach next to the Marriot hotel which provided a beautiful view during breaks between some excellent presentations and some very thought-provoking talks. The morning presentations were on very varied and interesting topics, which included audits and quality improvement projects from medical students, paediatric trainees and consultants. Presentations from neonatology to general paediatrics meant that there was something for everybody. I particularly enjoyed the presentation by the co-host of the WPS meeting, Dr Carol Sullivan who spoke with enthusiasm and wit about writing a student textbook in paediatrics. It looks like it will be a hit. Just before coffee, we were delighted to see Dr Peter Dale adorned in a bright pink wig and pink cape to highlight and talk about the approaching change to the RCPCH curriculum-progress. He went pink for Progress. Details can be found on the RCPCH website. More fantastic presentations ensued after coffee and the morning session was rounded off with a presentation on the problems encountered by babies born in the late pre-term period. Often thought to be close to term that physiologically they would be similar to those babies born at term. Evidence suggests this is not the case and is certainly gave us food for thought prior to lunch. A brilliant and tasty selection of food was available for lunch, finished by coffee and a chance to chat with the exhibitors. The lunch break was also a great opportunity to pop outside and enjoy the glorious sunshine and beautiful views overlooking the mumbles. After lunch we were kept from any thoughts of postprandial sleepiness by another set of wonderful and stimulating presentations. The first lecture back, presented by Dr Sheena Durnin was perfectly timed about of the use of paediatric pain relief practices in emergency departments in the UK and Ireland. These practices were evaluated across 40 hospitals in the UK and Ireland. It found a wide variety of practices in terms of analgesia used, timing of analgesia policies, and availability of play specialists to name a few. Dr Durnin earned the award of best presentation. Congratulations! Next up, another award winning presentation by Dr Rachel Morris who spoke so eloquently and with such passion about the implementation of family integrated care in a tertiary neonatal unit. The results were encouraging in that since the introduction of Family integrated care there had been an increase in breast feeding rates and a reduction in the length of stay and an anecdotal feeling that parents felt more in control and were ready for discharge sooner. Dr Morris won the best trainee award and this was thoroughly deserved. Following another round of superb presentations, the mid afternoon session was rounded off with an absolute gem of a talk from invited speaker Dr Mark Stacey, consultant anaesthetist and Associate Dean in Cardiff and Vale NHS Trust. The talk entitled ‘A Bakers’ Dozen Resilience Skills’ got us up and thinking. We had to write ourselves thirteen points to aid us in our resilience at work and life and included sleep, meditation and taking care of yourself. Some very important points and recommendations made. This talk left many feeling invigorated and gave us something to talk about during the afternoon tea break over coffee and cake before the late afternoon session. Fuelled with caffeine and carrot cake we had a further four short quick fire talks and the day was completed with a guest lecture from Dr Michael Farquhar, Consultant Paediatrician in children’s sleep medicine at Evelina Children’s hospital. His talk entitled “Rounded with a sleep: Why We Need To Talk About Fatigue” discussed the importance of sleep and gave a convincing argument for the need for all of us to sleep well. Night shift workers are encouraged to take power naps as this will improve our senses, judgement skills and general wellbeing. This talk went beautifully well with the Resilience talk and is definitely something we should all try and think about. Driving tired can be as bad as if driving after drinking alcohol. We made our way to the beach to enjoy the rest of the sunshine before a delightful dinner with colleagues and friends. A lovely end to a fantastic day.
Once again the WPS conference was a great success, showing a very talented bunch of people. It was thought-provoking and inspiring and a great way to meet up with colleagues and brilliant guest speakers. I’m off to get some sleep before the winter meeting (I prescribed it to myself)! Guest post from Dr Laura Potts, Clinical Leadership Fellow, Paediatric Trainee, Wales Deanery The Medical Women’s Federation (MWF) was founded in 1917. They aim to advance the personal and professional development of women in medicine, to change discriminatory attitudes and practices and to work on behalf of women patients and their families.
This year’s spring conference in Cardiff covered a broad range of topics affecting women from living and working with a disability through to antenatal screening and management of HIV. The first talk ‘Prenatal testing ; risks or certainty’ was given by Dr Annie Procter, Consultant clinical geneticist. She discussed the evolution of antenatal testing and its future directions. The potential scope of antenatal screening is vast, especially with the introduction of fetal DNA analysis in maternal blood, but routine screening is currently limited to the three major trisomies. This thought provoking talk advised caution; should we test for everything we can, just because we can? It also highlighted the importance of managing families expectations effectively. Dr Olwen Williams spoke about the progress in HIV and AIDS management in recent years. Huge advance have been made and are now close to enabling affected women to have normal deliveries and breastfeed. Women are however, still presenting with late disease and later in life, with and opportunistic infection and Kaposi sarcoma. She also reinforced the results of the recent PARTNER study which showed that in those with an undetectable viral load, transmission to their partner did not occur. There is a new public health initiative promoting Undetectable = untransmissable. There were also a number of abstract presentations. Of particular interest was the work being done at Singleton neonatal intensive care unit on family integrated care (FiCare), presented by Dr Rachel Morris (ST5 Paediatric trainee and trainee representative for the MWF in Wales) . Family integrated care is centred around four main themes – staff education, parent education, creating the right NICU environment and providing psychosocial support. The concept originated in Estonia and was developed by Professor Lee and colleagues in Toronto. It has been shown to reduce length of stay, retinopathy of prematurity and infections and increase breast feeding rates. Singleton have already had a lot of success, receiving excellent feedback from families and demonstrating reduced length of stay and increased breast feeding rates. During the afternoon there were a number of workshops. I attended Dr Cora Doherty’s session on wellbeing and the healthy team. For optimal team effectiveness and performance mind, body and spirit must be considered, that is to say the team needs a clear vision, good morale and trust and have their physical needs met. The concept of the ‘fitness’ of team members to be part of the team was also considered and how we as team members and leaders have a responsibility to protect our own wellbeing and that of our team. During the remainder of the afternoon there was an interesting talk titled ‘menopause behind the headlines’. Whilst not particularly relevant to our patients it was a delightful insight into what some of us have to look forward to! Dr Clarissa Fabre, President elect of the Medical Women’s International Association (MWIA) shared the results of the most recent MWIA members survey. This included some worrying statistics such as 57% of respondents felt that they had been discriminated in their career, with 41% reporting that they had experienced sexual harassment or bullying in relation to their work. Unfortunately younger doctors reported lover job satisfaction, more sexual harassment and bullying and a higher incidence of stress and burnout. The conference ended with the Dame Hilda Rose lecture, given by Dr Sally Davies, focusing on the importance of stories such as Dr Frances Morgan’s. She was the first woman to receive a doctorate in Medicine in Europe and the first female doctor registered in Wales. She was a pioneer in medical practice and social reform, working all over the world as well as working as a General Practitioner in Wales. These stories demonstrated how far women have come in achieving gender equality but that there is more work to be done, as highlighted by the recent MWIA survey. The MWF work hard to fight discrimination against women in medicine, for example, challenging Jeremy Hunt on the lack of impact assessment for the new junior doctor contact in England and helping to tackle the gender pay gap. An interesting quote was offered at the end of her talk, ‘good practice benefits all, bad practice affects women more’. I wonder what you all think of this? The key messages from this lecture and the conference in general were that huge progress has been made by women in medicine and in women’s health and that we all have a responsibility to report and challenge bad practice and behaviour, and make looking after ourselves and each other a priority. For anyone interested in finding out more about the MWF their website can be found at www.medicalwomensfederation.org.uk Dr Tim Warlow, Paediatric Palliative Care GRID trainee, Wales Deanery Few of us can forget recent cases in the press of Alfie Evans and Charlie Gard. Such tragic cases of breakdown in relationship between families and care teams. I’m sure that alongside my own cries you have had the thought ‘Surely things didn’t have to get to this!’ These cases bring into stark clarity the importance of our skills of communication and our ability to put into practice the ethical and legal duties to involve of families and children in decision making. These cases are nightmare scenarios, but at some points in our career we will face similar challenging situations. Aware of these issues, the All Wales Paediatric Palliative Care Team received £20,000 of Welsh Government funding to improve the skills of paediatricians in these areas. Our response was to organise a series of free workshops exploring issues of ‘communicating difficult news’, decision making and advanced care planning in paediatrics. April 2018 saw the first of these workshops in the fantastic Copthorne Hotel, Culverhouse Cross. Within a month we had filled all our places and the response on the day from delegates was fantastic. The truly multidisciplinary event was attended by consultants, community nurses, therapists, trainees and hospice staff, all of whom engaged amazingly in communications skills breakout groups and seminars. There was time to explore advanced communication skills, read and use the Paediatric Advanced Care (PAC) Plan, and consider the views of families and young people in planning. The highlight of the day was without a doubt an interview with one of our parents whose son sadly died under the care of our service. She discussed the value of good communication, of doctors being prepared and sensitive, and the benefit of early and co-ordinated planning.
The good news is that there are several further days being organised, one for each of the health boards in Wales. The next of these is in Swansea where Dr Griffiths will be using trained actors to facilitate what will be an exhilarating day of interactive learning together with other professionals. Please contact [email protected]for further information about upcoming days and to sign up. All workshops are free of charge and are in great venues with food provided. If doing a good job of communicating and parallel planning with families excites your interest, these days are for you. If you want to run a mile, these days are even more for you! Let’s get to grips with the really difficult stuff of paediatrics, lets help families to live well and for those whose lives are cut short, to live well right to the end. by Chris Course, Chair WREN Summary
The Welsh Research and Eduction Network (WREN) Spring Study Day took place at the Princess of Wales Hospital, Bridgend on 11th May 2018. Once again, attendance was well supported by doctors from across the training grades (and an Advanced Neonatal Nurse Practitioner!), as well as Dr Huma Mazhar (from Singleton Hospital), Dr Naomi Simmons (from Glan Clwyd Hospital) and Dr Judith van der Voort (Head of School) joining us for the day to learn more about how the network is getting on and our current activities. Our educational programme was once again diverse, with talks from Dr Phil Connor and Rhian Thomas-Turner about the new Children and Young Adult’s Research Unit at Noah’s Ark Children’s Hospital for Wales and their plans for increasing junior doctor involvement. Dr Ian Morris then gave an excellent strategy for rapid-fire critical appraisal, with an emphasis on the START assessment (slides available on our website, or on request). Dr Gethin Pugh from the Quality Improvement Skills Team at the Wales Deanery also gave us an introductory workshop to Quality Improvement, as well as teaching us the basics of the Plan, Do, Act, Study model and signposting the further QI training opportunities available. The WREN Blog continues to go from strength to strength and now receives over 500 hits a month on our articles, under the editorial leadership of Dr Rebecca Broomfield and Dr Annabel Greenwood. They are looking for contributors too, so if you have something to share or a topic you’d love to write about, please get in touch. Four new projects are being undertaken via the network, three of which are starting now. Details of the WREN projects and their project leads are below. Project leads can be contacted on the Current Project Portfolio page. We will be disseminating these projects amongst the units, but if you would like to get involved in any of the projects in WREN’s current portfolio, please contact the project leads (details below). If you have an idea for a project you would like to develop with WREN’s help, please contact either myself or Siwan Lloyd via our website, or using the details at the top of this newsletter. The next WREN study day is planned for November 2018 (confirmed date to follow), and we hope that you will be able to join us for another stimulating and thought-provoking study day, building on from the success of the last! Newly Launched Projects Project Title: ‘The Impact of the Meningococcal B Vaccination on Septic Screens’ Project Leads: Dr Ele Jones (ST5) and Dr Rebecca Towler (ST5) Description: Pyrexia is a common adverse effect of the Meningocccal B vaccination. NICE guidelines exist for the management of fever <3 months of age and recommends investigations for sepsis for pyrexial infants but does not make comment of post-vaccination infants. This project aims to retrospectively assess how infants are managed in paediatric and neonatal units who are presenting with fever post-Meningococcal B vaccination over a 12-month period. Project Title: ‘Aiming to improve paediatric trainees confidence with ECG interpretation’ Project Leads: Dr Ankita Jain (ST6) Description: The Paediatric Cardiology department at UHW gets several referrals a month from various hospitals to provide their opinion on ECGs done on children for various clinical indications. We would like to help improve confidence in paediatric ECG interpretation, and have developed a structured online educational module. Using a pre- and post-quiz on ECG interpretation it is hoped to show how skills can be improved. The link for the quiz is https://goo.gl/forms/2Qj8NBZHBdOYL33d2 Project Title: ‘Can a resus drug App help improve accuracy and reduce stress in time-critical scenarios?’ Project Lead: Dr Jordan Evans (ST5) Description: Accurate calculation of WETFLAG resus drugs is critical, but can be affected by stress and the time-critical nature of emergency scenarios. This project aims to assess whether a smartphone app can help to improve prescribing accuracy and reduce doctor stress levels in resus situations. A pilot study has shown an App to be effective, and this project aims to assess larger numbers of doctors and nurses using the technology in simulated scenarios. Ongoing Projects Project Title: ‘Head injuries on the postnatal wards’ Project Lead: Siwan Lloyd, ST3 Description: A pilot study at UHW has demonstrated that infants being accidentally dropped on the postnatal ward is not an uncommon occurrence, however their management and level of investigation following injury was very variable. Following on from this, an all Wales study is underway to determine the incidence, risk factors and management used, with the aim of producing a best practice guideline for these infants and their parents. Project Title: ‘Re-audit of the Management of Respiratory Distress Syndrome in Preterm Infants’ Project Lead: Chris Course, ST4 Description: Following the initial audit in 2014/2015 by WREN, a Wales Neonatal Network guideline was introduced for the Management of RDS in Preterm Infants in June 2016. The re-audit has commenced March 2018 and is running for six months to assess how the new national guideline has affected patient care. Project Title: ‘Management of feverish illness in infants <3 months old’ Project Lead: Blanche Lumb, ST1 Description: Do we consistently meet the NICE standards set in the investigation of sepsis in <3 month old infants? This project aims to assess that the appropriate investigations occur in a timely manner, and that appropriate empirical treatment is commenced across paediatric assessment units in Wales. Where we chose to deviate from the guidance, are we documenting this appropriately? Upcoming Projects (Planned Start September 2018) Project Title: ‘Evaluating the impact of the introduction of the SEREN program on Type 1 Diabetes Management in Children’ Project Lead: Matthew Ryan, ST6 Description: SEREN is a structured education package for children newly diagnosed with T1DM. This project will assess SEREN’s impact by using Quality of Life questionnaires, serial HbA1c measurements and number of DKA admissions for children diagnosed with T1DM in the years pre and post introduction. Guest blog post by Dr Kimberley Hallam I’m an ST2 in paediatrics and unfortunately did not have the chance to attend the RCPCH conference last year. So, this year I was very excited when I realised, not only would I be able to attend for all 3 days, but it was also in Glasgow…a city which I love and where my twin sister lives. Getting up to Glasgow itself was challenging! I travelled up after work on the Wirral on Monday night. Soon after leaving, there was an announcement that there were trespassers on the line. Unfortunately, this meant I didn’t arrive at Glasgow Central Station until 00:45! Luckily, I was staying with my sister so didn’t have the hassle of a late night check in. DAY ONE Day one of the conference was entitled the ‘Science and Research’ day. Because of my late arrival to Glasgow, I didn’t attend the 8am ‘Personal Practice Sessions’, but started at 9am with a welcome from the (now ex-) President of the RCPCH, Neena Modi. During the course of the conference, she relinquished her presidential title to Russell Viner. She gave an eloquent opening talk which was followed by a presentation by the RCPCH & Us Network. This is a group of young people who work with the RCPCH to ensure that young people’s views are listened to in all matters within the RCPCH organisation. They spoke incredibly well and are clearly a group of passionate, intelligent young people who are forward thinking, keen to bring about change and ensure their voices are heard. Another highlight from the morning included a talk by Prof. David Archard regarding children and parental rights. He took examples from recent high profile cases and presented ethical considerations regarding parental rights. He focussed on a public slogan taken from the Charlie Gard Case: ‘My Child, My Choice.’ After a fascinating discussion, he concluded that ‘disagreements [between medical staff and parents] will continue and [will] probably proliferate. Parents’ feelings and views count but they are not decisive.’ He closed the session with the remark that ‘we live in a time of post-truth and populism.’ Next came an interesting presentation from Dr Cherry Alviani and was entitled ‘Sleep for your own health: A Pan-UK Survey on Paediatricians Experience of Sleep Around Shift Work.’ She talked about a survey she completed which showed a lot of trainees do not have training on how to manage sleep around night shifts and that many hospitals do not provide somewhere for trainees to sleep on night shift and/or do not support them doing so. Given lack of sleep affects judgement and clinical performance, these are important issues to address. As an aside, the BMJ have recently published a brilliant article which gives general advice on how to survive night shifts and which I have personally found quite useful: http://www.bmj.com/content/360/bmj.j5637.full After the plenary session, I attended a workshop entitled ‘Press, Politics and Paediatricians; Campaigning for Child Health Across the UK.’ This was an interactive workshop and even had some role play where members of the audience acted as news reporters and grilled (a pretend) Jeremy Corbyn and Jeremy Hunt. Suffice to say, this became a little heated! Overall, the session introduced the idea that it is our duty as paediatricians to be advocates for child health. This may include being politically active (e.g lobbying government) or may involve speaking out on behalf of paediatricians/children in the press. The RCPCH have opportunities for members to become involved in such work on their Press and Parliamentary Panels (they include free training). I’ve put this link here so you can have a wee look if you’re interested: https://www.rcpch.ac.uk/news/membership-benefit-month-media-and-parliamentary-training The last session of the day I went to was run by the British Association of Paediatricians of Indian Origin (BAPIO) and covered ‘Hot topics in paediatric subspecialties.’ They had a number of insightful and interesting talks including ‘When do you need a gut specialist?’, ‘Chronic cough: when is it a cause for concern?’ and ‘Changing landscapes in paediatric epilepsy.’ They also had talks from Neena Modi and Russell Viner (who got a bit of a kind-hearted grilling from the audience after his talk ‘Paediatric services: fit for the future’. I chose not to go to the meal out on the first night. Instead, I went to a fabulous place in Glasgow called Stravaigin with my sister and a Mersey trainee. It comes highly recommended! DAY 2 Day two of the conference was the ‘Global Child Health Day’ and, I have to admit, the day I was most looking forward to. It did not disappoint. The day kicked off at 8am with a session on how to include global health in your career which was delivered by a diverse group of trainees who all had experiences of working in global health during their training years. They introduced the variety of ways a trainee can take part in global health work. These include clinical work, teaching, quality improvement projects, research and public health. The session covered considerations such as the stage of training you should aim to do such work, what support you might receive and where you can do the work. They also talked about the courses you can go on to help prepare. For example, ETAT, CHILS, GIC and the Diploma of Tropical Medicine and Hygiene. I left this session feeling very inspired and excited about my potential future opportunities. Next up was the plenary with the first person to speak Prof Anthony Costello (Director of the Department of Maternal, Child and Adolescent Health, World Health Organisation). He gave a keynote speech on ‘Global governance for child health and sustainable development.’ As his title suggests, he came across as a very inspirational person. He questioned ‘is everything getting better?’ He stated that, globally, child mortality is improving rapidly and maternal mortality is improving but not to the same extent. As currently projected, low income countries will not catch up with higher income countries for a great number of years. Globally, we are still falling short in harder to reach areas and there are still basic health needs which are not being met. For example, lack of access to clean water and sanitation. Five key problems which act as a barrier to improving child health are as follows: 1. Fragmentation of global child health strategies undermines programming and limits impact 2. Child health goals will not be met without adequate funding and delivery to marginalised populations 3. Evidence is not systematically generated and integrated into policy and programs 4. Strategies are insufficiently tailored to country context, and tools need improved end-user design 5. Lack of accountability, clear targets and strong monitoring He then went on to describe five key areas for WHO and UNICEF to address. The next talk was regarding child refugee health and is something I have been interested in for a long time and passionate about since attending the Royal Society of Medicine’s study day ‘Child Refugee Health: Everyone’s Responsibility.’ Dr Marylyn Emedo presented data on ‘Adverse experiences of Unaccompanied Asylum Seeking children (UASC) and the impact on their emotional wellbeing and mental health needs.’ As a bit of background, there were 3290 unaccompanied asylum seeking children in the UK in 2016. Children from Afghanistan, Albania and Eritrea formed 48% of all UASC in 2016. Her study was a retrospective review of records of all UASC referred to a clinic run by a local authority in London between 1st January to 31st August, 2016. The study focussed on adverse experiences the children went through on their journey to the UK. It found that 51% of children experienced trauma on route to the UK including detention, beating, torture and sexual assault. All the children in the study were screened for mental health needs. Of these, 75% reported at least one symptom suggestive of PTSD, anxiety or depression and 43% accepted a referral to CAMHS. Her recommendations were for timely review in line with statutory guidelines and initiation of early support by mental health services. Next, the workshop I chose to attend was ‘What should RCPCH’s global health priorities be?’ This started with a talk outlining some stark facts: 98 of every 100 children who die <5 years, die in developing countries, mainly from avoidable/treatable causes. There has also been a shift of mortality from communicable to non-communicable diseases. There followed a discussion surround how to address these issues as we work towards the Sustainable Development Goals (SDPs) set by the UN (http://www.un.org/sustainabledevelopment/sustainable-development-goals/). There was participation from the audience and good engagement from the RCPCH. I was particularly happy to hear that the RCPCH are launching a global health professional development framework to run alongside paediatric training in order to engage trainees in global health work. I continued the global health theme by attending the International Child Health Group’s afternoon session. This took part in the main Clyde auditorium and was mainly delivered by people who had conducted projects related to international health. The first talk was delivered by Dr Jonson and was entitled ‘The validation of transcutaneous bilirubin as a method to monitor newborn jaundice in a low income country.’ She had recognised there were significant problems with babies developing kernicterus as a result of untreated jaundice in Haiti. Despite having a reasonably small data set, her study suggested that transcutaneous bilirubin monitoring was a safe way of measuring bilirubin in a low income country. The unit she was working on had a lower incidence of kernicterus following the trial. However, she suggested a larger data set would be required to fully validate her findings. Amongst the remainder of the afternoon talks, the one which stood out for me was given by Dr Christopher Hands and entitled ‘Delivering nurse-led emergency paediatric care in Sierra Leonean Hospitals: The effect on quality of care and mortality.’ This nurse-led care involved the introduction of triage systems, stream-lining the patient journey at the point of care and training nurses in ETAT. These basic interventions had resulted in a very impressive reduction in mortality. Anecdotally, nurses now recognised they had the skills to save the lives of individuals presenting with symptoms they previously thought they could do nothing for. For example, hypoglycaemia and seizures. Other talks included ‘Neonatal outcomes from FGM/cutting in the Gambia; results from a multicentre prospective study’, ‘The use of satellite clinics in W Uganda to remove barriers to seeking care’ and ‘Identification of the health burden for street children and service provision available in Kismu, Kenya, through Focus Group Discussions.’ At the end of the second day, I was exhausted. However, thanks to this day and the enthusiastic way in which the RCPCH approach global health, I now have a renewed determination to pursue a career in this area. DAY 3 Day three was entitled the ‘Health Services for Children day.’ The plenary in the auditorium started with a keynote speech from Prof. Jason Leitch, the National Clinical Director from Scottish Government. He was a very entertaining and enthusiastic speaker and it really was a pleasure to listen to him in his home city of Glasgow. He talked about the state of child health inequality in Scotland. He described how children living in Glasgow within a few miles of each other have a very different life expectancy (a phenomenon which is termed the ‘Glasgow Effect’). He then went on to talk about various local programmes which had been set up. For example, a programme in which fathers in prison are given intensive parenting classes and have their children visit the prison regularly. This even involved the inmates performing a play of the Gruffalo for the children and has the benefit of decreasing their chance of reoffending. There have also been programmes which involve intensive health visitor input. He ended with the following picture. After the plenary and a short refreshment break, it was time for the final workshop session. As I seemed to be developing a political interest as the conference went on, I decided to attend the session ‘Child Health Policy Development: Why, What and How?’ This started with a presentation regarding the RCPCH health policy strategic direction for 2018. This states that the RCPCH wants to achieve the following:
1. To prioritise the health needs of infants, children and young people 2. To prevent ill health and promote health and wellbeing 3. To ensure continuous improvement in the quality of healthcare services 4. To reduce child health inequalities They plan to achieve these aims in the following way: 1. Developing robust, evidence-based policy 2. Prioritisation and horizon scanning 3. Understanding the environment we work in 4. Influencing the right decision makers, at the right time 5. Having a tailored approach so the right messages reach decision makers across the UK After the presentation, there was a discussion with audience participation and engagement from the new president. We discussed why and how the RCPCH develops policy, its impact and the role of paediatricians in influencing decision makers. We concluded that, as paediatricians, we have a duty to advocate on behalf of children and young people and part of that involves lobbying to push child health up the political agenda. Following the workshop and lunch, I decided to start the first part of the afternoon with the ‘Children’s Ethics and Law Special Interest Group’ (CHELSIG). After an introduction to CHELSIG, there was a presentation ‘Children’s rights, UK healthcare and Brexit: Could things get worse for young people?’ This session discussed the UN rights of the child, including Article 16 (the views of the child), Article 24 (health and health services) and Article 16 (young people have the right to a private life). According to a study completed by the NIHR, 57% of children felt they were not involved or only involved a little in their care. This session encouraged paediatricians to involve children in decisions about their care and consider facilitating groups where children and young people can provide input into the running of paediatric services. The next session was called ‘Moral distress, trauma and burnout in staff in relation to changes in PICU outcomes, challenging cases and media involvement in disagreements about end of life care.’ This session was led by Gillian Coleville who had studied the impact of the above in Great Ormond Street staff following the Charlie Gard case. The staff highlighted their main sources of distress are being accused of not caring, public condemnation without the right to reply, fears for their own safety, witnessing a child’s suffering, protracted legal proceedings, impact on other families and constant changes to care plan. 15% of staff had features of clinically significant post-traumatic stress syndrome. I was quite surprised at how high this was and also found it distressing to hear how the case had impacted upon their private lives. The final session I went to on day 3 was one run by the Association of Paediatric Emergency Medicine. This was an afternoon focussing on the Manchester Arena bombing on 22nd May, 2017. We heard from Allan Courdwell, Head of Group Emergency Planning with the Northern Care Alliance who talked us through what happened on the day and how the trust managed the major incident. This was followed by an insightful talk by Fiona Murphy MBE, Associate Director of Nursing who covered the bereavement response after the bombing. She gave a moving description of how the bereavement officers supported those who suffered the death of a loved one. Her commitment to providing dignified support to the families was exceptional. She described various ways in which she co-ordinated and delivered the bereavement support. This included putting families up in a hotel together, having 24-hour access to a bereavement officer and finding out information regarding the victims so they could, for example, play their favourite music when families were viewing their bodies. She also arranged for the families to visit the arena (when safe to do so) where they had lit a candle where each of the victims was found so the families could further understand and come to terms with what had happened. This talk moved me and many others to tears and I was so overwhelmed by the dedication she and her team showed to support the families in the aftermath of the bombings. So, that concluded my first attendance at an RCPCH conference and I really enjoyed the experience. It was great to see how proactive the college came across in providing advocacy for children and addressing global child health. It was also fabulous to catch up with old friends and be inspired by projects which other paediatric trainees are undertaking throughout the country. I’ll definitely aim to go again next year! Guest blog by Dr Jemma Wright I was delighted to attend the first day of the RCPCH annual conference this year and here is a brief summary of my day. The day started early with a personal practice session about the new PROGRESS curriculum. Hopefully you are all aware of this new curriculum as it is going to be introduced this August. The session was an introduction to the new curriculum and it does seem like the college is trying to make it easier to engage with the new, much shorter curriculum. There is lots of information available on www.rcpch.ac.uk/progress including details of the mandatory 'key capabilities' we need to achieve and 'illustrations'/examples of how to evidence this on Kaizen. The main tip was to engage with this curriculum early as you can start producing evidence on your eportfolio now so it is already there to link to the new curriculum when it becomes live on 1st August 2018. The overall theme of the conference was ‘Children First – Ethics, Morality and Advocacy in Childhood’ and the main plenary had a strong theme on ethics.
The first keynote speech was about “Putting the Child First” and was an extremely topical philosophical exploration of the interaction between best interests and parental rights. There has been some significant media attention in the last year on multiple cases of disagreement between the medical teams and the parents. He alluded to these cases including the common protest of ‘my child, my choice’, and put a spin on this statement by highlighting that a parent does not necessary have the right to choose anything for their child – his example being that parents have the right to choose what to feed their child but they cannot choose to feed them poison. Overall it was an interesting discussion concluding that the child must always come first. This was followed by three project presentations: The first was on the impact of austerity on families with disabled children across Europe. The conclusion of the project survey was that cuts since 2008 have resulted in worsening quality and access of services to disabled children with a significant negative impact on families in the UK, especially those in severe poverty. The second was about delays in seeking legal judgements in cases of withdrawal of care, collecting data of 15 cases across the England over the last 5 years. They recommended considering alternative methods to avoid these delays such as mediation/dispute resolution, which have high success rates in avoiding litigation, and tend to have higher satisfaction rates. The last project was about a UK survey on paediatricians experience of sleep education. It was found that around 75% of paediatric trainees have not received any teaching on sleep during their training. Interestingly they recommended that we should all be taking a 15 min nap during our night shifts to reduce fatigue and that this should be supported by our workplaces. For more information, they have recently published articles in ADC and BMJ to promote more awareness about how to approach sleep during shift work. The plenary concluded with Professor Neena Modi talking about “Children in the 21st century’ focussing on the historical progression of a child’s role in society from possession, to protection, to partnership. She also talked about the increasing importance of non-communicable diseases in children especially childhood obesity and the interaction between child health and adult health. There is a whole section about these issues in the State of Child Health section on the RCPCH website. Next up, I chose to go to a workshop about navigating academic training pathways. As a non-academic trainee, it was interesting to hear that the college is keen to support paediatricians interested in developing an academic element to their job. I found out about a research funding opportunities database on the RCPCH website (https://www.rcpch.ac.uk/research_funding_opportunities) and the new academic toolkit (http://apatoolkit.eastface.co.uk). After lunch, I headed to the BPAIIG speciality group session. We had a presentation from an epidemiologist at PHE taking about paediatric antimicrobial resistance followed by a talk by a paediatric ID consultant about balancing antimicrobial stewardship since the new NICE sepsis guidelines. The key learning point when prescribing antibiotics was to be mindful of antibiotic resistance and always ‘Start Smart then Focus‘. There was a good representation from Wales in this session. I was asked to present my project about the epidemiology/microbiology of candidaemia over the last 15 years at Alder Hey Children’s Hospital followed by an excellent presentation by a Cardiff medical student looking at the risk of laceration when using an adrenaline auto-injector. There were also two further presentations about the impact of PCV on pneumococcal meningitis rates and two cases of INF a/b receptor 2 deficiency associated with immunodeficiency. Finally there were two further talks by paediatric ID consultants about the use of biomarkers to guide length of antibiotic course and the novel use of old antibiotics or new antibiotic combinations to treat multi-resistant bacteria. Excitingly there is a new national trial entitled BATCH (biomarker guided duration of antibiotic treatment in children hospitalised with confirmed or suspected bacterial infection), which is being coordinated by the Centre for Trials Research in Cardiff and may guide further developments in this area. Overall I had an excellent thought provoking day and enjoyed the excuse to visit Glasgow, my old FY2 home.  After the huge success of last year’s St David’s Day Conference, I was very much looking forward to this year’s event, and Abby Parish and her team once again certainly did not disappoint! Nestled in the heart of Wales’ vibrant capital city, a stone’s throw away from the iconic sites of Cardiff Castle and the Millenium Stadium, Park Inn provided a classy, yet relaxed setting for an exciting day of learning ahead. Greeted with a lovely warm beverage and a selection of delicious pastries on arrival, there followed an opportunity to catch-up with paediatric colleagues both old and new before the opening lecture of the day. The programme itself was particularly attractive this year, focusing on Ethics as the principal theme. On a personal note, I felt my knowledge of Ethics in Paediatrics was somewhat lacking, with minimal educational opportunities available previously to explore this complex but fascinating topic. I therefore jumped at the opportunity to attend this year’s St David’s Day Conference to broaden my knowledge and experiences. The introductory lecture was provided by the President of the RCPCH, Professor Neena Modi. This fascinating lecture on the ethical issues in neonatal research emphasised the importance of the positive relationship between parents/patients and the medical profession, to enhance understanding about science and research methodology, whilst simultaneously strengthening trust between both parties. Professor Modi also discussed the concepts of ‘opt-out’ consent and mention of a possible ‘inclusion benefit’ in order to improve recruitment and efficiency of Randomised Controlled Trials. The next lecture was one of three of the day by Dr Richard Hain, Consultant and all-Wales Clinical Lead in Paediatric Palliative Medicine. His ‘Introduction to Parental Authority’ talk gave an excellent insight into the difficulties often faced concerning parents’ influence on treatment and care decisions. He talked about the concept of “best interest,” discussing the differences between objective and subjective interests, and their importance in helping parents choose ‘the path of least regret’ with regards to treatment decisions. Before morning coffee there was a case presentation session led by Wales Neonatal GRID Trainees Kate Burke and Zoe Howard. Their experiences of the management of three different babies born with Trisomy 18 highlighted the variability of genetic diagnoses, the postnatal role of perinatal palliative care, and the central role of the parents. The final session of the morning featured a lecture on prenatal screening and the associated ethical dilemmas, by Professor Angus Clarke, Clinical Geneticist in Wales. He discussed the goals of antenatal screening programmes, particularly focusing on the permission of informed reproductive decisions, conveying ‘reproductive autonomy,’ whilst considering the balance of health economic assessments. Dr Hain brought the morning session to a close with his lecture on ‘the value of a short life, who decides?’ This was an extremely thought-provoking session discussing the rights of the fetus, and the value of a child, particularly focusing on the views of the parents and that of the law. The afternoon session, entitled ‘Costly care – because you’re worth it,’ focussed on the legal aspects of a number of ethical dilemmas, including reference to the relevant articles of the European Convention on Human Rights. The legal concepts were presented by Dr Rim Al-Samsam, Consultant in Paediatric Critical Care Medicine, who has a special interest in law in the context of healthcare. Dr Richard Hain then chaired an open session alongside Dr Al-Samsam, encouraging audience participation to discuss potential treatment dilemmas faced in a hypothetical case. Following an incredibly profound and inspiring day, the CEO of the RCPCH hosted an interactive ‘road-show’ to discuss some of the topical issues faced by the RCPCH and their potential plans to improve them. Also discussed was the exciting new RCPCH curriculum, due to be launched over the coming weeks. If you are yet to attend a St David’s Day Conference I could not recommend it more. I very much look forward to next year’s instalment already! Annabel Greenwood
Paediatric ST3  3rd-5th January 2018, Siwan Lloyd I had the pleasure of being able to attend the British Paediatric Neurology Association Annual Conference this year held at King’s College London. Despite a horrendous viral illness over the festive season which left me with significant post-viral fatigue, I managed to catch my early train to London on the 3rd of January (and had the pleasure of travelling first class in view of my tardiness in buying the ticket resulting in the first class ticket being cheaper!). Loaded up with free coffee and biscuits from the first class carriage, I arrived in London just in time for the first session. The venue was great, close to Waterloo Bridge, and there were beautiful views of the city to be seen in the evenings when crossing the bridge to attend the social events. The conference had a packed programme full of interesting talks, clinical practice sessions, e-posters and symposia. One of the highlights included the opening talk by Dr. Charlie Fairhurst who discussed the creation of the NICE guideline for Cerebral Palsy in under 25’s in which he emphasised the importance of treating pain first and foremost because if a child is in pain, there is no point in complex interventions to improve their mobility/social interaction because the pain will hinder the child’s participation. Patients with Cerebral Palsy are particularly at risk of pain from numerous sources (e.g. orthopaedic/muscular problems, GI dysmotility, pressure sores, dystonia etc. in addition to the usual causes of pain that anybody can experience). I felt that the talk also provided a very important reminder of the need for holistic and multi-disciplinary care. There were multiple presentations throughout the conference on current research ongoing in neurological disorders (including neuro-inflammation in psychiatric disorders, antibodies in neuro-inflammatory and demyelinating disorders, neurogenetics etc.) which really made me appreciate the rate at which our understanding of neurological disorders is advancing. There were also sessions on Neuroimaging including advances in fetal neuro-imaging (talk given by Prof. Mary Rutherford) and advances in PET scanning particularly in guiding epilepsy surgery. On the first day, I attended a workshop on Childhood Sleep Disorders run by the tertiary sleep service at Evelina Children’s Hospital, which involved learning about methods of sleep assessment (including polysomnography, actigraphy and sleep diaries). Pharmacological therapy including melatonin and clonidine (for fragmented sleep) were discussed. We also discussed potential contributors to sleep fragmentation (e.g. pain, seizures, obstructive sleep apnoea) and also discussed basic sleep hygiene advice and psychological interventions to help with behavioural insomnia. On day 2, I attended a workshop session on early epileptic encephalopathies and the emergence of underlying diagnoses related to epilepsy gene panels where the indications for genetic testing were discussed. We also discussed when a referral to a clinical genetics service is indicated and the common genetic mutations now being identified on epilepsy panels (SCN1a, SCN8a, SCN2a, KCNQ2, PRRT2 etc). On the third day, I attended a workshop on movement disorder emergencies including how to manage status dystonicus. This was something I had never come across in clinical practice and therefore was a very useful session highlighting the management including pain relief, dystonia medications, checking CK, strict fluid management. The session also discussed common mutations causing dystonia (including DYT 1, PANK2, RRT1, TOR1A) and also discussed surgical management options including deep brain stimulation and pallidectomy. This year’s conference used an app instead of the usual printed programme. The app allowed you to formulate your own personal programme and came with alerts to indicate which talks were about to start. During talks, you could also write notes on the app which were then linked to the talk. At the end of the conference you could then download all of your notes. There was also an option to ‘chat’ with other attendees during the talks (though I didn’t use this feature as I felt I didn’t have anything very intelligent to say as many of the topics were completely new to me!). During the conference, I presented my poster on head injuries sustained following infant falls on the postnatal ward. The poster outlined the findings of a case series of infant falls in UHW between January 2015-September 2017. We found a high incidence of injury on CT imaging in these infants and therefore we propose a lower threshold for CT imaging in this group. We also found significant variation in monitoring, investigation and follow-up of these patients highlights a need for guideline development in this area. I am now planning to expand this project to a multi-centre WREN project collecting data from other units across Wales to gain more insight in to the scale of this problem and how cases are managed elsewhere across Wales.  Dr Anne-Marie Proctor presenting her poster. Dr Anne-Marie Proctor presenting her poster. I was very pleased to see that two other Wales Deanery Trainees also had posters to display at the conference. Anne-Marie Proctor with her poster on Improving EEG investigations: Child’s Play? This poster presented how extension of a child-centred approach to EEG (including play therapy and flexibly timed investigations) to a second site in ABMU improved EEG success rates. Qumrun Nahar also presented her poster on the delivery of Botulinum Toxin Injection for Children with Spasticity: a Service Evaluation Project in Pembrokeshire, West Wales which showcased the service model of Botulinum Injections delivered in a rural DGH. This year’s conference displayed all of the posters as e-posters which meant that poster presenters were given a 3 minute slot to present their poster as part of a powerpoint presentation in a designated room. All presenters had 2 minutes to present and 1 minute for questions. Numerous poster presentations were running in parallel. The positive side of this was having an allocated time session to present your poster, and then you were free to listen to the other posters being presented with no obligation to stay standing next to your poster. The down-side was that because of the parallel sessions it was easy to miss out on seeing another poster that took your interest. For example, unfortunately I couldn’t attend both Anne-Marie and Qumrun’s poster presentations and was very sad to have to miss out on seeing one completely. There were also some posters which I felt could have generated much more than three minutes’ discussion and it was a shame to be limited to that timescale (some of the presenters struggled to describe their poster in any sort of detail in only 2 minutes!). It was an interesting and innovative way to display posters and it will be interesting to see if the idea is taken up at other conferences.
I was absolutely exhausted at the end of the three days, but know that I have learnt a great deal that will improve my interaction with children with neurological disorders, their families and the wider MDT. You can download the BPNA app which has further information on upcoming BPNA courses and events. And if you have an interest in Paediatric Neurology I would thoroughly recommend attending the BPNA conference next year. And if anybody is interested in getting involved in the upcoming WREN project looking at Head Injuries in Neonates on the Postnatal Ward please get in touch at [email protected]!  Association for Simulated Practise in Healthcare (ASPiH), 6th – 8th November 2017, Telford International Centre By Rebecca Broomfield As a part of my Clinical Leadership Fellow year I am focusing on the evaluation of simulation as a teaching technique, attempting to relate this to improved patient safety and improved patient outcomes. Anybody who knows me knows that I love a simulated scenario as a teaching session, it’s not everybody’s cup of tea but it really fantastic opportunity to learn. I therefore jumped at the chance to attend the ASPiH conference. I started by attending a pre-conference workshop session based on Evaluation of Simulation. I was actually unaware that pre-conference workshops happened. A lot of big conferences have a day prior to the main event which they run focus groups or workshops that people can attend to be taught and explore ideas with like minded others. My workshop covered a lot of educational theory behind simulation and how you can use this to evaluate your simulation sessions. Key learning points included the fact that a poor evaluation undermines the development of new approaches. The evaluation itself is “a systematic acquisition and assessment of info to provide useful feedback about some [object]”, therefore while evaluation of the session is often an afterthought and a quick Likert score which nobody reads or bothers to fill in correctly, it really should be an important part of the structure of the simulation session. We also discussed how to structure your evaluation and a way to form a measurable outcome. The actual conference kicked off on the Tuesday morning. There were key note sessions delivered at different points in the day and there were split sessions with a choice of what to attend between these. The keynotes were all interesting a relevant to current trends in simulation. Cherrie Evan’s talk on delivering simulation based education in Africa was an eye opener and inspiring to see how correctly administered simulation can really make a significant difference in patient safety and improve outcomes. Her work was through an organisation called Jhpiego and focuses on the safety of a mother and newborn at delivery. Dr Gabriel Reedy delivered a session on the educational theory behind education, which is particularly relevant to my project. All the keynotes can be found at: http://www.youtube.com/playlist?list=PLzm6Ad9XIwxmnblhwSbEcjceDNpUFW1iu - I’d also recommend watching Dr Al Ross’ talk on Resilience within healthcare if like me you’ve become a bit disillusioned with the term resilience and its meaning. In between the keynotes there was so much going on, it was almost overwhelming. Sessions ran throughout the day with presentations about many different aspects of simulation from setting up in-situ simulations with an emergency department, evaluation of simulation sessions and development of simulations focusing on wellbeing and resilience. The sponsors were around with lots of new technology and we got to play with all the new simulation models. There is a particularly interesting baby and child model which is amazingly lifelike and provokes significant emotion (I automatically checked the veins on this model immediately after picking it up!) I also got to observe a session using a interactive tent to have a projected environment in which to run a simulation. The situation that I observed was a building site with an injured builder. The walls were displaying images of a new housing estate and there were building site noises being played throughout. The tent feeds into the educational theory of distributed cognition suggesting that we need to be investing cognitive power into the technology as well as the people.
ASPiH is working hard to provide a standardised quality simulation teaching nationwide and as such they have developed their standards documents which can be found here: http://aspih.org.uk/standards-framework-for-sbe/. These outline the standard expectations for running a good simulation education program. It is looking into developing an accreditation system in order to promote good quality simulation. We know that simulation teaching is good, we now need to prove it and regulate its delivery in order to standardise experiences. I am even more excited about simulation teaching and its huge potential since attending this conference. I tweeted throughout the days including sketchnotes of some of the sessions I attended, if you are interested in these they are on my twitter feed for the conference dates. I am planning on attending the Paediatric specific International Pediatric Simulation Society (IPSS) conference during May in Amsterdam, if anybody fancies joining me you’d be welcome. If you want more information on ASPiH then visit their website here: http://aspih.org.uk/ As a Paediatrician I think we play a vitally important role in Public Health, we have the ability to make a significant difference with every contact we have with children and young people, therefore I was excited to attend the Public Health Wales Conference in October. It provided an opportunity to keep up to date with all aspects of Public Health as well as focus in on paediatric specific topics, such as adverse childhood events, the venue was fantastic and with Michael Sheen making a keynote presentation what was not to love?! The start to day 1 was nothing short of inspirational, a montage of pictures detailing the history of Public Health in Wales and significant events in history, such as devolving power over health, was accompanied by a harp and a flashmob choir popping up in the audience culminating in a local school choir taking to the stage, it was breath taking. After an impressive start the audience heard from Rebecca Evans, Minister for Social Services and Public health, who updated us on the progress which Wales had made within Public health. The next speaker Dr Christoph Hamelmann, Head of the World Health Organisation Europe office for Investment in Health and Development, spread the net wider and discussed more global issues and reiterated the importance in looking beyond your own borders in Public Health spheres. I was pleased to learn that the ‘Well being of future generations act” really is leading the way within the WHO. We wrapped up before lunch with a keynote on Climate change, followed by a discussion panel exploring air pollution and how we can build a sustainable future. The afternoon sessions on day one were split into ‘Spotlight sessions’ there were many of these going on at the same time and the topics which you could choose from were diverse. I attended one entitled “Mindfulness for wellbeing: Evidence and Practise” The science behind mindfulness was discussed briefly, demonstrating the activation of the pre-frontal cortex when being mindful. Children who are naturally high in mindfulness react less strongly and have better emotional regulation. It was interesting to see demonstrated that by using mindfulness techniques with school aged children you can shift them into individuals with high mindfulness. After the training these children had a significant decrease in the intensity of their reactions to angry faces. Mindfulness has an enormous potential for development within education, as within other areas, but it important that the training is ongoing and children learn to use it within everyday life. Mindfulness, growth mindset and metacognition are surrounding feature of the new curriculum being developed in Wales and has the opportunity to vastly improve the outcomes in mental health for this generation of children. My spotlight session was fantastic, but I had significant spotlight session envy as a college attended a Lego workshop based on driving improvement through the value chain and got to use LEGO to demonstrate visually resilience and improvements – she got to play with LEGO and call it work! (on a side note you can train to deliver LEGO sessions and this could be your job!)
Day 1 ended with a chaired Brexit Debate. The views from the panel were interesting and the uncertainty regarding the exit plans are already causing problems for Public Health initiatives within Wales. The panel presented reasoning that it doesn’t matter what side you were on when voting took place, we need to overcome this and work together to move forward. Wales have already done some of the ground work with how to respond. Brexit is currently overwhelming all of UK politics and other important issues are being neglected because of this focus. But on the other side of the coin, and attempting to be a glass half full type of person, Brexit is a huge opportunity to have ‘No more excuses’ and reduce inequalities. We need to change our mindset on Brexit, accept that it is currently happening and focus on the positives which we can derive from it. Day 2 started by hearing from Dr Frank Atherton who is Chief Medical Officer for Wales and a person I will never get bored of hearing speak. He attended WPS last Autumn and delivered an engaging Keynote there, and as a Welsh Clinical Leadership Fellow we have been in the privileged position to meet him on several occasions. He presented that we should celebrate our Public Health successes (Hepatitis C, Future generations act, reduction in smoking rates) but also recognise that we still have a long way to go. Inequalities still exist and are widening. Moving forward we need to focus on prevention with improved outcomes and ensure sustainability. But because a long term view is not easy to fit into political cycles it is hard to engage managers with this viewpoint. Dr Atherton concluded that we are on the right track and need to continue to engage the public and sustain ongoing developments in Prudent Health Care. Dr Chrissie Pickin followed on from Frank Atherton and presented an engaging talk entitled “Understanding people’s choices and how to influence them”. She started by noting that Health issues are complex and for every complex problem there is a straightforward, easy to implement, wrong solution. Providing education is an obvious solution because the assumption is that people would not deliberately harm themselves but a knowledge gap is rarely the reason behind the behaviour. She gave some top tips to influence people’s choices.
Having learnt about how to influence people’s choices it was fitting that the next speaker, Richard Chataway delivered a talk on Social Marketing and Communication Science. Because we have a better understanding of what drives behaviour change as well as advances in technology social marketing has significantly changed. Richard Chataway presented, amongst other topics, a public health initiate undertaken in Australia, his team wanted to reduce smoking rates. When quitting smoking the motivation is there, the knowledge is there but people need support. He launched My Quit Buddy, an app which provided daily progress tracking, distraction techniques and motivational messages. This was an incredibly successful campaign and the app has had wide uptake. He also explored the use of technology within research into changing behaviours. With the introduction in artificial intelligence it is possible to pre-test communications such as an advertising campaign, to understand it people will find it motivating at a subconscious level this can remove the test and learn element of marketing which will make it more effective, quicker. He again reiterated that in order to find a solution it is important to understand the behaviour and design a solution around it. A panel discussion followed this. After a short break, there were more ‘Spotlight sessions’ with lunch in the middle. There were again many topics to choose from. I attended “Tackling Adverse Childhood Experiences” It is known that if a young person experiences 4 events they are 15x more likely to commit violence, 14x more likely to experience violence and 20x more likely to be in prison than the general population. We need to break the generational cycle and make a social movement for change looking at the root causes and take a psychological approach to tackle these. The impact of breaking the generational cycle is huge, 47% of adults have experience 1 adverse event. The second of my ‘spotlight sessions’, after lunch was “The good, the bad and the social: Two sides of social media” Social media is more addictive than smoking or alcohol, 10 million photos are uploaded to Facebook every hour. It can be both positive and negative the challenge comes with harnessing the positives while mitigating the negatives. Instagram is cited as the most negative with associations to negative body image as well as anxiety and cyber bullying. There was a lot of discussion about where the responsibility lies for managing social media for children and young people. It was felt that this was not just the responsibility of parents, social media itself needs to take some responsibility. The conference closed with Michael Sheen discussing “Building on our cultural strengths: Supporting communities.” As expected Michael Sheen was an engaging and well informed speaker. His message began with the understanding the if you want different outcomes you have to fundamentally change what you do. He outlines inequality as a significant problem, the less you have the more you have to pay for it. If we want families to drive themselves up socially then we need to look at the weight of debt which they have. We have a benefit within Wales as we have a strong community spirit and have held onto our identity and language. As a Public Health team we need to support our communities to be as healthy and sustainable as possible, we need to provide space where communities can come together and shift the power into the grass roots. His concluding statement is worth recognition and highlights a positive to finish a highly engaging conference. “One who has health has hope, and one who has hope, has everything” (Originally a proverb I think!) Once again, I tweeted through the conference and these can be found on my twitter feed from these dates. Public Health is an important topic which is extremely relevant within Paediatrics and the selection of work presented during this conference leaves me in no doubt that Wales really is leading the way. Leaders in Healthcare Conference 30th October – 1st November 2017, ACC Liverpool By Rebecca Broomfield I am currently taking a year out from the Paediatric training program and doing a Clinical Leadership Fellows placement through the Wales deanery. As a part of this year we come under the umbrella of the Faculty of Medical Leadership and Management (FMLM), it was under this disguise we managed to sneak ourselves into the FMLM’s annual conference "Leaders in Healthcare". I went to this conference with an initially pessimistic outlook. I truly believed that a lot of the information provided would be over my head, in a language that I didn’t understand, from managers who were slightly out of touch. I am humble enough to eat my own thoughts and I would thoroughly recommend everybody tries to attend an FMLM conference at some point in their career, indulge me and read on to discover why! As per conference structure, which I am becoming more and more familiar with, Day 1 began with a welcome – another choir, (starting to think this is a new trend .... perhaps someone could do a study?) followed by a Key note speaker. Seriously, this was an impressive start. We heard from Nicky Moffat in a keynote entitled “Leadership is everyone’s business” Nicky Moffat has a background in the military and spoke about the importance of not buying in people for leadership roles but investing in people and growing them up from within. She voiced an important message of inclusion; that every person has a role to play, as a leader your role is to value these differences and figure out how to make them work. You do not have to be able to do everything, but you do have a responsibility to those who you lead to dedicate time to your own personal development. You set the tone, so make sure that you lead your way. She was inspirational to listen to and it was particularly interesting to hear from somebody whose career was outside of medicine but was experienced in a structured, high-pressured environment. After a brief pause for coffee, we split into smaller group sessions. I went for a workshop entitled “Joy in work”. It was run by Henry Stewart, a man who introduced himself as “Chief happiness officer”, which I love, who wouldn’t want that to be their job title??! He runs the Happy company, which has been listed as one of the 20 best workplaces in the UK for five successive years (www.happy.co.uk). Henry Stewart has also written “The Happy Manifesto” a book that has made it onto my Christmas wish list (along with many others from this conference alone.) The company motto is “Don’t tell when you can ask” He has identified that people work better when they are challenged and given freedom. As a manager we should be enabling people to innovate, and rather than focusing on weaknesses we should develop our strengths. Mistakes should be celebrated and, within the boundaries of clear principles and targets, team members should be given freedom and ownership of projects. The style of the session was relaxed, he actively encouraged participation, and provided a significantly different perspective on workplace than my experience of the NHS. Lunch provided an opportunity to network with other conference attendees. There was a wide range of people present, many with backgrounds in significant leadership positions within the NHS. My after lunch session focused on collaboration across barriers and introduced me to the concept of Compassionate Leadership, which will be a blog post for the future. I didn’t want to stick to hearing from people with leadership roles within the NHS, so I headed to a second afternoon session delivered by Carrie Thomas, who herself is an ST4 in emergency medicine, but was delivering a session on how we can learn lessons from elite sport. She directed the audience to focus on the daily standards, looking at the processes rather than focusing on the outcome. She advised learning from excellence, managing what you are able to control and utilising visualisation to drive you forwards. Remember that you are a team and it is vitally important to work together, not only should you commiserate together but you should celebrate the wins. Day 1 ended with an incredibly passionate and moving talk from Gulwali Passarlay (his book “The Lightless Sky” has also made it onto my wish list!). Guwali started with a thank you and a reminder not to forget the little things you do as clinicians daily as they are the important things. He spoke about his incredible journey as a child refugee travelling alone from Afghanistan across 12 countries, to end up in Britain, go to university and carry the Olympic torch in 2012. It served as an acute reminder of our privileges. His story was about overcoming adversity and never giving up. He reminded his audience that having an experience was one thing, but how you used that experience was another; you have a choice. At the start of day 2 Dr Bruce Keogh, hopefully an man who needs no introduction, delivered the opening keynote. He started by stating that we do not want to loose our NHS by mistake and received a standing ovation at the end of his talk. He outlined the history of the NHS and spoke about innovation. I’m not entirely sure that I agreed with some of what he said, but that is probably best left out of this blog for fear of entering a political minefield that I am unable to control or step back from. He did make a very valid point however, stating that people do not fear change, they fear loss. I will be taking this forward as a part of this year, and my future career. An important role as a leader is to engage people, bring them with us, inspire them to innovate and together we will be able to make a difference. As per day 1, day 2 then broke into smaller group sessions. I attended a resilience workshop. This started by recommending everybody watch ‘Inside Out’, which already had me engaged and listening. The workshop ran through 4 stages of coping and looked at each of these. They explained that resilience found ways to bypass stages, and therefore you progress through these stages quicker, or even skip some stages when faced with conflict or a challenging situation. The focus on the ability to define the problem, which would enable you to employ the correct solution. For example, it is important to be direct in complex situations. Building resilience is based on 4 key pillars; confidence, social support, purposefulness and adaptability. They encouraged assessing your own resilience, a tool to do this can be found here; www.robertsoncooper.com/iresilience/ and focusing on one weakness to improve. It was an interesting session, and do now go and watch ‘Inside Out’! After lunch I focused on 'Changing Culture'. Culture is important within a workplace because it impacts the mood and atmosphere which in turn affects performance. Leadership is about gestures and choices which we make all of the time and these influence the culture within our teams. Culture itself cannot be managed, it is a behaviour pattern which becomes established and over time this is reinforced and amplified by visible artefacts. Changing culture is what we are ultimately trying to achieve with our quality improvement projects. Small gestures can create tipping points which is known as the butterfly effect. Within culture change, the leader is in charge but not in control, this is complexity thinking which involves non linear relationships which cannot be predicted. However, machine thinking is the predominant discourse in the NHS; the NHS can be managed and the leader has complete control. The down sides to machine thinking is that everything falls to the leader, participants and team members are passive which leads to significant amount of stress and pressure. A switch from machine thinking to complexity thinking will change the culture. It is hard but as clinical leaders we should be brave! Make that change, a small shift can have a much wider impact. All of us are leaders and we need to recognise this. The final small group session I attended was on coaching – I am exploring this more on a personal level and will during, the course of the year, write a blog solely focused on this theme.
The Leaders in Healthcare conference closed with a keynote from Deborah Rowland: “How to lead mindful change” The most important message I will take from her session is that good leadership starts with knowing yourself. Invest in yourself as a leader, understand your strengths and weaknesses and recognise them without judgement. When you have spotted something you are able to change it, if you don’t look for it and recognise it, then you cannot. Her four key messages for developing your own leadership style were: Perceiving (tuning into the system), Noticing (staying present), Integrating (all aspects, including difficulty) and Choosing (respond, don’t react). To run through all of these points would take a blog post in it’s own right so instead I will direct you to her book, ‘Still Moving’ which is a challenging but useful read. In conclusion, despite my initial reservations, the Leaders in Healthcare conference was an extremely simulating and enjoyable two days. I never felt during sessions that voicing my opinion was not as valid as the opinion of somebody with significantly more leadership experience than myself. The conference has inspired me to continue to develop myself as a leader, and to first reflect on my own skills and weaknesses which will enable me to be better equipped to help guide the NHS through the challenging times ahead. I would encourage everybody to take a look at the FMLM website and available courses and opportunities www.fmlm.ac.uk 9th November 2017, Royal Society of Medicine, London By Chris Course On 9th November, the Neonatal Society held their Autumn Meeting at the Royal Society of Medicine in London. The program included oral presentations of submitted abstracts as well as invited guest speakers. There were a variety of topics covered, from studies looking at postnatal dexamethasone use upregulating surfactant proteins in preterm lamb models, surgical outcomes of preterm infants with congenital diaphragmatic hernia over a twenty-year period, increasing demands on neonatal unit for management of hypoglycaemia and breastmilk exposure influencing preterm brain development. The Widdowson lecture was given by Professor Pierre Gressens of King’s College and concerned the genomics of preterm brain injury. To be honest, some of the technicalities of the science and molecular pathways went a bit over my head, but there seemed to be some promising preliminary results on upregulating pro-repair inflammatory pathways and suppressing the damaging and immunomodulatory pathways by using tiny engineered pieces of DNA to protect the preterm brain’s white matter. Might seem a bit removed from clinical practice now, and seemed to be still a way from trials in human subjects, but then again, in a decade who knows what we’ll be doing on the wards! The keynote lecture came from Professor Rebecca Reynolds of Edinburgh University, who gave a fascinating talk on maternal health determining offspring life-course outcome. She went through data showing that it had been identified in the 1960’s that areas with high infant mortality ratios at the turn of the last century, went on to become areas with high rates of cardiovascular deaths in later life. Over the years, various studies have been conducted looking at the fetal programming effects of raised cortisol (secondary to maternal stress) reprogramming the fetal hypothalamo-pituitary-adrenal axis, and raised BMI/poor maternal diet/lifestyle leading to impaired insulin sensitivity in the fetus. Cohorts have been followed-up which show these infants have higher rates of type 2 diabetes and poorer neurodevelopmental outcomes/behavioural problems. There’s also a cohort of mothers in Finland that’s been followed up based on the amount of liquorice they consume…. Might seem odd, but apparently, it’s a popular snack in Finland, but suppresses an enzyme in the placenta that prevents too much cortisol passing into the fetus. It really highlighted how what we do in early life, and even before conception, can affect us for the rest of our lives! It did however also make me aware that in our role as paediatricians/neonatologists we have an opportunity to change long-term health for the better too. For anyone who hasn’t been to the Royal Society of Medicine, it’s a suitably impressive venue (befitting the name really) just behind Oxford Street, which was perfect for a leisurely lunch and a spot of early Christmas shopping during the society’s business meeting. And the day was rounded off with a drinks reception – what’s not to love! The day really brought home how diverse the neonatal research world is, and how much work is going on to try and improve understanding of physiology, diseases and develop new treatments. The Neonatal Society hold three meetings a year. The Autumn and Spring meetings are one-day, held in London, are free to attend and don’t require prior registration. The Summer meeting changes location around the UK (and sometimes ventures into Europe), with next year’s being held in Dublin in June. Abstracts are invited to be submitted for all the meetings, and are a great opportunity to get projects presented at a high-quality, national meeting – good for the CV/portfolio! Additionally, once you have presented at a society meeting, you are eligible to apply for membership.
For more information, check out www.neonatalsociety.ac.uk St Brides Hotel, Saundersfoot, Friday 10th November 2017 Hosted by Glangwili General Hospital & Bronglais Hospital By Annabel Greenwood This Autumn’s WPS meeting took place in the absolutely stunning location of St Brides Hotel in the picturesque seaside town Saundersfoot. Nestled in the clifftop, overlooking the breath-taking rugged Welsh coastline, it provided the perfect backdrop for an invigorating day of presentations, discussions and networking. The day began with the invitation lecture from the esteemed Dr Trevor Brown, Consultant Paediatric Allergist at Ulster Hospital, on cow’s milk allergy (formerly cow’s milk protein allergy). Ever a diagnostic and management paradox for GPs and general paediatricians, this in-depth discussion covering IgE verus non-IgE mediated reactions, clinical presentation and potential management options was invaluable. The morning session presentations were abundant in variety and interest, including projects and audits from Cardiff University Medical Students, Welsh Paediatric trainees, and Consultants. Of highlight during this session was the fantastic prize-winning project presented by our very own WREN co-chair Dr Siwan Lloyd on head injury following infant falls on the postnatal ward – a case series. The variety in the approach to investigation and management of such patients was fascinating, especially given the high rate of CT head abnormalities of those imaged. The subsequent departmental guideline implemented at UHW will certainly help standardise care and provide more clarity and direction for management. Almost time for lunch, but of course not before the brilliant Guest Lecture from Detective Superintendent Anthony Griffiths, Head of Public Protection, Dyfed Powys Police – ‘Child Protection: The Challenges for Policy and Multi-Agency Working.’ This lecture provided an invaluable insight into the challenges often faced by the police in child protection cases. The videos and images used were extremely powerful and emphasized the great difficulties in tracking down offenders in today’s society, particularly given the huge smart phone and social media influence. After an action-packed morning of presentations and lectures it was time to refuel with a mouth-watering lunch overlooking the absolutely spectacular scenery. Coffee could be taken onto the balcony, and what a treat it was to catch up with friends and colleagues with the sound of the waves crashing onto the shore below. There was also the opportunity during this lunchbreak to visit the exhibitor stands, the main theme being cow’s milk allergy, in-keeping with the invitation lecture earlier in the day, and there were a variety of different formulas to sample at these stands (some of which far more palatable than others!!) The afternoon session was equally interesting and stimulating, including presentations inspiring and empowering trainees, highlighting the importance of blogging, social media and trainee-led initiatives to encourage learning and champion change. The final Guest Lecture of the day was provided by the highly-regarded Dr Julian Forton, Consultant in Paediatric Respiratory Medicine and Cystic Fibrosis, UHW, on ‘the new C21 Curriculum at Cardiff University School of Medicine.’ It was absolutely fascinating to learn how the curriculum and course structure has evolved since my days in medical school! The aim is for a more case-based, small group learning approach with early clinical exposure. The exam format was also an interesting change, whereby all years take the same end-of-year exam, with the focus being on demonstrating improvement and development each year. As the sun was setting at the end of a wonderful day, it was time for the evening entertainment in the form of the ‘celebrating trainee event’ followed by the formal evening dinner. This year the Best Trainee prize went to Dr Siwan Lloyd in South Wales (taking a clean sweep of prizes!) and to Dr Stacey Killick in the North. Best Educational Supervisor went to Dr Zoe Roberts…congratulations to all!
The day was wrapped up with a splendid evening of dinner and dancing (thank goodness for the spa to recover the next morning!) Once again, WPS has delivered an outstanding conference! It provides an excellent platform to showcase your work, and to become inspired by colleagues and friends. It also provides the opportunity to learn from lead professionals in their specialised field, and to celebrate the achievements of others. We certainly are lucky to have such a wonderful paediatric society in Wales! Now, who’s joining me for the Spring meeting?!.... |
Editors
Dr Annabel Greenwood Categories
All
|





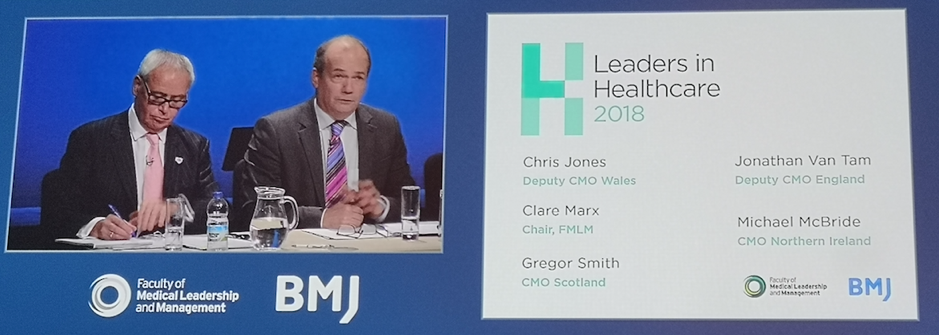
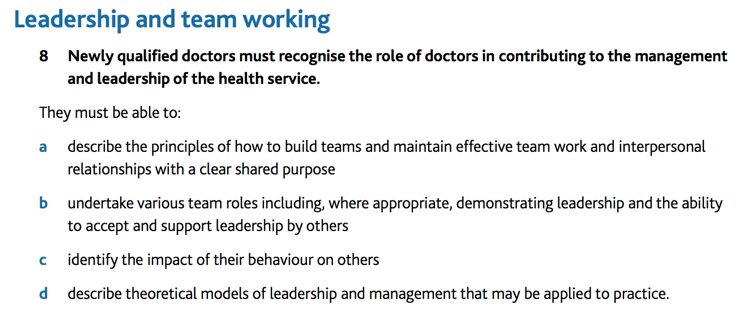
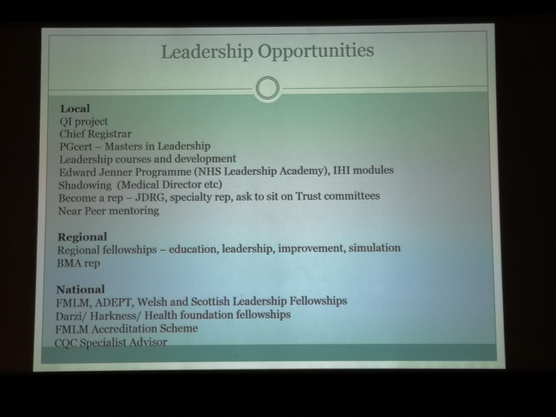
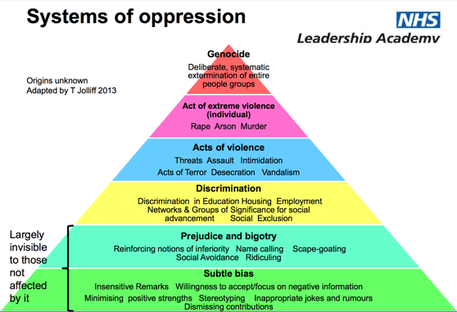
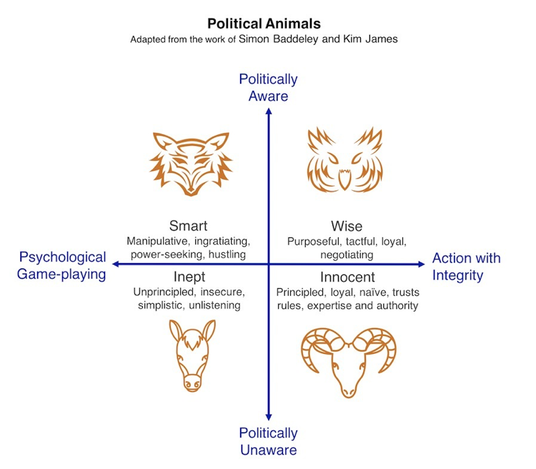
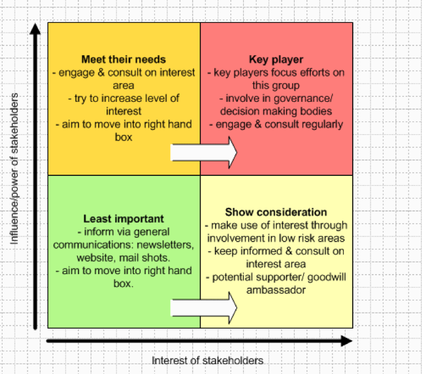
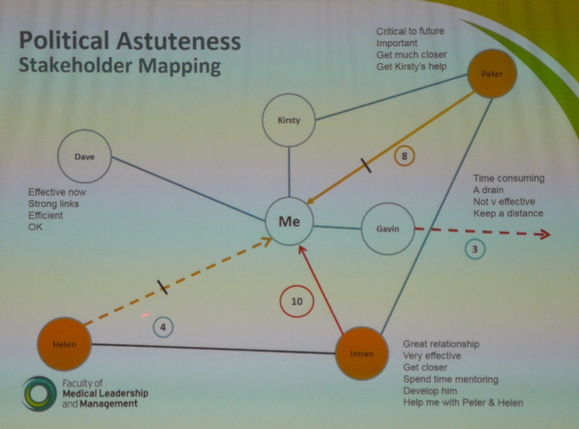





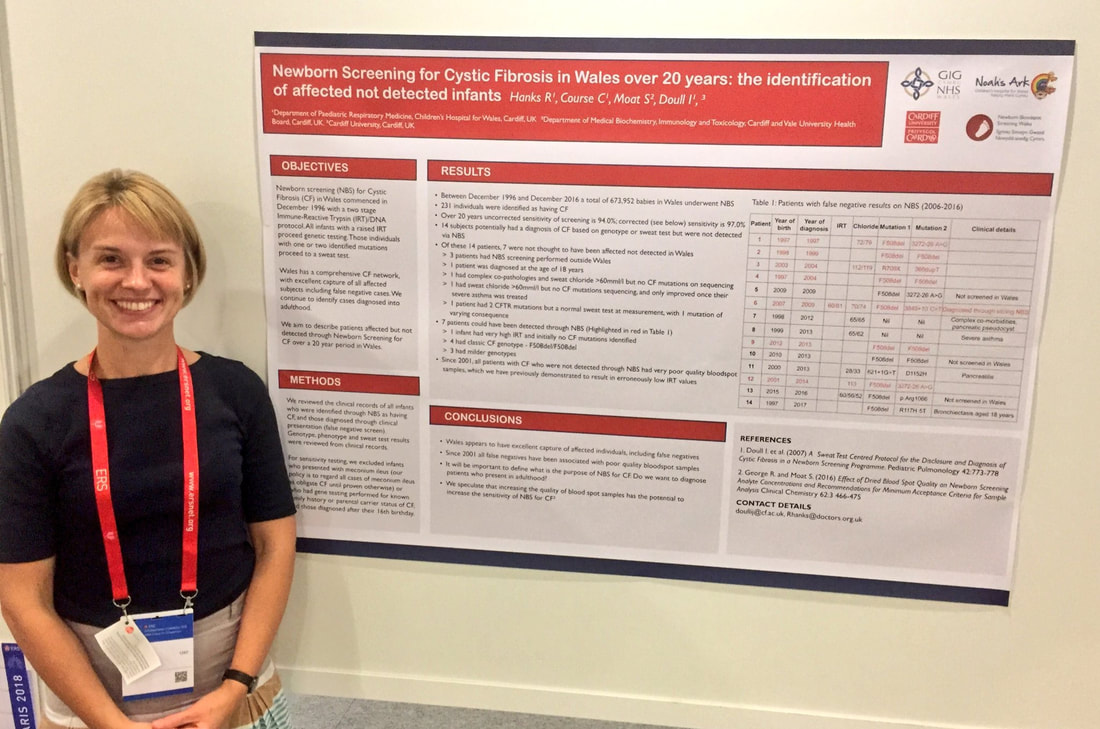

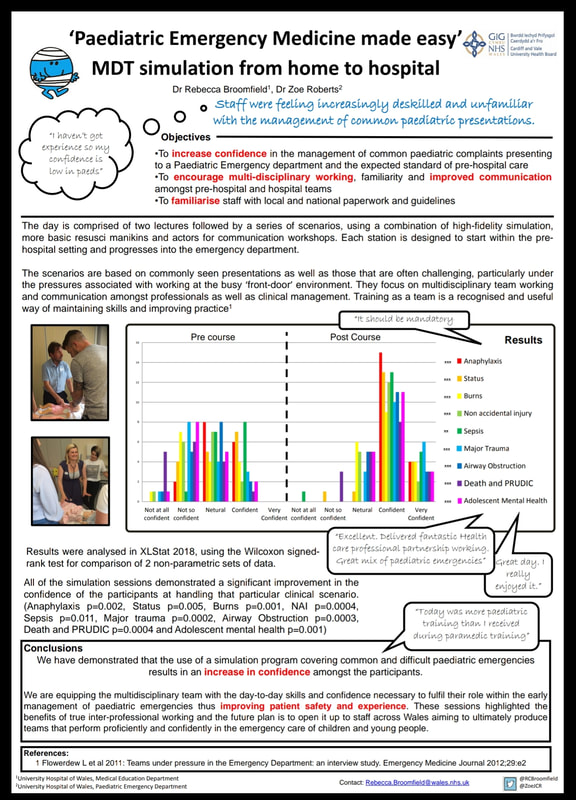





















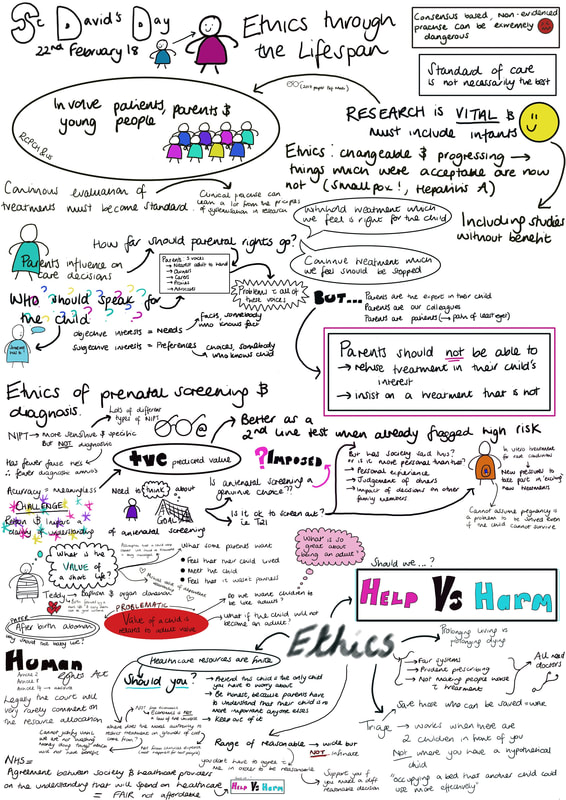
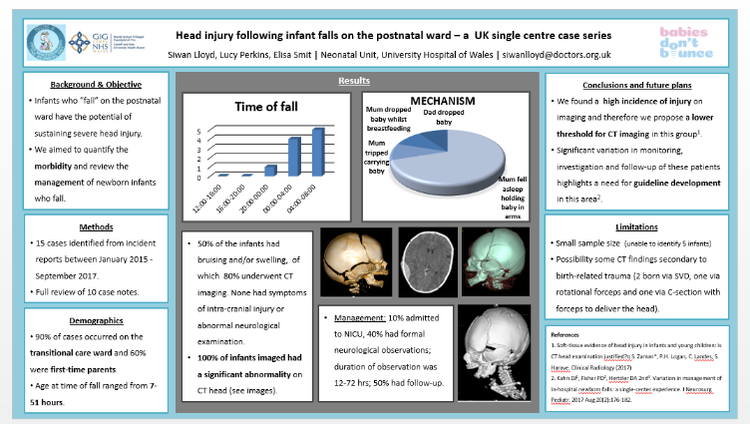

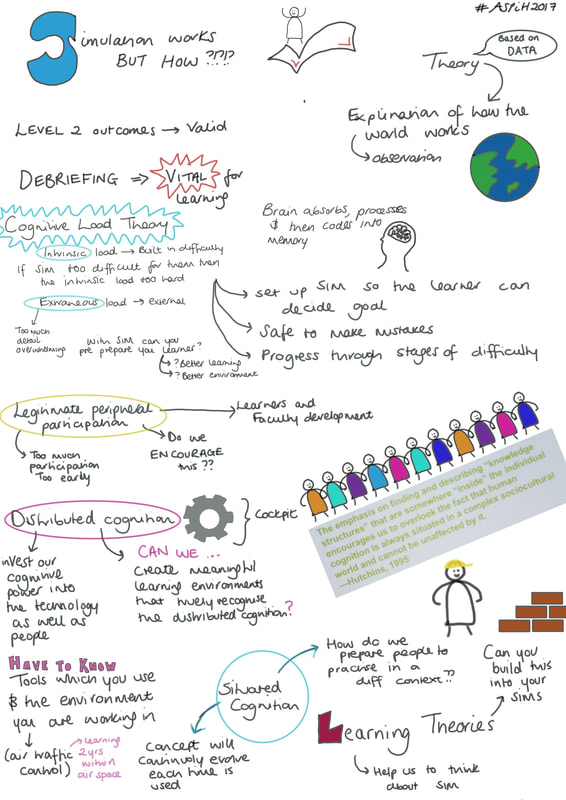
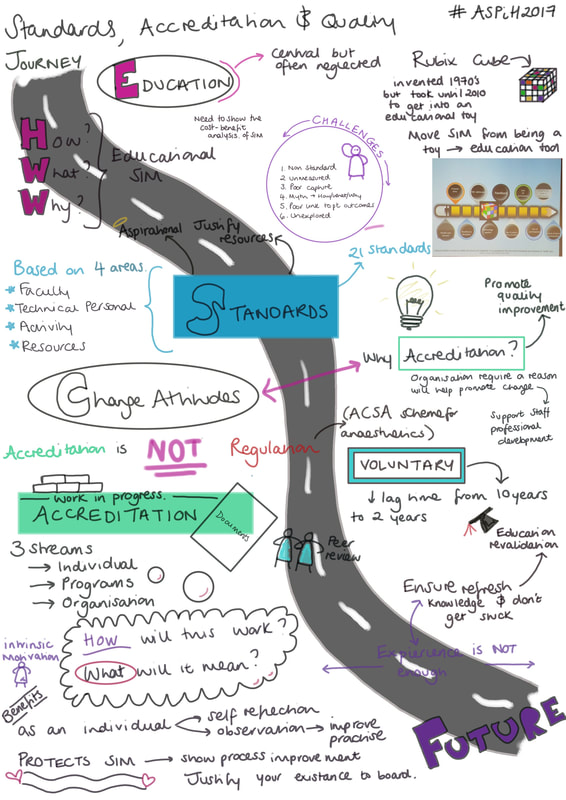



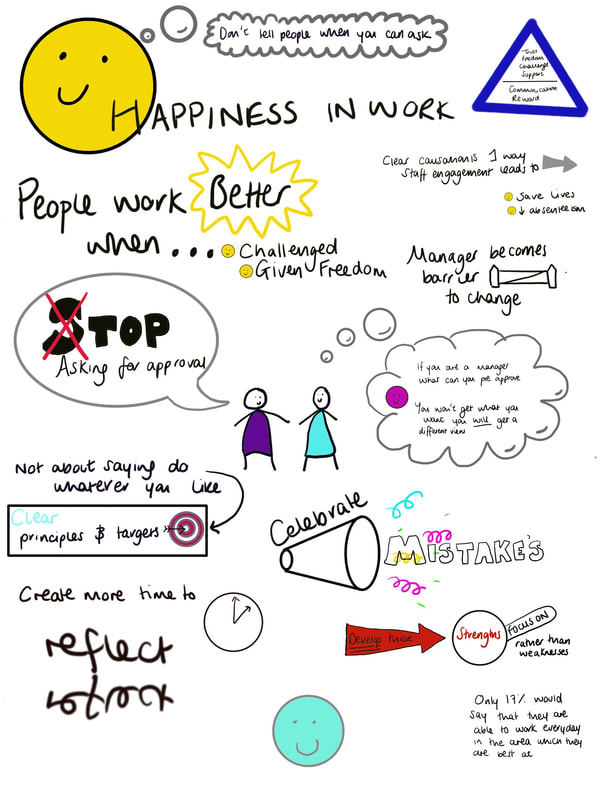
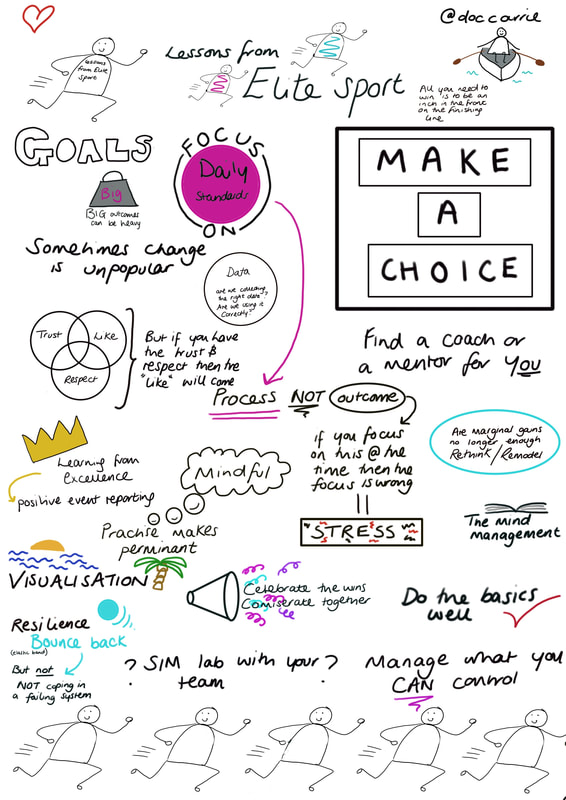
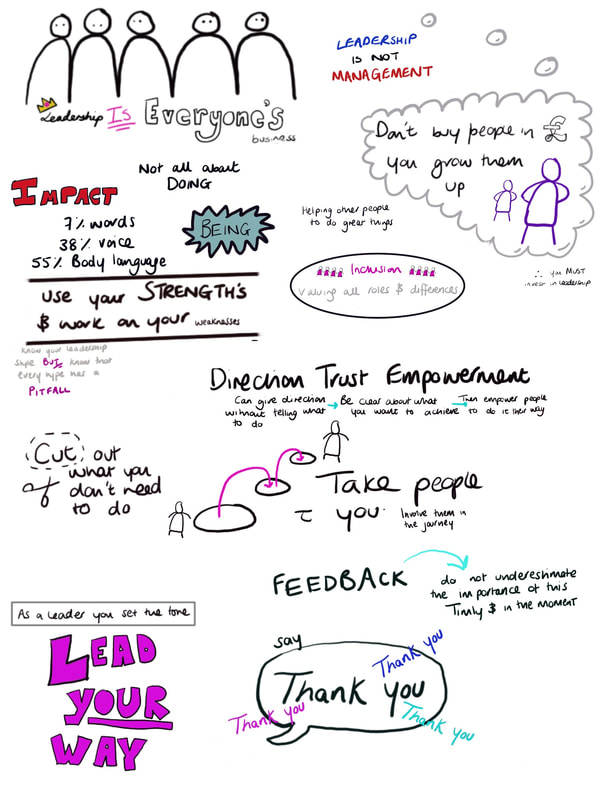

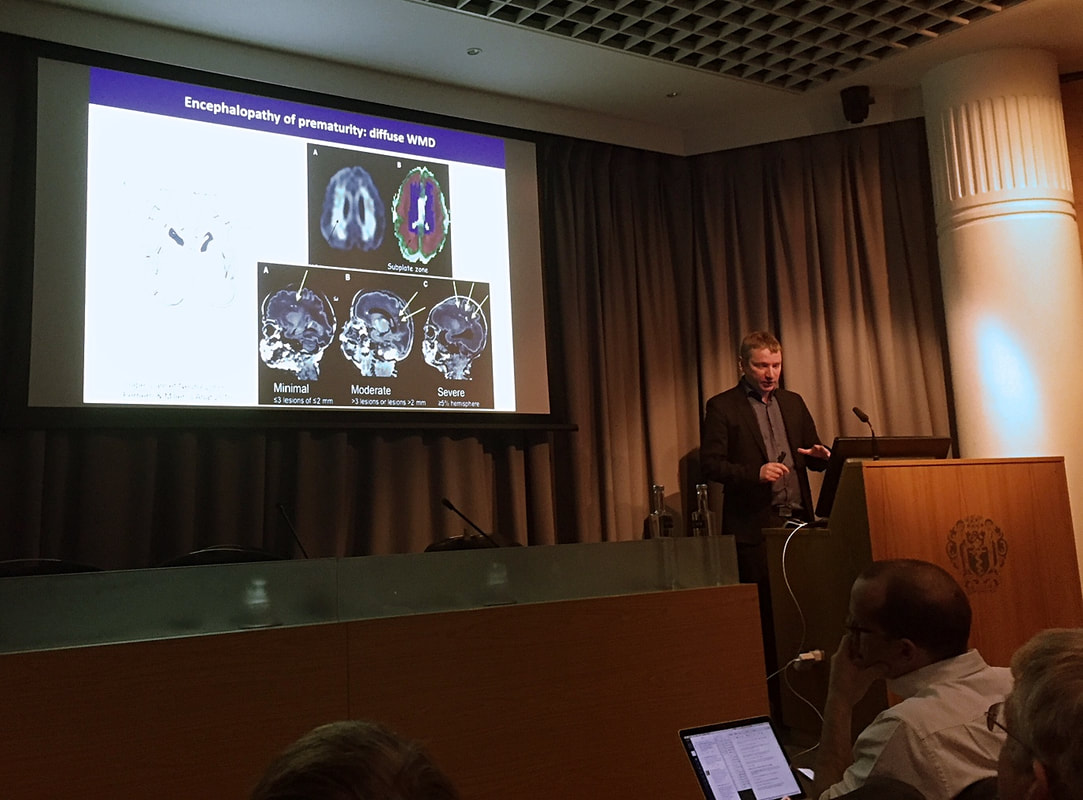
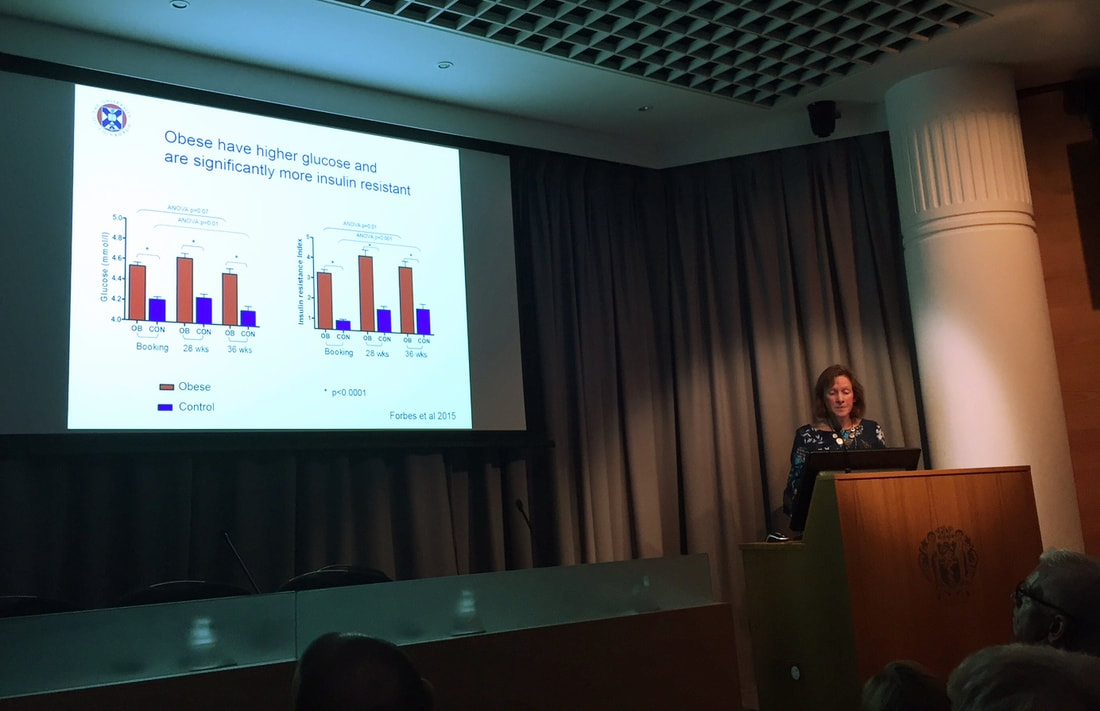





 RSS Feed
RSS Feed
