|
Dr Tom Cromarty Editor Interests: Paediatric Emergency Medicine, Medical Engagement and Leadership, Simulation, Quality Improvement, Research Twitter: @Tomcromarty |
Welsh Research and Education Network
WREN BlogHot topics in research and medical education, in Wales and beyond
Dr Celyn Kenny Editor Interests: Neonates, Neurodevelopment, Sepsis, Media and Broadcasting Twitter: @Celynkenny |
|
An OOPE in Sydney, Australia. Dr Thomas Cromarty I have just returned from an OOPE and wanted to share my experience of living and working in Australia. After embarking on the best training scheme of them all (Paediatrics) in 2012, I worked around South Wales from ST1-5. The Welsh Paediatric Training Programme Director is keen to produce well rounded paediatricians and encouraged me take the opportunity in Westmead Children’s Emergency Department, Sydney. I could tell you about all the trips we went on: Visiting my dad in Canberra, Campervanning around Tasmania, watching the tennis in Melbourne, taking selfies with the quokkas on Rottnest island (Perth), surfing in Margaret River, watching the Commonwealth Games in the Gold Coast, swimming with turtles on the Great Barrier Reef and night treks in the Daintree rainforest. But that will just make you jealous and me sad, so I’ll try and give you unbiased view of my reflections on a year working there instead. “Big surf” in the Australian Life Saving Ironman @ Queenscliff Life Saving Club Nat and I with the Rottnest star of the show aka “The Quokka” It would make a mockery of a blog if I didn’t start by mentioning the Work:Life balance situation! My partner and I lived 500m the beach in a place called Queenscliff near Manly. Our end of the beach was quiet, had waves most of the time and was pretty much perfect. We lived on the top floor of an apartment block which included a roof top terrace aka skin cancer zone. As an “outdoorsy type” I was in heaven. There were running, cycling and triathlon clubs, surfing beaches, SUP, yoga studios, open water swimming and even Dragon Boat racing! You name it, it was expensive, but it was available. Unfortunately, I worked 40km away in the west of the city which meant that I had my old friend, traffic, to contend with on a regular basis. I worked 4 x 10 hour shifts per week in the Paeds ED, with most shifts mirroring the peak attendance times of 14:00-00:00. Despite the commute, there was no chance of me moving to other side of the world and not living by the Ocean! The Work: Positives
Dr Smarty Pants, hard at work… at Westmead Children’s Hospital The Work: Negatives
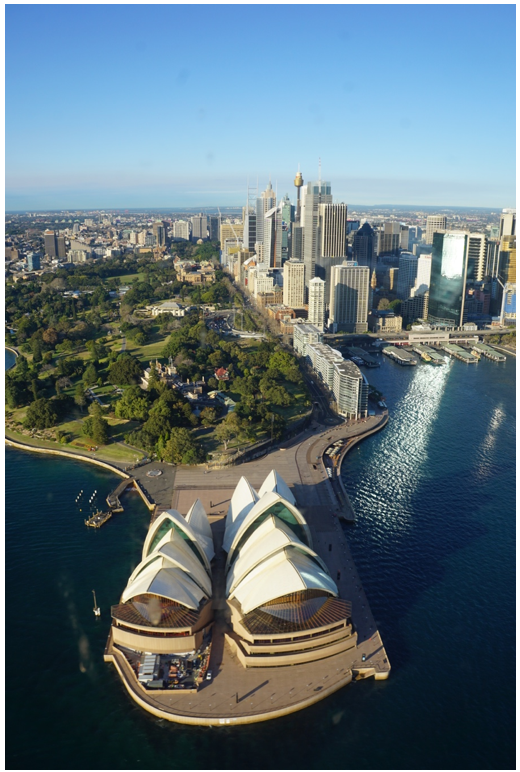
I produced a PDP of goals to achieve throughout the year, these included upgrading my USS skills as well as confidence managing paediatric trauma and minor injuries. I found this particularly useful and would encourage everyone to take some time to establish some short, medium, and long term goals for life both in and outside of work. I think it is essential for all medical staff to experience working in a number of different settings. This enables them to be exposed to a number of working environments and behaviours, choosing which to adopt into their personal style, facilitating their journey to becoming a more effective clinician and leader. My year working abroad will undoubtedly be different to yours and you need to decide if it is right for you (and your significant others!) What I would say though is if you don’t try it, you’ll never know… What’s the worst that could happen?! The start of “Hells Bells” 24 hour adventure race in Noosa, Queensland Helicopter trip over Sydney CBD Fair Dinkum, I had a ripper of a year out and am looking to continue that growth of skills this year as a Clinical Leadership Fellow in Cardiff and Vale, engaging junior doctors in leadership and QI development. If you want to get involved with this project, have any questions about taking a year out or just want to see some more photos please don’t hesitate to contact me at [email protected]. Favourite phrases:
Patient’s parent: She’s been crook for days mate? Doctor: Nah no worries mate, she’ll be right!
1 Comment
|
Editors
Dr Annabel Greenwood Categories
All
|









 RSS Feed
RSS Feed
