|
Dr Tom Cromarty Editor Interests: Paediatric Emergency Medicine, Medical Engagement and Leadership, Simulation, Quality Improvement, Research Twitter: @Tomcromarty |
Welsh Research and Education Network
WREN BlogHot topics in research and medical education, in Wales and beyond
Dr Celyn Kenny Editor Interests: Neonates, Neurodevelopment, Sepsis, Media and Broadcasting Twitter: @Celynkenny |
|
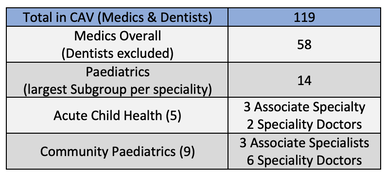
I recently spoke at the Cardiff and Vale SAS (Speciality, Associate specialist and Staff grade) staff forum. The forum was attended by about 15 current SAS doctors and their day included talks from the medical director, amongst other leaders in the organisation. I concentrated on the medical engagement work I had done last year as a Welsh clinical leadership fellow. As a part of that year I conducted a Survey of current medical engagement levels. My aim was to include any non-consultant doctors who would not been previously included in the medical engagement survey conducted in 2012 and 2016. I wrongly considered all non-consultant doctors to be labelled as “junior doctors”. This was more than just an error in nomenclature, as it highlighted my ignorance in understanding the important roles of different medical staff working in the organisation. SAS doctors are neither Consultants nor Trainees, but a separate and highly important group. Paediatrics has a large number of SAS doctors supporting the service in both ward, outpatient and community settings. The numbers in Cardiff and Vale (CAV) Health Board: They are one of the most diverse branches of practice in the health service, make up 20% of the workforce in some areas, and play a pivotal role in the provision of hospital services. I, like many others at all levels of healthcare organisations, had neglected to understand or recognise the incredible work and experience SAS doctors have gained through their distinguished careers. Specialty, Associate Specialist and Staff Grade (SAS) doctors are a key part of the paediatric workforce but are often undervalued and are reducing in number. SAS doctors are senior clinicians with at least four years training in paediatrics, are not a consultant and are not currently in specialty training. This new report from the RCPCH outlines the latest workforce data on SAS doctors in paediatrics and gives recommendations for how employers and workforce planning bodies can better support this essential group (1). SAS doctors are an important part of the paediatric workforce with nearly 800 whole time equivalents working across the UK. Most work in community child health, many in key roles such as Named Doctors for Looked After Children and Medical Adviser for Adoption. Furthermore, there is an average of one SAS doctor on every general paediatric rota in the UK – vital for the maintenance of services and reducing gaps. During my session on medical engagement, we had a number of really interesting conversations on the causes of SAS disengagement as well as potential remedies for improvement. I was interested to hear that many of the doctors in the room had > 20 years’ experience in their respected specialities. Many of these individuals felt under-appreciated and undervalued. Most of my recommendations to improve medical engagement generally, focus on organisations and senior leaders creating cultures where all staff: 1. Feel valued 2. Have a voice 3. Are listened to! One of my favourite questions to ask anyone about medical engagement (if not about most things in life) is; “If money was no object, what is one thing would you do to improve ……. SAS engagement?” When individuals are not constrained by the normal instinctive barriers which inevitably suppress innovation and freedom of thought, individuals and teams come up with some fantastic ideas. The interesting part is that many of these do not require much investment at all. E.g. “I would make sure that the clinics that I run (and have done for 10 years) are in my name instead of a consultant” “I would make sure that SAS doctors are given the accreditation and recognition for the work they have done” “I feel like I have a huge amount of experience in the speciality, can contribute to the decisions being made on a strategic level and just want to have my voice heard” “I would really love healthcare staff to stop thinking I’m not a consultant, therefore, I cannot be experienced!” SAS doctors often fall victim to ‘Gradism’– facing lack of recognition, higher levels of bullying and, in some cases, being denied the development opportunities and incentives given to other branches of practice (3) The same themes came out of the discussions with SAS doctors as those from discussions with Foundation Doctors and Trainees; “We want to feel valued” and for organisations to really show this ‘Actions speak louder than words!’. Forums, where different groups are represented, encouraged to speak, listened to and then those views acted upon, can make massive positive steps towards creating a culture of improved medical engagement. To see the ‘Full Engagement Survey Report’ click here or this link To see the Summary and Recommendations click here or this link For more information on SAS doctors: check out these two excellent articles The Hidden Heroes of the NHS (2) RCPCH: Supporting SAS Doctors (1) The report recommends a number of measures for workforce planners and employers including:
Although the charter was published in 2014, a 2017 survey revealed that 53% of SAS doctors were not aware of it and 65% didn’t know if it had been implemented by their employer. References: (1)https://www.rcpch.ac.uk/news-events/news/supporting-sas-doctors-our-new-report (2)http://secure.rcem.ac.uk/code/document.asp?ID=3793 (3)https://www.bma.org.uk/features/whoaresasdoctors . Covid 19: Addressing the Nation |
Editors
Dr Annabel Greenwood Categories
All
|






 RSS Feed
RSS Feed
