|
Dr Tom Cromarty Editor Interests: Paediatric Emergency Medicine, Medical Engagement and Leadership, Simulation, Quality Improvement, Research Twitter: @Tomcromarty |
Welsh Research and Education Network
WREN BlogHot topics in research and medical education, in Wales and beyond
Dr Celyn Kenny Editor Interests: Neonates, Neurodevelopment, Sepsis, Media and Broadcasting Twitter: @Celynkenny |
Easter Quiz - History of MedicineWe hope you have all enjoyed Easter and are looking forward to warmer and longer days.
Test yourself and spot the correct answer!
ANSWERS: 1-3; 2-3; 3-2; 4-4; 5-1.
0 Comments
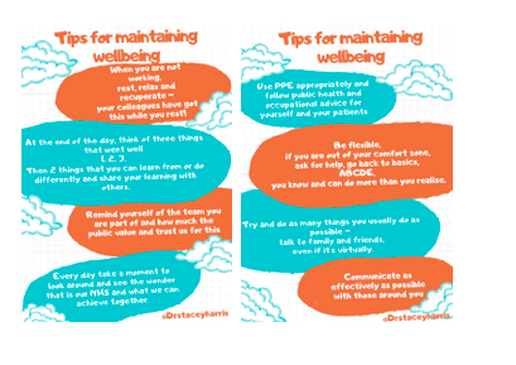
March is here, with Spring just around the corner. As the latest wave of the pandemic is easing, let us pause, reflect and take stock of the last year. So much has happened, so much has changed. In the world and no doubt, in everyone's personal life. Let us also look ahead with hope, and be kind to one another as always! Last week, I enjoyed taking part in a virtual conference - so I thought I'd share the experience. Children's Cancer and Leukaemia Group |
Editors
Dr Annabel Greenwood Categories
All
|





































 RSS Feed
RSS Feed
