|
Dr Tom Cromarty Editor Interests: Paediatric Emergency Medicine, Medical Engagement and Leadership, Simulation, Quality Improvement, Research Twitter: @Tomcromarty |
Welsh Research and Education Network
WREN BlogHot topics in research and medical education, in Wales and beyond
Dr Celyn Kenny Editor Interests: Neonates, Neurodevelopment, Sepsis, Media and Broadcasting Twitter: @Celynkenny |
|
Oliver Walker ST6, Neonatal GRID Trainee Preparing for consultant interviews may feel like a very distant problem in the early years of paediatric training. However, thinking early about what you’d like your future consultant job to be and how to get it can help guide your priorities in the last years of your training. For many of us this may well be the first interview we have had since applying for paediatric training.
Dr Helen Jeffries and Dr Rachel Rayment gave an instructive talk on consultant interview skills at the recent junior doctor leadership session at UHW. They talked from personal experience of being both the interviewer and interviewee. A key message was the importance of preparation well in advance. As well as building your CV in the later years of training, try to demonstrate an interest that will be a selling point to the panel, be it an area of clinical expertise, management experience, research or education. Look online for consultant interview scoring criteria and identify areas of strength as well as weaknesses that you can address in advance. When looking for jobs try to think carefully about whether it is right for you, remember that consultant jobs are often still a career long position. Dr Jeffries and Rayment told us that if you feel the job doesn’t quite fit your needs (e.g. you have a research interest you’d like to pursue) you can discuss any specific changes with your future employer. They suggested that this should be done early in the process as once you are appointed renegotiation can be very difficult. Once an interview has been offered, visit the department, make contact with and ideally meet as many members of the interview panel and department as you can. This will give you a valuable insight into the priorities of the department and likely interview questions. It is as important to meet non clinical as clinical staff. Visiting will stop you being an unknown quantity at interview. Make sure you are aware of local issues and practices - this can be especially true if moving regions or countries. For example, NHS England has a very different structure to NHS Wales with different bodies for service commissioning and service delivery and this alters an organisation’s priorities. Look at the values of the trust or board you are applying to, try to see what the its plans for the future are and how you complement these. When preparing for the interview practice as much as you can with friends and especially consultant colleagues who can offer valuable feedback. There are also services that provide professional advice and training for interview skills. Dr Jeffries and Dr Rayment emphasised that clinical skills are taken as a given - it is how your other skills and experience will fit the needs of the department that really matters.
0 Comments
Dr Christopher Course ST5, Neonatal GRID Trainee The first South Wales & West BPD/CLD Symposium took place at the Holiday Inn Cardiff North on 12th June 2019. The day aimed to update delegates on the latest topics on the prevention and management of chronic lung disease of prematurity (CLD), also known as bronchopulmonary dysplasia (BPD). We attracted nearly sixty delegates from a multi-professional background from across the South Wales and West Country regions. The morning session focused on hot topics in the prevention of CLD. It started with an overview of the current trends in management of respiratory distress syndrome of prematurity, presented by Dr Chris Course. This talk highlighting changes in practice since the introduction of the Wales Neonatal Network RDS Management Guideline in 2016. Progress has been made in mechanical ventilation support and supportive care, but the data highlighted the ongoing need to optimise early care in the delivery room and aiming to stabilise on non-invasive respiratory support. This was followed by Professor Sailesh Kotecha (Cardiff University) presenting his groups ground-breaking work on the influence of pulmonary microbiome on the development of CLD, the negative impact of ureaplasma colonisation, and potential therapeutic interventions. Professor Sailesh Kotecha of Cardiff University Dr Malli Chakraborty (NICU, Cardiff)followed with an overview of the current evidence base for different mechanical ventilation strategies in preventing CLD, stressing the importance of minimising duration of mechanical ventilation, gentle ventilation modes (such as Targeted Tidal Volume mode) and future directions for support, such as NAVA (neutrally-adjusted ventilatory assist). The morning was rounded off with Dr Lieve Boel (NICU, Cardiff) giving an update on the latest research in antenatal and postnatal steroid management, discussing the emerging role of early postnatal hydrocortisone, and potential advances with intracheal instillation of steroids. The focus of the afternoon then shifted towards the management of CLD and the longer-term outcomes of CLD and premature birth. The afternoon started with a discussion on the role of palivizumab in reducing RSV-related morbidity and mortality for those babies with chronic lung disease, and the possible expanded role it may have for late preterms, who still have a higher RSV-related morbidity. Dr Aung Soe, (Medway Hospital Kent) Topic Expert for the NICE guideline on Specialist neonatal respiratory care for babies born preterm (https://www.nice.org.uk/guidance/ng124) highlighting some of the challenges of the NICE review process and summarising the recommendations. Dr Aung Soe presenting the new NICE guideline This was followed with a moving talk from two parents, whose daughter had been born extremely preterm and suffered with CLD. Their experiences were vitally important in bringing all of the science and guidelines discussed so far during the day to impact it really has on families. We rounded the day off with Dr Martin Edwards (Consultant Paediatrician, Children’s Hospital for Wales) presenting his research on the long-term respiratory outcomes of premature birth, stressing that abnormal lung function and increased respiratory morbidity persists through childhood and into adulthood, highlighting that if we can optimise their early respiratory care, we can have a positive impact on their health for the rest of their lifespan.
We would like to thank Abbvie ltd for their help in supporting the day and we hope to organise a similar symposium next year – please stay tuned to the WREN twitter feed and website for more information.  Dr Rebecca Broomfield Here in South Wales we have Sony manufacturing plant based just outside Bridgend. They do a lot of work with the local community and have provided a lot of support for initiatives within the children’s Ward at the Princess of Wales Hospital. Because of this connection a group of paediatric trainees, including myself, were invited to spend the afternoon with their team learning about the different wellbeing initiatives which they have introduced for their employees. We also got to peek around their plant and all came out wanting a Raspberry Pi! Have they got a problem?Sony is a large company which has adapted and remodelled to make the factory and business viable in the current market. They are very flexible in their workforce and their production lines. They are able to upscale and descale production depending on demand and they have diversified in order to maintain the company. The have a variety of space which are able to be utilised for multiple things … but what about their workforce? The site which Sony currently occupies has expanded quickly with increasing number of staff and therefore a greater focus on them. Sony wants to make a quality product as their output and recognise that the staff which they employ are large contributors to the input variables contributing to a quality end product. The staff do shift work and are mainly local within south wales. Sony wanted to ensure that they remained a well thought of employer and therefore surveyed staff about their wellbeing. Prehaps more importantly they have responded to their staff survey with a variety of positive projects. What did they do?Physical HealthSony employees fed back that they did not feel that they had enough information to stay healthy. Sony have responded to this, as a good tech company should, by collecting data on the health of their employees. They have knowledge of the BMI’s of their employees, and promote their staff knowing their blood pressure and health status. They have managed to decrease their percentage of abnormal blood pressure readings over a 5 year period from 46% to 13% (a 33% reduction) simply by having the resources to make people more aware of their own health and its importance. Mental HealthResearch suggests that 1 in 4 people suffer a mental health problem each year. 55% of Sony employees surveyed stated that they would like more support and information on mental health. But beyond that it was also contributing to the companies work absences with 12% of short term absences and 32% of long term absences contributed to by mental health issues. They have then acted on the responses to their survey but providing things for both mental and physical health. Examples of the mental health initiatives include mental health awareness training for their managers teaching them how to recognise and support members of their teams suffering from mental health problems. They have introduced mindfulness workshops and created more informal ‘tea and talk’ events which also feature facilitated discussions on a variety of topics such as emotional intelligence and understanding triggers. They have responded to the employees wish to be more informed on their health by putting in sessions in the canteen focused on healthy eating, ensuring that their menu is well balanced and promoting the benefits of cooking. They have also increased the availability of physical health projects to their staff. They have fitness classes which are free of charge, that take place outside of normal working hours, they have a gym onsite with showers and changing facilities and promote taking part in events such as the Cardiff half. They have also focused on physical activity as a part of their team working days hosting a mini Olympics. They have access to a cycle to work scheme and have step challenges and a running club. As a part of all of this they have also remembered that a lot of their employees have families and have hosted family days out to encourage a positive work life balance for their team members. As well as the wellbeing initiatives they have also listened to the feedback from employees with regards to education and career progression. They have an onsite academy with well structures career pathways and modules to complete for career progression within a person’s interests. They have dedicated time to study and complete these. Importantly, Sony have recognised that some people do not want to progress through a career pathway, they want to turn up to work and be able to do the best job which they can. They have also therefore ensured that even if people do not want to progress through a career pathway they have relevant training and opportunities to keep them up to date within the role they are currently doing. Through the development of the education centre and career pathways Sony recognised that >70% of their employees report to and are managed by their first line supervisors. Therefore they have invested in providing them with appropriate training to coach and support the staff under them, whether it be on a production line or within a more managerial position. There senior executive is also regularly available to all staff, having a drop in breakfast session in the staff canteen. And finally, something which we can all relate to they have Sony version of the Greatix. Sony has some core company principles and all team members are invited to submit nominations for those who have fulfilled a key principle. The person who is selected nominated gets a reward, a picture on the wall detailing their achievement and which core principle they were nominated under but also, uniquely the person nominating also gets mentioned and recognised. It's working in Sony, so how can we bring some of this back with us into the NHS?While working as a trainee within the NHS is obviously different to working within Sony I feel that there are many points of good practise which can be effectively transferred in order to improve wellbeing and maintain a healthy workforce. We need to as a team embrace change, as numbers of trainees gets smaller, rota gaps get bigger and the demand for our service and skills increases we need to be ready to embrace the changes necessary to adapt to this. I have been privileged to work alongside a variety of extremely skilled healthcare professionals from nursing, pharmacy, physiotherapy and other allied health categories. The benefits of utilising this multidisciplinary team more effectively would be beneficial for the best use of our staff and improve work life balance and job satisfaction. As a profession we need to continue to support wellbeing initiatives and in fact expand on these from local teams all individually creating their own micro environment to deanery lead wellbeing initiatives. When I started working as a doctor it was not unusual to have a cake rota providing cake during a weekly teaching session or a breakfast journal club where you met to discuss a paper over coffee and croissants. While I am sat here writing this I am struggling to remember when this was last a regular feature of my job. Small gestures like this have the potential to contribute to a positive working culture and a sense of feeling valued within teams, both of which contribute to improved wellbeing. Like Sony we too can also focus on physical and mental health aspects. I know that the Calm app offer a year’s free membership for healthcare professionals with an NHS email address (go to: https://blog.calm.com/healthto benefit from this) Could this be promoted by our educational supervisors or Head’s of schools so that more people at least know that resources are available. Welsh Paediatrics have recently attempted to promote physical activity and a team mentality by suggesting people sign up to complete a trail half marathon – while this might be madness, it was promoted by our Head of School, was distributed via a HEIW email and demonstrates that our deanery recognises the importance of having different challenges outside of work to focus on, using these to draw us together creating a team environment and contributing to an increased sense of value. If you too want to sign up for something utterly stupid then the link is here: https://toughrunneruk.com/events/cardiff-trail-half-marathon/(note I am a VERY slow runner, I will come last and you would be welcome to join me at the back! I have been promised that no troll will be left behind!) We need to expand our Greatix system including recognising the people who regularly nominate people. While we do not have the budget which Sony has and will not have financial rewards or fancy tech available, the scattered systems which we have currently could be brought together, more centrally co-ordinated and recognised more effectively. Greatix works well in a lot of places but I feel we could expand this initiative significantly within Wales.
Another thing which we should take from Sony was the way which they handle feedback. They have links which employees can feedback anything at any point as well as regular access to the chief executive. They are also, and perhaps more importantly, excellent at feeding back to employees actions which they have taken based on feedback. As trainees we are often asked for feedback but rarely get any response or see any change from the feedback we have given. I know that our feedback is acted on but a more transparent way of communicating this could open channels of communication and once again increase a feeling a value, team work and promote an open culture. And finally, it’s not all about the trainees! As I become more senior within my training I am looking to my consultants for not only for clinical guidance but also looking at whether they are well supported, do they have a good work life balance, do they actually appear to enjoy their jobs??! As a deanery or school should we also be focusing on supporting the people who are supporting our trainees looking after their wellbeing and giving them the resources to be able to inspire the next generation of paediatricians. Camille Roberts ST1 Why did we initiate the project?In paediatrics, as in other specialties, a large number of pre transfusion blood samples are rejected as a result of labelling and sampling errors. Over 200 paediatric pre-transfusion blood samples were rejected in UHW in 2018. We wanted to find out where errors were occurring and whether we could make any improvements. What did we discover?Questionnaires were completed by 43 staff members across paediatrics including senior and junior doctors and nurses. 49% had never received training or none within the last 3 years. 26% were ‘somewhat’ or ‘not at all’ confident with pre-transfusion sampling, and 79% admitted to having a sample rejected previously. We also undertook an audit of rejected Paediatric samples between March to May 2018. 45 pre-transfusion samples were rejected, of which 75% were due to labelling errors. The most common labelling errors were a lack of signature, date of birth, first line of address, and no declaration completed. What did we do?We have put together an informative poster with key points for pre-transfusion sampling, focussing on accurate labelling. This is located in treatment rooms and doctors’ offices across the children’s hospital, including theatres and paediatric A&E. It will also be provided to new doctors at induction. We are working on improving staff competency training rates and have had doctors trained as assessors to facilitate this. We will subsequently re-audit and repeat questionnaires to assess whether rates of sample rejection have improved. How is this relevant to paediatrics & elsewhere?Having to repeat blood samples following errors can be particularly emotive in Paediatrics. However, it is of relevance across all specialties as incorrectly labelled samples are more likely to lead to ‘wrong blood in tube’ errors, necessitate additional procedures for the patient, lead to delays in treatment, and add to staff workload. Any suggestions?If you have any suggestions or if you are interested in expanding the project to your area please get in touch, we would love to hear from you. Dr Camille Roberts (ST1 in Paediatrics) [email protected] Contributors to the project...Ann Patterson, Dr Sally Richards, Dr Ifeoma Ujomu, Samantha Mcwilliam
Dr Huw Davies ST5 #ChildhoodObestiy Welsh Obesity Society, @WelshObesity The Association for the Study of Obesity,@UK_ASO What if we faced an infectious disease outbreak that affected 25% or more of our paediatric population by age 5? 50-80% of those worst affected by it will carry the adverse effects for life. It is a key cause of chronic ill health, linked to Type 2 Diabetes, Sleep Apnoea, Cardiovascular Disease, and Stroke. Insidiously, it creates barriers that prevent those affected from engaging with its cure. It might shorten lives for 20 years or more and is set to create a huge drain on healthcare and social care funding. There would be surely be an outcry against such a plague, and we would marshal all of society’s resources to fight it.... This is the situation for the obesity outbreak, with the greatest implications being for children. In Wales, obesity adds significantly to the burden of disease for society’s poorest. A key thread running through the Child and Adult Obesity meeting, held on the 26thof June, was that childhood sets the trajectory for a lifetime, for the better or the worse. Lucy O’Loughlin (@oloughlin_lucy) from Public Health Wales (@PublicHealthW) presented the scale of the problem. Current surveillance at reception demonstrates clearly that while the proportion who are overweight and obese is stabilising (albeit at the highest levels in the UK), severe obesity is increasing in prevalence. 2/3 of those overweight in reception will be obese adults. Meanwhile parents stress over “skinny-looking” or “under-fed” children because we can no longer accurately picture how a child should look; only <1% of those entering reception class are underweight. Public Health Network Cymru: Obesity Public Health Wales Observatory: Obesity in Wales (2019)Public Health Wales: Overweight & Obesity Welsh Government Consultation Document: Healthy Weight: Healthy Wales BBC: Obesity overtaking smoking as biggest Welsh health risk 'GOOS'The findings of the Genetics Of (Severe) Obesity Study (GOOS) were presented by Dr Agatha van der Klaauw. Genetic screening approaches show potential to understand the mechanisms of weight gain and appetite in the most severe obese, particularly if presenting at an early age or associated with liver or gastrointestinal problems. Some genetic obesity syndromes are also associated with Autistic Spectrum Disorder; children with ASD already face a high risk of obesity because of their challenges with diet and engagement with physical activity. GOOS Useful Resources 'Connect'Aneurin Bevan Health Board are leading the way with “Connect”, a multidisciplinary service aimed at the most obese which provides intensive psychological, dietetic, behavioural and medical support for whole families. We heard from several members of their team, including Drs Hazel Baker and Naomi Swift (@ClinPsychNome) on the impact of cultural, social and psychological factors. Adverse childhood events are being highlighted over and over as serious contributors to poor population health and sadly in Wales we carry a high burden of these. Obesity is not the simple consequence of a lack of willpower, but is a highly stigmatised disease produced predictably by a combination of societal factors, family circumstances, and leads to a psychological hole which is extremely hard to escape. Olivia Colleypriest (@livveycolley22) also gave a dietician’s view on the evidence around very low calorie diets in children and adolescents – an underdeveloped area of study. Sara Jones of Swansea University also provided evidence that the very earliest childhood behaviours are formative and crucial. Breastfed infants are less likely to become obese; while formula fed can often mean over-fed, with pressure to achieve a schedule interfering with the development of appropriate hunger cues from the baby. With the introduction of solids disparities clearly emerge between those receiving high calorie loads from infant food products which set the tone of over-exposure to calories and sugary taste experiences. Infants whose early exposure is instead to whole foods, especially vegetables, seem to benefit throughout childhood and beyond. For the most impact we must seek to promote the healthiest feeding choices for every family. HENRYHENRY(@HENRYHealthy) is an early childhood intervention programme piloted in Leeds, which seeks to build health parenting behaviours while reducing stress and pressure on parents. We heard from the charity’s CEO, Kim Roberts, on the impact the programme has had and their hopes to spread its lessons elsewhere including Wales. Dr Nalda Wainwright (@naldaw) of Trinity St David gave a fascinating presentation on “Physical Literacy” (@Phys_Lit_Wales) – how early motor competence supports engagement with physical activity for a lifetime. Motor delay is common in areas of deprivation and this leads to a downward spiral of lack of confidence and disengagement, with exclusion by peers all the attendant psychological harms. She highlighted the SKIP programme as an early years intervention which can mitigate this serious inequality in outcomes. Over the past decades children have lost many opportunities to play, particularly missing the instruction of older children in basic skills such as throwing, catching, even running. The final presentation, from Dr. Rebekah Pryce (General/Endocrine Paediatrician at ABUHB), reiterated the need for urgent action, from clinicians but also at all levels of society. Setting up Connect required perseverance and they faced several false starts. However, the business case for obesity interventions should be overwhelming – even small reductions could have huge health and economic implications, let alone the multigenerational impact on individual families. Connect aims to provide person-centred care for some of the most at-risk children and families; the psychological, behavioural and dietary interventions required are not trivial. The meeting’s organisers were proud to provide an all-female panel for the Q&A, with a truly multidisciplinary range of voices. The need for leadership at all levels to prioritise population health and preventive approach was highlighted. Education for parents and professionals is a must, with an emphasis on care and support rather than simply another lecture or source of anxiety. Health visitors were identified as the professionals with the greatest scope to work with families to build skills for life; however, this is one of the greatest areas of shortage and under-resourcing at present. With Welsh Government support we can hope that a change is going to come.... Annabel Greenwood ST4 As a Neonatal Registrar, it is not uncommon to be faced with the situation of an equivocal or borderline CSF result when testing for neonatal meningitis. Even when considered together with the clinical picture, it can often be difficult to interpret. Should the baby be started on antibiotics? And if so, for how long? A diagnostic conundrum. It was therefore an exciting prospect to hear that our Neonatal Unit was participating in the ‘PCRctic Study’ for the diagnosis of neonatal meningitis. But what exactly does this study involve I hear you cry?!... What is the PCRctic Study?A multi-centre prospective study designed to enhance the diagnostic accuracy of neonatal meningitis. Why is it important?Neonatal bacterial meningitis is a serious illness that can be fatal if not treated. Early diagnosis is key. However, the diagnosis of neonatal meningitis is often challenging, both clinically and microbiologically, resulting in uncertainty regarding antibiotic initiation and duration of treatment. The negative predictive value of bacterial culture is low and can be inaccurate in confidently excluding bacterial meningitis. What does it involve?"PCRctic" is a novel assay based on 16S rDNA PCR technology. It aims to detect a single intact bacterium whilst eliminating free DNA from dead and/or contaminating bacteria, therefore enhancing diagnostic accuracy, eliminating false positive results, in a rapid, cost-effective fashion. This new diagnostic assay could lead to reduced antibiotic use and hospital stay for many newborn babies tested for meningitis. How does it work in practice?CSF is collected in the standardised way. At least 5 drops are to be collected in each bottle; two of which are standard universal containers, and one an Eppnedorf tube. Parents are consented before inclusion into the study. The samples are then sent to the lab for further analysis…. What does the future hold?PCRctic has already shown promising results for the diagnosis of neonatal bacterial meningitis. The study is currently ongoing across a number of tertiary neonatal units in the UK. Such novel molecular techniques have the potential to replace bacterial culture and enhance our antibiotic stewardship. Want to learn more...'Multi-centre diagnostic accuracy study of PCRctic - a novel 16s rDNA PCR assay for exclusion of neonatal bacterial meningitis' Dr A Abelian, Betsi Cadwaladr University Health Board
Dr Roisin Begley, ST8 PEM I recently attended the RCPCH annual conference in Birmingham and to nobody’s surprise spent the Tuesday PM at the Association of Paediatric Emergency Medicine (APEM) session.
The key talks this year were themed on adolescents. These can be a particularly challenging group for us to cater for at times in the ED. The first speaker was Dr David James, PEM consultant in Southampton. He covered why adolescents are different and why we need to give them special considerations. Key messages were: new thinking/definition of adolescence is from 10-24 years. This has come from the paper in the lancet ‘The age of adolescence’ by Prof Susan M Sawyer et al. The adolescent brain is still developing and lots of the risky behaviours associated with adolescents can be attributed to this. Neuroscientists have shown ‘Evidence points to a dissociation between the relatively slow, linear development of impulse control and response inhibition during adolescence versus the nonlinear development of the reward system, which is often hyper-responsive to rewards in adolescence. This suggests that decision-making in adolescence may be particularly modulated by emotion and social factors, for example, when adolescents are with peers or in other affective (‘hot’) contexts’ (Decision Making in the Adolescent Brain, Sarah-Jayne Blakemore & Trevor W Robbins, 2012) So what is our role in this….. Dr James explains, as paediatrician’s we have a role to use the health encounters to identify risk-taking behaviour and perform psychological assessment: the HEADSS screening tool (Home, Education/employment, peer group Activities, Drugs, Sexuality, and Suicide/depression). The aim is then to signpost on to services locally for support. (ie drugs and alcohol, sexual health clinic, bullying services). Locally in Wessex they have developed an app to help with this. Web based version. iOS and Android on the way. Dr David James runs a RCEM day called the ‘forgotten tribe: adolescent in the emergency department’ if you want further insight. The second speaker was Dr Damien Wood, who explained his role in the eating disorder team in the Nottingham region. He was accompanied by Emily (an ex patient) who told us what it was like to life with an eating disorder and her experience of healthcare. She said ‘mental and physical health shouldn’t be seen as separate- it should just be health’. Emily recommended we all watch: Things Not To Say to someone with an eating disorder. The third speaker was Dr Annette Langseth, Consultant paediatrician at The CYP Haven. Her key messages were that we need to feel comfortable and confident talking to CYP (Children and Young People) about sex. If we feel uncomfortable or ‘judgey’ then they will not feel able to have conversations to us, disclose honest information or ask important questions. So get used to saying ‘vagina, anal and sex toys!' So lastly from me…. I missed this talk and seriously regret it. Dr Mike Farquhar gave a plenary talk on the Wednesday about his experience of growing up LBGT+ in the UK today, but you can get highlight of this issue through his twitter story: ‘ you can exhale now’ and by following him @DrMikeFarquhar and @RainbowNHSBadge. Key themes from this year’s annual conference were investing in the workforce and the future paediatrician with many plenaries and breakout sessions having a focus on staff wellbeing. Considering the ever increasing number of articles regarding dissatisfaction and junior doctor burnout, and the well-known case of Dr Bawa-Garba it was a pleasure to see the college taking on board the struggles of trainee wellbeing and taking the occasion to explore this further. It was an enjoyable experience to have the opportunity to listen to so many inspirational speakers and hear their experiences and to discuss the projects that they had been involved with. For the early risers, Tuesday morning began with a 5K run or a yoga session – I have to admit that I wasn’t there for either due to being on a train but I thought a nice session to include in the programme and begin the day with, and so I hear enjoyable. "Learning from Excellence"Dr Adrian Plunkett, Consultant Paediatric Intensivist in Birmingham, gave the initial plenary session on “Learning from Excellence” for what proved to be a highly motivational talk. He discussed how for so long the focus of health care has been avoiding harm and improving care, by learning from errors already made. He feels it is almost ingrained within us as part of our training to find the mistake, rather than focussing on the positive. He gave the example of a series of sums, and asked the audience what we saw: Honestly, what did you focus on first? The one wrong calculation, or the four that were correct? His take was that we should be taking the time to appreciate and reward excellence and hard work as a way to learn, rather than focussing on what an individual or organisation has done wrong. “Success has a much greater influence on the brain than failure” - Earl Miller (MIT Neuroscientist) Dr Plunkett wants us to ask ourselves, when regarding our peers and colleagues:
His group were the first to spearhead the emerging certificates of appreciation and now has a whole group focussed studying excellence in healthcare to help create new opportunities for learning and improving resilience and staff morale. For those interested www.learningfromexcellence.com and I believe a conference in the planning for February 2020. "The Cost of Caring"Dr Hilary Cass (previous RCPCH president) and Dr Caroline Elton (psychologist and author of “Also Human”) lead a stimulating seminar exploring how the traditional view of patient-centred care wasn’t enough, and more consideration needed to be given to the health professionals providing that care. The “Triple Aim” was an initiative designed to optimise health performance by focusing on (unsurprisingly) three aims - enhancing patient experience, improving population health, and reducing costs. BUT... It is increasingly felt that this is not enough and many organisations are now moving towards the “Quadruple Aim” with the fourth aim being the goal of improving the work life of health care providers. Dr Cass spoke about doctors, and particularly paediatricians being over-represented in those that access professional counselling services. Anecdotally, she describes paediatricians being at higher risk of stress, burnout and depression than some specialities but at lower risk of addiction to alcohol or drugs. Dr Elton discussed her book which many members of the audience had read and appreciated and then discussed her own practice, particularly focusing on career planning for doctors and helping doctors make the right decisions for them when trying to balance the work and lives. www.careerplanningfordoctorsanddentists.com "How does burnout affect patient care?"Dr Judith Johnson (psychologist) discussed causes of burnout and expressed what the majority of healthcare workers are feeling. Many causes of burnout were identified and discussed – excessive workload, low staffing levels, poor leadership, lack of support and lack of resources. These are known, accepted and still people have difficulty challenging that this isn’t right or appropriate. She gave the example of the Mid-Staffordshire inquiry “when staff are burnt-out terrible things can happen”. Burnt out and disengaged staff were present on all levels resulting in a catalogue of events and lack of care. "Wellbeing"Dr Dan Magnus (PED Consultant, Bristol) kicked off the trainees’ session with a lively discussion on wellbeing within medicine. Opening with a comparison between doctors and the crew of Apollo 13. I’ll admit I was slightly alarmed by this statement as I didn’t think things were that bad, only to realise later I’d mixed up Apollo 13 with the Challenger spacecraft disaster, and rather than our careers coming down in flames it was more – “Medicine you got a problem”.
Dr Magnus has done much work, particularly in ED, looking at the need for recovery after shifts and traumatic scenarios. Taking 10 minutes and having a cup of tea after a difficult event is not enough. He described working in Toronto where doctors don’t work more than 2 long day shifts or nights in a row (living the dream)! www.yougotthiswellness.com/ He describes three essential components of wellbeing within the NHS – belonging, competence and autonomy. Perhaps surprisingly he’s not particularly a fan of resilience training “encouraging doctors and medical staff to ‘be more resilient’ is just a crafty way of diverting attention from understaffed rotas and deteriorating working conditions in an effort to get individuals to be more accepting of clinical environments”. He highlights one of the main barriers to improving wellbeing as establishing what people want as every doctor or health professional will have a different take on what’s important to them. Saying that the general view is: better rotas, better facilities for rest and relaxation and more civility and kindness in the workplace”. He identified 5 key statements for improving wellbeing:
www.emtraineesassociation.co.uk/fatigue-shift-work--rotas http://www.emtraineesassociation.co.uk/rest Overall, an enjoyable conference with lots of food for thought!
This talk focused on Dr Rebeccah Slaters work on how noxious information is transmitted to the neonatal brain.
Her research focuses on how the brain behaves at rest and then differs with noxious activity with the aim of improving neonatal pain management. Throughout the discussion the speakers explored how to assess pain in neonates such as scoring systems and assessing facial expressions; although this is much harder in more preterm infants. Speakers then suggested possible analgesics such as sucrose, morphine, fentanyl or light touch. Dr Slater discussed her POPPI trial - which assessed if morphine was a suitable analgesic for ROP screening in infants however this trial was quickly stopped due to safety concerns. The rest of the discussion then focused on ethical issues surrounding pain management for example in patients with HIE, those requiring multiple and frequent blood tests or those having ROP. This series of talks demonstrated the difficulty in assessing neonatal pain but also the rapidly increasing knowledge and evidence. It did raise the question of which analgesic is best and when it is needed with ongoing evidence hopefully able to answer this more. Mike Bailey IT Director, Cardiff and Vale University Health Board  Cardiff and Vale have recently purchased the Patients Know Best patient portal (PKB). PKB is licensed such that any patient of Cardiff and Vale UHB secondary and tertiary services can use it. Primary care is licensed separately, and that cost is under consideration. Mike Bailey: PKB is presented as a website, accessible from any patient devices that feature one of the common internet browsers (PC, laptop, tablet, phone) and is responsive, even where there is a low signal strength. PKB addresses a number of our strategic priorities. We are committed to “Information for You” and as such, PKB will provide patients with access to as much of their clinical data as possible. This will include (past and current) diagnosis, meds, care plans, live results, appointments, letters, images, reports. This should mean that patients will genuinely want to use PKB and positively support patient sign-up rates. There are also a number of operational gain that PKB will facilitate: · Empower the Person. Through various functionality, including online care plans that can be shared with the patient’s care network, support the patients in taking an increased ownership and role in their care. · Facilitate significant elements of service redesign. Including community-based services. Self-reporting, for instance, will enable a significant reduction in outpatient attendance. The capacity freed up in outpatients can be directed to further improvements such as early, supported discharge, with an open ticket back to the ward if becomes necessary. · Facilitate operational savings (time/resource/cost). Very similar activity within Sussex & Surrey IBD process, reduced priority admission waiting time from 6 weeks to 1 week. Reduced admissions (average 5 day stay) by 90% and reduced surgery by 80%. Cheaper medications were also utilised as condition did not reach the same level of severity. · Home First. In addition to early supported discharge, PKB will facilitate the use of online questions and telephone/video conferencing to reduce the need for patients to attend site. · Outcomes that matter to people. Trials within CAV Audiology have demonstrated that when patients are able to complete pre-clinic questionnaires at home, in their own time, the response are much more meaningful and hence enable improved focus on the required care and support. By facilitating a fully informed consent, patients are able to fully understand post treatment impact and actively make a decision on the pathway that suits their needs. This significantly reduced DNAs at the outset of treatment and at the latter stages, when patients fully realise the pending impact on an impending procedure. · Reducing health inequalities. ENT and Audiology have demonstrated that the time saved via unnecessary appointments and improved processes has allowed specialist nurses to target those, often elderly and isolated patients, which have disengaged from their services. PKB also enables patients to delegate access to their records within PKB to their circle of care, thus enabling increased support, through better informed carers - who can see appointments, care plans, letters, meds, help to self-report etc. · Compliance. ENT and Audiology have confirmed that issuing compliance related questionnaires and surveys via PKB has resulted in a significantly higher return rate. · Prehabilitation. PKB can automatically receive and display data from smartwatches and related apps, in order to, with the patients’ permission, track exercise, diet and sleep, as part of prehabilitation programme or just general wellbeing. · Provide cashable savings (letters). Letters to patients will be accessible within PKB, rather than via traditional postage. This is much cheaper than current methods. Even if a patient does not open a letter, it can be rerouted to an outsourced provider, which will send a paper letter cheaper than can be produced internally within CAV. There are many other benefits, specific to each specialty. Initial rollouts will include Gastro, ENT and Audiology. ENT and Audiology already have PKB but, now that we have purchased a full license, we will now be integrating PKB with UHB and NWIS systems to full enable the above benefits. Whilst we await the completion of the integration work, we are also launching PKB for the national Talipes service. This will launch during May 2019, before integration is available but will provide a significant improvement over the current paper-based data collection process Aurey Tong: Whilst we await the completion of the integration work, we are also developing PKB for the Cardiff and Vale Talipes service. This is for parents whose children have congenital talipes equinovarus. The aim is to empower parents via information and support. They will have an electronic version of the talipes passport, a library of resources including top tips, and the opportunity to support each other. Huw Davies, ST3 Paediatric Trainee, Wales I attended the conference entitled "The Importance of a Supportive Environment for Healthcare Professionals". Awareness of burnout, mental health difficulties, and bullying affecting doctors and others in healthcare is at last increasing. We heard several moving accounts from those at all stages of training. A common thread was that all our speakers could objectively be considered high flyers, on the surface coping well with tough jobs. Yet all had felt like failures inwardly: because they were bending under demands of critically understaffed rotas; because they felt responsible for a tragic patient death; because they had been targeted for victimisation, for no evident reason. They had all looked around at peers seeming not to struggle, and thought "what must be wrong with me, that I can't cope". As a profession, our high standards and sense of duty make it hard to take stock and realise that we ourselves need help. Our speakers all mentioned this as the hardest and the most critical step.
The stories we heard stimulated round table discussions discussing what we had heard - how can individuals and institutions value and support our professionals and maintain their resilience throughout a medical career. We had access to well presented research data from the posters on display. I would highly recommend to anyone to raise these issues with their colleagues - those not giving them thought might well be the ones in most need. I hope this conference is replicated again soon and that these voices are heard at local levels too. Katie Richards As part of my Master’s (MA) in Music Therapy and my training to become an HCPC-registered qualified Music Therapist (one of the allied health professions), I am fast approaching the end of my final placement, in a regional tertiary-level Neonatal Intensive Care Unit (NICU), which consists of an intensive care unit (ITU), a high-dependency unit (HDU), a low-dependency unit (LDU) and a nursery. Part of the requirements for our final placement, which forms most of our Advanced Professional Practice module, was that we had to set up a new music therapy service somewhere which had never had it before (one day per week for around 24 weeks). We could choose any client group or setting, and I was drawn to working with neonates ever since reading an article (scroll to see some reading recommendations!)by chance during the first year of this three-year part-time MA course. I was absolutely thrilled when the Senior Nurse emailed me back within minutes to say they’d love to have me on board! I did lots of preliminary reading around music therapy in the NICU and observed a qualified music therapist working in a different regional NICU prior to commencing my placement, so I had a pretty good idea of what to expect. As with all our placements, this involved six weeks’ observations at the start, before commencing our own clinical work. Our placements are very varied, with my first-year placement having been in a Special Educational Needs (SEN) school working with a child with autism and my second-year placement in a private psychiatric hospital working with in-patient adults with acute mental health issues (and some with complex mental health issues, e.g. chronic schizophrenia and dementia co-morbidly). This sets us up for our future work, where the client groups could be incredibly varied (from pre-birth to end of life, and everything in between). The thing about music therapy is that you usually need a wide variety of musical instruments for different circumstances. Because we often work ‘in the moment’, you just don’t know when you may need something in particular, so it’s better to have it with you than not to. Because of this, I start my day by loading myself up like a Buckaroo – one more stringed instrument and my arm might fall off! Neonatal music therapy sessions can look quite different depending on the patient you’re working with and are adjusted to what that particular baby/parent needs at that moment in time, keeping in line with their broader clinical goals. For example, when working with a term baby who was quite aware of their surroundings and in a quiet-alert state, I used musical instruments with more of a sensory impact to encourage visual tracking (e.g. the shiny, reflective tambourine, the colourful rattle or the colourful wave drum – see photo). Of course, these instruments all work on auditory stimulation, but with the added benefit of visual stimulation and tactile stimulation if the baby swipes or grabs one of these instruments. I purposely selected rattles which would be easy for tiny fingers to grip, or instruments which don’t take much physical effort to make a sound, be that with their hand, foot, arm or leg. I was careful to ensure that all of my instruments could be easily wiped clean and sterilised after working with each patient, to reduce the risk of infection. Before beginning each music therapy session, I check with the baby’s nurse (and the parent, when they’re present) if it’s okay for me to work with the baby at that time, or whether they’d rather I came back later that day or the following week. It’s important to check that it’s suitable timing, and to be able to be flexible if not. Checking what state the baby is in (whether they are fairly alert, irritable or sleeping) is also important, and determines whether or not I work with them at that moment and, if so, which instruments I would use for that session. Different instruments would be used for different states and clinical goals, and also for different aged babies.
For babies born at very early gestational ages (e.g. 25 weeks), if they’re not many weeks old yet I tend not to work with them. Their mother’s voice will be the best and safest thing for them to listen to, whether that is through talking, humming or singing quietly. It’s crucial not to over-stimulate very young babies, as they need to adjust to the world first, which takes time. The sensory input from bright lights, noises around the ward, smells and touch can be too over-stimulating if they all occur simultaneously. It can calm them just hearing Mum’s voice (and indeed her heartbeat), whilst feeling the vibrations of her voice and heartbeat during skin-to-skin time. With this aged baby, I would only offer emotional support to the parents, and provide suggestions of how they could use humming/gentle lullaby singing, or even just reading or talking to their baby to support their wellbeing and development at that time, being sure to let parents know to watch out for signs of over-stimulation in their baby, explaining what these might be. For babies born at gestational ages such as 34 weeks, I might work with them while their parent is holding them. In this scenario, I would use gentle (and very simple) guitar playing with just two chords, often accompanying improvised quiet singing (e.g. singing “Jacob, Jacob, how are you today?” [don’t worry – no actual patients’ names have been used in this example!]). I try to encourage parents to sing or hum along quietly, but often find that they are perhaps too embarrassed or self-conscious to do so on the ward, which I can completely understand. It’s not the same as being at home and having your own space, with no-one else watching or listening to your every move while you try to get to know your baby. Research has shown the importance of using the mother’s own voice, as this is what the baby will respond to best. The familiar sounds from being in utero (the whooshing of the amniotic fluid, the strong pulse of the mother’s heartbeat and the muffled sounds of the mother’s own voice, as well as those of people she sees regularly – so often the father’s voice is also recognisable to the baby) create a feeling of security for the baby as it tries to adjust to its new surroundings, so re-creating this in an informed and cautious way whilst watching for any signs of over-stimulation is important. During the music therapy session, I’m constantly looking out for any signs of over-stimulation (there are many!) and checking the baby’s monitor for their heart rate, oxygen saturation levels and respiratory rate, which further helps me to assess their mood and current state. I also check the sound levels of my musical interaction via a decibel-monitoring device. With a more relaxed baby comes development, the ability to sleep and feed better and better emotional wellbeing, which is crucial for the often-traumatic environment they now find themselves in. The gato box (see photo – the two-tone wood block) is used to gently re-create sounds of the mother’s heartbeat, and with this you can help the baby to entrain their own heartbeat to a slower pulse, inducing relaxation and often sleep. Using the wave drum (see photo – the oceanic disc, complete with cartoon octopus!) very slowly and quietly (this can take a bit of mastering in itself!) can re-create sounds of the amniotic fluid whooshing around, also helping to calm the baby, reminding them of a time where they felt safe, secure and contained. The music has the power to ‘hold’ them when they are not being physically held, which is also a really effective way of helping them to feel safer. The predictable characteristics of the music, when used in an informed and careful clinical way by a trained music therapist, are purposefully used to help the baby feel more relaxed. When there is a predictableconstant for a period of time (the non-alerting style of the music used), the baby is less likely to become startled by the unpredictablesounds of bins closing, taps running, monitors beeping, doors closing and telephones ringing etc., as they have that predictable sound (the music) to tune into, which provides a sense of security. It’s also important for my sessions to be quite short – often 10 minutes is plenty. I observe for any signs of over-stimulation and bring the session to a close sooner if this occurs. For term babies who are quite alert and aware of their surroundings, perhaps having been on the unit for a while and becoming increasingly bored by the blank white ceiling tiles above them, I work with them in order to increase neuro-development, where sensory stimulation is key. I would most likely use the reflective tambourine (see photo), the easy-grip rattle (see photo) and the wave drum, as well as my guitar and voice. Simple nursery rhymes with lots of repetition can help with early language development. The rattle, wave drum and tambourine are good for visual tracking, and any of these can be used to encourage them to move their arms and legs more, building up their physical development as they reach out to touch them. Music and sounds used can also encourage a baby who usually only looks to one side to explore the other side too, which can be good for their physical development. When the baby touches one of the instruments, it can also teach them about cause and effect, as they learn that when they touch it, it makes that sound. It can also help babies to learn the (unwritten) ‘rules’ of conversation – they make a sound, then I make a sound, then it’s their turn again, then mine, and so on. This can also provide them with a sense of security – the anticipation of knowing whether they will get their turn again, consistently having those needs successfully met, builds trust and a secure attachment, which is important for their future development, and can last long into adulthood. It can be a bit of a balancing act at times, as I have sometimes worked with term babies who have been on the unit for quite some time who need sensory stimulation and a more lively session, yet they’ve been on the same ward as a baby who is only 28 weeks (gestational age) (e.g. in ITU). In this case, I factor in the rest of the babies on that ward, whilst trying to tailor the sessions to the individual baby I’m working with, so ensuring I’m quiet and perhaps sticking more to guitar and singing simple nursery rhymes, or improvised observational singing based on what the baby is doing, whilst slowly moving the rattle from left to right for the baby to track it visually. I often leave them a small square cut from some thin emergency blanket material (bought especially for this purpose) to play with (supervised!) on the days I’m not there – it makes a fascinating crinkly sound and is very cheap, as toys come! After each session I sanitise the musical instruments, then have to negotiate the notes… who knew it could be such a mammoth task adding a new continuation sheet half-way through a patient’s file?! I attend the MDT meeting when possible, where most of the patients are discussed. This helps me to be more informed about the family situation of the babies (including any psycho-social issues), and also helps me to prioritise who to work with (babies andparents). A big part of my clinical work on the NICU, which people may not initially think of, is talking to (and, more importantly, listeningto) parents and providing much-needed emotional support to them. I also ran a music therapy support group for parents, using relaxation techniques and providing a confidential space for them to meet other parents and explore their experiences on the NICU, using music to help in the process. Parents can be experiencing trauma in the NICU, so it’s vital to provide that emotional support, which can be invaluable for helping them cope. Some parents don’t necessarily have much of a support network around them in the form of friends and family, so it’s important for them to have someone to talk to. We have regular confidential clinical supervision and peer supervision, as well as clinical seminars in university. This helps us to think about the work in different ways, which ensures it remains patient-focussed and helps to achieve clinical goals. Reflective practice also plays a big part in our work as music therapists. If you’d like to get more of an idea of how music therapy sessions look in NICU work, you can watch these two short videos on YouTube (though they’re from America, so it’s not exactly the same): https://youtu.be/bwKCK3W-96E https://youtu.be/4qjx2BrrQJg Reading recommendations: Loewy, J., Stewart, K., Dassler, A., Telsey, A. and Homel, P. (2013) The effects of music therapy on vital signs, feeding, and sleep in premature infants. Pediatrics. 131 (5), pp. 902-918. Loewy, J. (2011) Music therapy for hospitalized infants and their parents. In: Edwards, J., ed. (2011) Music Therapy and Parent-Infant Bonding. Oxford: Oxford University Press, pp. 179-190. Shoemark, H., Hanson-Abromeit, D. and Stewart, L., (2015) Constructing optimal experience for the hospitalized newborn through neuro-based music therapy. Frontiers in Human Neuroscience. 9: 487. Dr Tom Cromarty The term “Burnout” has become somewhat of a dirty word in the healthcare lexicon over the last few years. The insinuation that healthcare staff have somehow failed to build enough resilience or resourcefulness to manage the stressors of life on the front-line. The concept of “front-line” comes from war battlefields and it’s no co-incidence that this metaphor is used in healthcare. Soldiers get diagnosed with PTSD, whilst healthcare professionals suffer burnout. Both of these have at their core the issue of “Moral injury”. If doctors were “in it for the money” then I’m pretty sure they would be astute enough to pursue another line of work. Caring for patients and their families is a vocation for most doctors, or at least it started off that way at some point in the “life choices” decision making process. However, when doctors are not able to deliver the high standards of care they intended for a variety of reasons, this takes a toll on personal wellbeing. The symptoms of burnout are really a “signal” of a healthcare system that is failing to look after its assets. If we want compassionate, engaged and highly skilled doctors leading the charge on the frontline then we need to provide the working environment to facilitate it. This starts with senior leadership recognising that >50% of doctors are experiencing these symptoms and they “Cannot give what they don’t have”! Many organisations now recognise the urgency of the situation and are starting to offer support. However, there are a number of skills which we can develop as individuals to equip us for “combat in the healthcare battlefield”. I have looked up to Dr Mark Stacey for a number of years. An obstetric anaesthetist and human factors expert, he has put together a “Bakers Dozen” of skills. Written as a prescription to yourself, these can all be practiced and developed, in our quest for becoming “Anti-Fragile” (the opposite of fragile funnily enough). I have been lucky enough to hear this talk a couple of times, taking new learning points from it on each occasion. I would highly recommend contacting [email protected]and see the talk in person, but in the meantime here is a short summary of 'The Baker’s Dozen' by the legend himself; 1. Problems: challenge or threat? Do you view your problems as a challenge or a threat? From a practical (and physiological) point of view it is more useful to frame problems as a challenge (problem solving mode) versus a threat (fight/flight mode). This also means reflecting on your self-talk about life eg “life is unfair”, sadly we know that, we see proof of it on a daily basis. 2. Develop optimism skills even if you are a pessimist Having started out researching ‘learned helplessness’ (something many in the NHS will be familiar with, especially our patients), Marty Seligman has become a top optimism guru. His PERMA model (Positive Emotion, Engagement, Relationships, Meaning, Achievement) is helpful. I have also found the ‘Losada principle’ very useful - three nice things to balance/overcome one negative (unless of course if you’re in a long term relationship....). The PERMA Model: Your Scientific Theory of HappinessAlso, have your own mission statement and rehearse it daily. Mine is “today I am going to do the best I can for my family and the people I care for”. 3. Keep a gratitude diary What 3 things have you done well in the last 24 hours? I usually think about these on the way home from work, which sets me up to start the evening in a positive manner. How many of you when you get home complain to your partner? Flip it round – say or do something positive. 4. Do physical exercise (every day) Do not underestimate the benefits of regular physical exercise. Lack of time is an often used excuse, but do you have time not to exercise when you look at the range of benefits (decreasing risk of Alzheimer’s, improving mood, improved sleep and many others)? The 7 minutes exercise app is a great way of moving all your body parts without taking up too much of your time. 5. MEDITATE Probably the most useful skill I have learnt in the last 25 years – it has a whole range of benefits; improved concentration, focus and sleep. If you don’t do some form of meditation you are spending less time on your mental health than you are cleaning your teeth! The simplest meditation technique I have found is the four count breath technique also called box breathing. It only takes a minute – breathe in for a count of 4, hold for 4, out for 4, hold for 4 – do 4 times – perform when you feel that acute pressure coming on and practice every day – teach it to everybody! (Even the Navy Seals are taught it!) 6. Become a stress management expert Imagine a bucket, while at work fill it with the stressors of the day, at the end of your shift find a trigger (for me it is unlocking my bike) to empty the bucket. Now you are going home with an empty bucket ready to be filled with the stressors of home. Set a second ‘empty bucket’ trigger (like brushing your teeth before bed) to set you up for the next day and of course... “Scientists have discovered a revolutionary new treatment that makes you live longer. It enhances your memory, makes you more attractive. It keeps you slim and lowers food cravings. It protects you from cancer and dementia. It wards off colds and flu. It lowers your risk of heart attacks and stroke, not to mention diabetes. You’ll even feel happier, less depressed and less anxious. Are you interested?” (see number 7) 7. Sleep! The above quote is from Matthew Walker’s recent book and if that hasn’t convinced you then I’m not sure that I will. Sleep – ignore it at your peril, it is possibly the most important performance enhancing agent available to you. 8. Ask for Help Never be afraid to do this whether you are a senior consultant or newly appointed trainee. 9. Deal with aggression Learning assertive skills is worth the effort particularly as there will always be conflict in our jobs. 10. Learn Learning is a fantastic skill that does not just teach us the skill – it also teaches us about learning – in particular how, as an expert, it is difficult to understand why the novice is struggling to learn the skill. 11. Make better decisions You could read the enjoyable and academic “Thinking Fast and Slow” by Daniel Kahneman or more readable “Decisive” by Chip and Dan Heath that teaches the WRAP model. In particular note the prepare for failure – we can do everything right in our job but bad things will still happen. 12. Avoid HALT in you and the people you work with Are you Hungry, Angry, Late or Tired? Avoid these factors in yourself and look out for them in your co-workers/friends/partners/ children. They will look out for HALT in you. The HALTcampaign, lead by Michael Farquhar and Guy’s hospital, is a model worth following. 13. Smile As you work through your day see how many people you can make smile. …..And there you have it.
These are all skills! And as such they will all get better after practice and less easy when neglected. Just get started and have a go at two or three of them. I have found the gratitude diary and sleep (earlier bed times) particularly useful in recent weeks and have seen benefits in my overall wellbeing. Mark reminded us that if you never meditate, you are spending more time cleaning your teeth than on your mental health. Some people say “We don’t have time for any of this” but the truth is “We don’t have time to neglect it”. If you want to be the compassionate, healthy, high performing doctor you always dreamt of, the remember “You can’t give what you don’t have!” Baker’s Dozen of Mental Toughness. Your stress management and resilience toolkit The Happy MD – Dr Dike Drummond Mission Statement: Revolutionize the quality of healthcare by improving the health, happiness, humanity and effectiveness of the people providing patient care. Physician Burnout Symptoms ZDoggMD – Moral Injury Reading List from Mark Stacey: Human factors and resilience Mastering Resilience in Oncology: Learn to Thrive in the Face of Burnout. Fay J. Hlubocky, PhD, MA. Miko Rose, MD, and Ronald M. Epstein, MD Practical Human Factor training Martin and Elaine Bromiley – “How mistakes can save lives” Decision making and brain training! Brain rules: John Medina The Decisive moment: Jonah Lehrer Decisive: Chip and Dan Heath Three books: three slightly different takes on human error Safety at the Sharp end: Rhona Flin Field guide to understanding Human error:Sydney Dekker Why hospitals should fly-much lighter than the above: Nance J. Mind management recommendations: The Chimp Paradox: Steve Peters (it works for the Sky cycling team) Search inside yourself: Chade Meng Tan (it works for google!) 10 % happier - Dan Harris- true life story with loads of practical advice-advice-done be put off by the title! 26th March 2019, Cardiff Dr Annabel Greenwood ST4 I am currently in the process of implementing a mentorship programme on the Neonatal Unit at UHW. As a trainee, it’s hard not to feel overwhelmed and at times, emotionally drained by the demands and expectations of our training. Our wellbeing and a positive mindset are paramount in ensuring we can optimise our potential, but how can this be achieved without an appropriate support network in place? Last month, I was fortunate enough to attend the RCPCH Mentoring Skills Workshop in Cardiff to learn more about mentorship and the key principles involved. This was a fantastic one-day workshop lead by Matt Driver and Sandra Grealy, who have a wealth of experience in coaching and leadership. I feel passionately that mentorship is an invaluable process for both the mentor and the mentee, and would like to use this platform to share with you some of the key concepts involved… So what is mentoring? Mentoring is the process of supporting and guiding a mentee in the development of their own ideas and agenda. The mentor is usually a more experienced professional who aims to help nurture the potential of the mentee. The Situational Model The relationship between a mentor and mentee relies on the right balance between ‘push’ and ‘pull.’
This balance helps us understand the differences between coaching, mentoring, directing, and a more hands-off approach. Depending on the situation and the needs of the person, the balance between ‘push’ and ‘pull’ will need to be adjusted accordingly; Coaching: The agenda is set by the coach rather than the subject. ‘Pull’ behaviours outweigh ‘push’ in this case. Directive: The agenda is set by the ‘director.’ It is an important approach where the subject needs to have information. ‘Push’ behaviour outweighs ‘pull.’ Hands-off: The subject is encouraged to do things for themselves, without ‘push’ or ‘pull.’ Core SkillsSo, what are the key core skills to be an effective mentor?
What about advice? Let’s face it, if someone comes to you with a problem, it’s all too easy to jump-in with our own opinion or advice, often backed up by personal experiences. However, this approach is not useful in the case of mentoring, as it discourages the mentee from exploring their own possible options or solutions and driving their own agenda. During the workshop we worked through a useful exercise to help appreciate this difference.
After listening to the mentee, the mentor was given the task of adopting two different approaches; a) Give advice b) Work through a structured set of questions instead;
As you can see, approach b) focusses on ‘success’ and positivity. These are open questions, allowing the mentee to create and explore their own agenda. The ‘T-GROW’ approach to mentoring The ‘T-GROW’ pneumonic provides a very useful structure to shape a mentoring session; Topic
Goal
Reality
Options
Will
The Contract Before embarking on a mentorship session it is important to address ‘the contract.’ This defines the relationship between the mentor and the mentee, and provides the opportunity to explore each other’s expectations at the outset. It is important to emphasise the confidential nature of the meeting, unless of course any alarming information is shared. How do I learn more?
Dr Tim Warlow The Paediatric Palliative Care Team & Ty Hafan hospice are hosting another free conference at the Copthorne in Cardiff on the 9th May 2019.
It will involve interactive sessions on advanced care planning, decision making at the end of life and the All Wales ‘PAC’ Plan. This is one of the most challenging areas reported by new consultants in managing professional relationships and families. We are hosting an expert panel including police, ambulance and organ donation teams, and a live interview with a bereaved parent with an open Q&A session. It promises to be a thoroughly engaging day with professionals from a variety of backgrounds represented, to tackle some of the most challenging aspects of paediatrics. A hot lunch and refreshments are provided. Currently within Paediatric training you have to opportunity after your core training to apply for sub speciality training within Paediatrics. Info on the GRID process can be found here: https://www.rcpch.ac.uk/resources/apply-sub-specialty-training-ntn-grid-guidance The list of sub-specialities available and information about them can be found here: https://www.rcpch.ac.uk/education-careers/careers-paediatrics/sub-specialties Having applied and been successful this year I thought it might be useful to have a blog post covering the best tips which I received along the way. Dr Rebecca Broomfield Before you start? Firstly you need to decide if you even want to apply for a sub-speciality, and if you do then which one! I cannot start this blog by saying that I had always dreamed of being an Emergency Paediatrician - I had not. If I am completely honest for the first two years of my Paediatric training I mainly wanted to pass my exams. However, I was asked an important question the day after finding out that I had passed my clinical exam. (Literally the day after, thanks Dr Ian Morris!) He asked me what I wanted to be. My reply was a rather surprised, hopefully its clear I want to be a paediatrician, but it was the next question that really started me thinking - What do you want to do within that? It made me stop and made me question exactly what type of paediatrician I wanted to be. Now, I don't think he was necessarily asking what GRID I was going to apply for or meaning that I should sub-specialise but I started asking what I loved about my job, what I didn't enjoy and this made me realise that I needed a slightly more focused career aim than gaining my clinical exams and bobbing along through the rest of my training. So, if you are at the start of your career, or even near the end - I ask you "What do you want to do within that?" Is a sub-speciality for you? Do you have an interest in medical education? Have you got a passion for clinical leadership? Have you always fancied a PhD? You might already know the answer. Or you might, like me, have not thought about it until somebody asked. If you have decided on a sub-speciality then you need to start looking at your CV and tailoring it towards that focus. Personally I asked for a rotation in PEM. I attended PEM relevant conferences and took part in PEM research. The QI projects I undertook became more emergency focused and I attempted to gain insight into whether this was the place where I wanted to base my career by talking to the people already doing it. The application The best tip I had here was to look at the marking scheme when you are writing your answers. You can have a fairly good idea of what you are going to score if you at least look at the criteria you are being judged against. I started by brainstorming everything which I had been involved in. I didn't think I had much to go on to be completely honest when I started, but you'd be amazed how much you have actually achieved when you write it all down in one place! Once you have drafted answers and put words together on a page then ask people to read them! Ask as many people as you can from within your sub-speciality choice but also from outside it. Ask people who you consider to be friends but also people who you don't. Put yourself out there, brush away any imposter syndromes and get feedback on what you have actually written. Accept that they will all have different opinions with what you need to include to get top marks and realise that you will not be able to include it all. But the more people you ask to read it the better your answers will be. Importantly don't be to modest - this application my be the only chance to sell yourself to the speciality which you want to be part of. The best feedback I got told me bluntly to sell myself more. It feels uncomfortable to most but it is necessary, nobody else is going to sell you. If you have done something amazing then shout about it! The interview This was possibly the most stressful experience of my career thus far. It is extremely uncomfortable for the majority of people to sit in front of a group of highly qualified experts in the field which you want to join and talk about yourself and how great you are for 20 minutes. If this doesn't come naturally to you then the only thing to do it to practise! Do mock interviews, record your answers to standard questions and play them back to yourself, talk to the mirror whatever you need to do to get comfortable doing it. My first mock interview was a disaster and the second one was even worse but I had a team around me who were willing to help me get better. I read a helpful consultant interview book, had thought of examples for key areas which could be adapted to answer a question, had structures for questions to avoid rambling and, most importantly, borrowed a friends lucky jacket (Thanks Kate!) While nothing can prepare you for the questions which they will ask, and there is always a question you would never have thought of, I felt as prepared as I could be when I hopped onto the long train from Cardiff to London on the day of my interview. Practise and preparation are the key. (Plus a quick toilet based power pose in the RCPCH basement - Thanks Amy Cuddy) Think about what happens if you get an offer I did not do this. Prior to submitting the application you have to rank the jobs which you would be willing to accept. I did this and truly believed that I had thought through all the pros and cons of each place - the 24 hours or so (ok, probably more like 72) of sobbing after my job offer came through suggests that the reality of the situation was slightly different to the expectation that I had had before. So I encourage you to think through the reality of what would happen if you were offered that job and what you would be willing to accept prior to clicking the submit button. On that note, this is my last blog post as an editor for the WREN blog. Thank you for reading and taking this project from strength to strength.
I have been successful in my GRID application I will be starting my Paediatric Emergency training in September, however this will no longer be based in Wales. We felt it was important for the editors of the WREN blog to be based within the Wales Deanery. Annabel will be continuing and I am being replaced by Dr Tom Cromathy who has previously written guest blogs for us. I look forward to continuing to contribute and am sure the blog will be in safe hands! Dr Siwan Lloyd ST4 I was very lucky to be able to attend the BPNA (British Paediatric Neurology Association)’s annual conference again this year. I attended with a poster presentation on “Single-centre case series of outcomes following switch from Levetiracetam to Brivaracetam”. I was also very pleased to see that two other Wales Deanery trainees also had posters at the conference: Emily Payne with her poster on “FLNA Mutation and Epilepsy – A Case Report” and Bethan McMinn with her poster on “Splints – to have and to hold”. The abstracts for these posters are published in the Developmental Medicine and Child Neurology Journal Volume 61, Issue S1. The conference was held at the Titanic Hotel in Liverpool which was beautiful (unfortunately, my study budget did not stretch to me staying there and so I was in a Travelodge in the City Centre which wasn’t quite as glamorous). edit. The Conference Dinner was held in The Cunard Building with drinks beforehand in the British Music Experience where I got to see the Spice Girls’ original outfits and try out some electric guitars (and realise that my very few guitar chords that I learnt in University have long escaped my memory). There was also an evening Ceilidh which took me back to the many good times that I had at Ceilidhs during my 6 years in Edinburgh University. I met many of the Paediatric Neurology GRID trainees who were extremely kind and helpful and allowed me to question them endlessly about what life is like as a Paediatric Neurology GRID trainee. They were extremely supportive in giving me career and applications advice. I would encourage anyone thinking of applying for any GRID specialty to go to the trainee meetings, contact the trainee representatives and attend the trainee sessions at the annual conferences for that specialty in order to meet as many current trainees as possible. The insight and advice that they can provide is invaluable when making difficult career decisions. The conference had a very varied and packed programme and I will just briefly mention some of the most memorable talks. There were speakers from across the world including Brazil, Ghana, Nova Scotia, Marseilles and Ecuador. It was extremely interesting to hear about their clinical experiences working in such different settings (e.g. experience of congenital Zika Syndrome in Brazil). It was also insightful to hear about experience of paediatric neurology services in Ghana and the challenges faced (e.g. limited access to newer AEDs/neuroimaging/lab support) and this again sparked my interest in Global Child Health and reminded me that we should really be striving for equality in paediatric services across the world. These talks also reminded me of the importance of hearing from clinicians working in other countries to gain insight in to conditions that they see more frequently than we do, and to understand the set-up of their services and share good practice. As I’m sure you can imagine, there was a lot of discussion about cannabidiol use and the pressure that there has been from the media, support groups and politicians to prescribe these medications. There was evidence presented on RCTs assessing cannabidiol use in Lennox-Gastaut and Dravet syndrome and also drug interaction studies for co-administration of cannabidiol with other AEDs. These discussions highlighted to me the many emotive issues surrounding this topic which has been of huge media interest recently and the importance of rigorous research and evidence for any medications that we prescribe. The NICE guideline is expected in October 2019. I attended two Personal Practice Sessions: the first on “Vestibular Disorders in Children” and the second on “Neuromuscular Disorders: Floppy Infant Diagnosis and Management” which were very useful. There were many talks on the emerging advances in genetics: next generation sequencing, gene panels, exome sequencing, whole genome sequencing. In the personal practice session on Neuromuscular Disorders, the speaker informed us that genomic investigations are now becoming first line in many neurological presentations. He reflected on the difficulty with informed consent and that his healthboard now employs a genomic nurse practitioner to take informed consent and discuss these issues with families. Their service also runs a “Genomic MDT” to discuss all results and the significance of the variants before the result is fed back to the patient and families (they hold these MDTs once a month with tele-conferencing to DGHs). I thought this was an excellent idea and something that would be very useful to roll-out to other healthboards as these emerging technologies are becoming more commonplace in clinical practice. There were presentations on the re-emergence of SSPE in the UK related to recent Measles outbreaks. It was heart-breaking to hear about these preventable cases. This inspired me to discuss vaccination with any parent/child that I assess during acute admissions and to try to do anything within my power to tackle the misinformation about vaccination which has led to so many tragic outbreaks of preventable diseases with devastating outcomes for some families. One talk that I very much enjoyed was given by R Black and introduced a resource that she and her team had developed called “me and my epilepsy”. This was developed following a qualitative study which highlighted that children and young people with epilepsy had unmet information and support needs. It also highlighted that children’s understanding of epilepsy very much relied on their parents to provide information. An animation was developed alongside the children from the study and all words in the video are the children’s own words. This made me think about the information that we provide for our patients and highlighted the need for more child friendly information and resources to be available and to prevent the situation where parents are the only “gate-keepers of information”. This is important to ensure that all children have fair access to information about their condition. I would encourage you to watch this video and share with your patients with epilepsy: Muir Maxwell Epilepsy Centre – Me and My Epilepy URL: https://www.youtube.com/watch?v=MO7xXL2ZXP8 There was a lot of discussion about the new RCPCH Shape of training report and the impact this will have on future paediatric subspecialty training. Training is planned to be shortened to 7 years, with the introduction of credentialing and increasing opportunities for post-CCT training modules. It was interesting to see the way in which our training is likely to change significantly in its format over the next few years and I would encourage everyone to have a look at this report. It will impact us all whichever subspecialty we decide to pursue.
I would very much recommend the future BPNA conferences to any trainees who are interested in Neurology, Epilepsy, Neurodisability, Genetics or Community Paediatrics. The BPNA also have some excellent courses for interested trainees like the PET epilepsy training courses which I would also highly recommend to any trainee. Siwan Lloyd [email protected]  Dr Rachel Morris ST6 Neonatal GRID Trainee My name is Rachel Morris and I am currently working as an ST6 neonatal registrar in Cardiff. Over the last 3 years I have also volunteered as a Dreamflight Doctor. Over this time, I have been fortunate to accompany 48 children - most of whom are from Wales - to Orlando for their holiday of a lifetime. WREN have kindly given me this opportunity to tell you about Dreamflight and what my role entails. Dreamflight was co-founded in 1986 by two British Airways employees, Patricia Pearce and Derek Pereira. They had a dream of facilitating a trip for children with a serious illness or a disability to Disney World in Florida for a holiday they would never forget. After recruiting volunteer doctors, nurses and physiotherapists from around the UK, they embarked on their first trip in 1987. Now 31 years on Dreamflight has taken over 5000 deserving children from across the UK to Florida. Patricia and Derek have both subsequently been awarded an MBE for setting up such a remarkable, life changing charity. Every October 192 children, aged between 8-14 years, make up 12 regional groups from across the UK, and board their very own private ‘Dreamflight' Jumbo Jet. Many of the children could not travel without the 24hr medical support Dreamflight provides. The children come on the trip without their parents, and may be their first taste of independence, often finding a confidence they didn't know they had. I was asked if I would like to apply to Dreamflight when a vacancy came up in the welsh group. Having heard about the trip I did not hesitate to send in my CV and application. I then had an informal interview to secure my place. Being a Dreamflight doctor is like no other role I have taken on. You become part of the Dreamflight family and form life-long friendships. With each trip costing in the region of £800,000, all year round there are an army of dedicated Dreamflight volunteers that take on huge challenges and organise wacky events to ensure we meet the target. Each time I travel with Dreamflight so many 'what if's' go through my mind. I worry about not knowing enough about each child's medical condition, terrified of what I would tell their parents if they were to become unwell. I think these thoughts will never go away and maybe shouldn't. But very soon into my first trip I realised my role on the trip was much more than being a doctor. In fact, with the support of the nurses and physio within my group, coupled with the incredible support and advice from Dreamflight’s Medical Director you share every major medical decision, which made that aspect of my role slightly easier. Possibly more importantly I also act as an ‘escort’ - a parental figure to two of the children. I can only imagine how difficult it must be for families to hand over their children for 10 days, which is why all of the escorts begin to build relationships with the families from the time their child is selected and send updates when on the trip. It is comforting to be able to relay to the families about all the training and procedures the charity has in place to ensure all of our children are safe, well and happy. Every volunteer would be expected to attend the annual briefing and training day, along with a welcome day for the families and children to meet prior to the trip. While we are in Orlando, each regional group has lovingly chosen a character name - I am part of Team Shrek! (Being the Shrek Doc has a much nicer ring to it that being “The Pooh Doc”!) Each team would have 3 radio holders so that the doctors and team leaders can communicate to share top tips, and request support should they need it. The entire team wear one colour and are easily identified in the busy theme parks, and we have hospital style drug charts to keep track of medications throughout the day. My concerns as the group doctor keep me on my toes even if I’m upside down on a roller coaster! The desire to have that constant knowledge of how the children are feeling, are they getting too tired, have they taken their medications on time, do we have their lunch time medications with us, have they eaten the correct foods, are they well hydrated, are they constipated? As well trying not to be over bearing and give them that chance to be independent! Aghh! A very tricky balancing act and a majorly steep learning curve! It is reassuring to know you are not alone with these concerns, and the wonderful sense of team spirit with the experienced Dreamflighters in the team help to steer us all in the right direction and help create that balance. Each doctor is on-call one night of the trip, the rest of the nights you are 'off duty' from 9pm when you handover to the night nurses and on-call doctor, attending handover again at 7am to resume your doctor/escort role. As well as all the more serious responsibilities, we also ensure we make every day as fun as possible! This involves high quality costume preparation, singing, dancing and lots of partying. We have a different outfit every day, designed around a theme, for example we have 'festival theme', 'American theme', and my personal favourite 'tropical flamingo theme'! We have neon tutus, headscarves, incredible glitter face paints as well as wearing our Shrek ears at all times. I go nowhere without my retro 80s bum-bag, worn like a holster, sun-cream and calpol primed for action. As a Dreamflight volunteer I work within an amazing group, headed up by our group leader Gillie Ticehurst, who is truly remarkable at making sure we all feel supported. During the trip we have a compulsory meeting/debrief every evening once the children have gone to bed. Going around the room, every single group member is asked to share any highs or lows from the day, any physical or emotional strain they may be experiencing. We support and discuss solutions to problems, ensuring work load is being fairly distributed. I have learnt a lot from the attention to wellbeing and peer support the charity offers to its volunteers. With the NHS putting more and more emphasis on wellbeing, it is meetings like this I hope we can incorporate more. With regards to other aspects of my role, it is much more than the 10-day trip. From early February I start spreading the word of Dreamflight. Contacting junior doctors, consultants as well as all members of the MDT to nominate children. Without nominations, the trip simply cannot happen. This can be a major challenge, appreciating how little time health care workers have to dedicate to extra form filling. We then meet the children to carry out a medical assessment and give them a chance to get to know us. We may also need to do home visits to appreciate equipment needed. As a group of medics and non-medics we then work around the clock making sure everything is in place to ensure the trip runs as smoothly as possible. As well as the crazy rollercoasters and outstanding themed entertainment they have opportunities to learn to swim, ride on the back of a dolphin and perform in our talent show in front of hundreds of people. An opportunity so many take up and thrive on. In 2008, eight of the returning Paralympians from Beijing, many of them medal-winning, had been Dreamflight children and say that Dreamflight was a real turning point in their lives. Allow me to share with you a little extract from an email I received following our last trip, a parent of a child with insulin dependent diabetes wrote …'Before Orlando, L was very dependent on us. He was continuously nagged about his blood sugar, as a result he had really low confidence, he was miserable, angry and had very little freedom. Since being home he's like a totally different kid! He's so confident and capable! We've taken a massive step back allowing him to make his own choices. For the first time Saturday he went to a Halloween party for 3 hours alone and yesterday went to a mates house for the entire day ☺…'. I think this feedback really sums up why I feel so passionate about Dreamflight! I cannot emphasize enough how the opportunities the children are given on Dreamflight impact on their future lives. I am passionate about what this small but mighty charity does for the children as I have seen first hand the genuine difference it can make to the children and their families. I assure you it’s far more than a holiday, it’s maybe that chance for a child to find acceptance for their condition, or the capacity to enjoy some independence while in a safe environment, a boost to their confidence perhaps, and for so many of them - a sense of belonging and friendship. For others - it could be just a break from the monotony of their treatment they deserve with the kind of medication that cannot be prescribed - that I guess is the magic of Dreamflight! If you would like to know more about applying to be a Dreamflight doctor please contact me on [email protected] or see our website at www.Dreamflight.org. and PLEASE remember to NOMINATE!
Annabel Greenwood ST4 The All Wales Neonatal Safeguarding meeting, hosted by the Wales Neonatal Network, was an eagerly anticipated event, particularly given it was the first of its kind in Wales to date. As Neonatologists, our exposure to safeguarding is often limited. Let’s face it, we’re far more comfortable managing clinical problems or performing practical procedures, than dealing with safeguarding scenarios. Unfamiliar territory brings with it an air of uncertainty. From a mental wellbeing perspective, it’s not only the babies to consider on the neonatal unit, but also the parents. It has been well documented that adverse childhood experiences (ACEs) can affect both health and well-being later on in life, and it is therefore imperative to provide the appropriate support and guidance early-on for parents in the attempt to reduce the chance of an ACE occurring. The programme in more detail...The All Wales Safeguarding Meeting was held in the Life Sciences Hub in Cardiff Bay, with panoramic views across the waters providing the perfect setting for thought and reflection on such a complex and emotive subject. There was a fantastic representation from all members of the multidisciplinary team, and it was invaluable to hear people’s different experiences and perspectives on various safeguarding cases. The day began with a discussion about ACEs and the concept of resilience in being able to deal with certain ACEs. The Welsh ACE Study conducted in 2015, concluded that for every 100 adults in Wales, 47 have suffered at least one ACE during their childhood. The prevalence of low mental well-being in adults increased with the number of ACEs suffered in childhood. There has also been an association between ACEs and the effects on physical health and health-harming behaviours in adult life. It is important to note that some people are affected more than others by ACEs, and this can be partly explained by a one’s level of resilience. Thereafter provoked a discussion on how we, as the multidisciplinary team, can support parents on the neonatal unit, e.g. providing access to counsellors, neonatal nurses with a specialist interest in mental health, neonatal therapies, and also ideas to enhance the level of support in the community. Certainly, food for thought… It was interesting to hear the experiences from a clinical psychologist’s perspective on perinatal mental health and children’s development. Dr Cerith Waters took us through the child development study, a longitudinal study beginning in the 1980s, and highlighted the key findings regarding the association between exposure to depression during pregnancy and a child’s long-term psychological and cognitive development. The study findings highlighted the importance of early intervention in pregnancy to help reduce the incidence of subsequent depressive disorders in young adults. A number of case presentations then followed, igniting detailed discussion signposting the safeguarding pathways and support available. The afternoon session included an infant mental health perspective on preventing emotional abuse and neglect, presented by Robin Balbernie, a child psychotherapist. This session highlighted the key difference between adult and infant mental health teams, namely that infant mental health teams help ‘get it right’ from the start, as opposed to intervening later-on in life when a person has already ‘gone off-course.’ He emphasised that the first relationships are the most important, and that traumatic events experienced early on in one’s life are preserved life-long. This relates to neuroplasticity and the concept that the earlier the maltreatment, the greater the effect on the brain. Whilst at the same time, the earlier the intervention, the greater its effectiveness. This was then followed by an interesting discussion by Dr Lizzy Nickerson about the difficulties in recognising birth injury versus non-accidental injury (NAI). This talk really hit home the importance of clear documentation at birth and following the newborn examination, particularly in the case of a representation to hospital a few days later with suspicion of NAI. Closing thoughts...From a personal perspective as a junior neonatal registrar, I found this day invaluable in enhancing my knowledge and confidence in safeguarding on the neonatal unit. Safeguarding is a complex and emotionally challenging area of paediatric and neonatal medicine, emphasising the importance of teaching days like these to raise awareness and ultimately improve our clinical practice.
Guest Blog from Dr Emily Shand I thought I knew what Paeds Palliative Care was. I thought it would be sad, but I would find the positives in knowing we were doing all we could in a sad situation. I thought it would be a really emotionally challenging job, and I thought I needed to try it to see if it was something that I could do as a career/special interest. So I volunteered.
Paediatric Palliative Care was a breath of fresh air to me. I had the time to think, reflect and give patients and their family my time. We didn’t have vast numbers of patients to get through on any given day. But those we did have, needed time. As the registrar I was based in the hospital most days, but most of our patients were in the community. We had a big list of active patients, most of whom I never met in person. My working week was sparsely timetabled allowing plenty of time for community visits, MDTs, admin and even reflection, tutorials and learning. I would come in each morning, sit with a cup of tea (oh the joy!) and find out which of our patients were admitted in the hospital. I would catch up with the specialist nurse and either together or alone I would do a ward round. Usually this was touching base with the family, liaising with the team, and symptom reviews or Advanced Care Plan discussions. The families really appreciated someone from the Palliative Care Team being there – even though I didn’t necessarily know the family initially, I was a member of a team who really knew their patients well and therefore a link to this support network. I would do a weekly round in Ty Hafan, the Children’s Hospice, with the consultant. Most of the children were there for respite, so were very well and enjoying life. Seeing the children in Ty Hafan really highlighted to me that we can get a completely different view of a child by only seeing them acutely unwell in the hospital. One stark example was a child I saw when doing an acute General Paeds shift overnight who was thought to be end of life on the ward. He was transferred out to the Children’s Hospice where I saw him again a week later – snuggling in bed with his pet dog - although minimally mobile and outwardly inexpressive, clearly getting joy from his companion. Children and their families are often so much more relaxed in the hospice environment - clearly happy and comfortable. It's hard to remember this when you only see them on the inpatient ward or unwell in the assessment unit. My experience in Palliative Care has definitely opened my eyes wide. I learnt about the common symptoms, how to assess the cause, and how to tailor the management holistically for that individual. I revised some pharmacology and gained confidence in prescribing symptom control medications, but realised drugs weren’t the only solution, and thinking outside the box was needed. Pain is so much more than just physical. Difficult conversations became more normal. I realised that often it is more difficult in anticipation, but when talking to the family it felt almost natural to discuss death and dying – they had been thinking it anyway. We had the luxury of longstanding relationships with these families, and the most wonderful nurse specialists who knew how much to say, when, and just how to say it. I learnt so much from being with them. Paediatric Palliative Care is not solely end of life care. It is being there, supporting children, families and their medical/nursing teams through the ups and downs of their condition. It is holistic care. If you ever get the opportunity to have a taster in Paediatric Palliative Care, whether it is a day or one of your rotations, the fantastic team of doctors, specialist nurses and the huge number of support staff will welcome you and I can guarantee you will learn more than you ever imagined you would. Dr Tom Cromarty Welsh Clinical Leadership Fellow, Paediatric ST5 Trainee Having been a Leadership Fellow for at least three months now, I am beginning to appreciate some of the key traits which great leaders develop and demonstrate. The opportunity to attend leadership conferences enables me to be immersed with people enthusiastic about medical leadership. People who are passionate about improving the lives of medical staff and the patients they serve. The “Leaders in Healthcare” conference was run by the Faculty of Medical Leadership and Management or “FMLM”. The FMLM aims to professionalise medical leadershipand improve patient care. Trainee membership is £84 per annum and you receive a whole lot of bang for your buck if you use all that is on offer. The conferenceconsisted of 3 days of masterclasses, keynotes and plenary sessions with a diverse set of speakers. 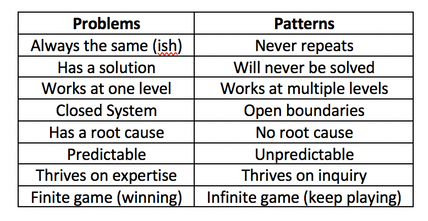 To be honest the most reassuring reflection from the conference was that there are no ground breaking new short cuts, evidence or cheats to employing great leadership. https://hbr.org/2018/11/the-fundamentals-of-leadership-still-havent-changed. Often with the best presentations, your practice is challenged, and usually more questions are generated than answered. Below I have put together a few small summaries of my favourite sessions over the week. I hope you enjoy them, there are also some exercises at the end to try. Political Astuteness: aka “Influence in Organisations” The world in which we work can seem vast, that’s if we are even given the chance to look up and have a glance for ourselves. Early on in a career, often the overwhelming thought is “I don’t do politics”. The usual pattern then follows with “Wowza, I need to know about politics” (to change things for the better) and finally “I need to tell everyone about how to master politics at work” (so we can all change things). This realisation is a like a loss of innocence. It’s easy to think you are just a sheep, but the world is complicated, and you NEED to develop political astuteness to be effective in the world. Directing individuals through authority or using a badge/label to exert power is not leadership, it is management and poor management at that. Leadership on the other hand is the ability to influence individuals. Influence cannot be bought or attained through hierarchy. The internal values one holds, shape their external behaviours. Your behaviours are the markers on which you are judged by others. For this reason, influencing power can be developed by and exerted at anylevel. “Does she/he do what they say?” As an individual you decide…“Am I going to be influenced by him/her?” Patterns not Problems: Working with Intractable Issues Types of problems:
Stephen Powis, National Medical Director of NHS England “In uncertain times, the only known is that there will be change, and it looks like it will be YOU doing the leading!” Digital revolution: Not just AI, but intra-operability, health/medical data, wearables. Link to the global health agenda.Genetic revolution: Need masses of space. Currently leadership is seen as aposition for individualsrather than a behaviour for everyone. We must stop the unhelpful “I’m just a….” attitude and the notion of“Don’t get ahead of yourself there Dr. X, you don’t need to be doing that yet”. Leaders need to aim to regularly add value to the people around them, and everyone can do that, every day. “It will never be someone like me” But think “Control your own destiny” it needs to be done by someone, why not make it you? Read theBMJ Leaderfor leadership tips, research and evidence. Matthew Hancock – Health Secretary England The NHS needs a leadership culture change. We must stop apportioningblame but start really harnessing a culture of learning from mistakes. Anyone who says they have never made a mistake simply isn’t telling the truth. And the truth is at the heart of honest reflection, learning and moving forward. We want staff to challenge without fear and encourage complaints as these are opportunities to improve. Ideally, we want to give away the directive and hierarchical power and consequently empower all individual healthcare workers. This is what we are! This is where were going! This is how were going to get there! Ends with a challenge: What are you going to do? Tim Swanwick - Leadership in the Undergraduate Years “Leadership is a contact sport which brings about change. This cannot be done from the comfort of a desk or department headquarters. The key to developing leadership skills is to get outside of your comfort zone, that’s when you learn the most. Seek out opportunities and go for it. Lead the way to your own future.” “Management makes sure the ship is stable, Leadership sails it in the right direction.” It seems like it wasn’t too long ago where communication skills were thought of as innate. If you had them, you’d be a GP, if you didn’t then you’d be a surgeon or a pathologist (I jest of course but you get the point). Thankfully, at least for the past 15 years, medical schools have recognised that everyone needs to be taught these key skills and consequentially there have been significant improvements. Communication workshops with breaking bad news and explaining diagnosis and management plans have upskilled all doctors and made a massive impact on the care delivered to patients and their families. The tide is changing, leadership & management is being asked about in medical school interviews. Specific leadership skills curriculums are being introduced into universities across the country next year. “What if every newly qualified healthcare professional graduated thinking as a leader.” GMC document 2018 – “Outcomes for graduates”. 1stdomain in the curricula. https://www.ted.com/talks/angela_lee_duckworth_grit_the_power_of_passion_and_perseverance?language=en The science of Leadership & Management is not new. There are 15,000 members of the American Academy of Business who have been researching L&M for many years. The BMJ Leader could bring business school world evidence to medicine. His best advice: Go and get some honest feedback, it will be perhaps the most useful gift you will receive from a colleague?!? Try asking this… “Tell me one thing that I do which is negative?” It takes a degree of bravery for you to ask and reciprocal bravery for them to answer honestly as well. He also insists that we should all have mentors. One can have multiple mentors, e.g. a leadership and speciality mentor. They offer a sounding board for example, difficult interactions with a colleague. They can guide you and order your thinking. Consider the following as some of the more “formal” leadership opportunities: Other Resources: NHS Improvement: Developing People Improving Care Great project in Scotland: Project Lift: NHS Scotland https://www.projectlift.scot/ Diversity And Inclusion in Healthcare Do you know what the 9 protected characteristics of the Equality Act 2010 are? Do you know what “BAME” stands for? This was a really interesting session recognising that even if there is diversity in the workforce or patients, these groups may still lack full inclusion or equality. Leaders need to learn how to o address these issues and respond to unconscious bias. How to hear some difficult messages, and how to respond positively. All too often issues are not confronted as “Oh this is making me feel uncomfortable” or “Of course we’re not, that can’t happen here”. We all need to be “Power aware, Identity aware and Self-aware”. The mindset we embrace in the workplace that liberates other people. Often organisations only take a stand when it gets to “Discrimination” stage, as the lower levels are largely invisible to those not affected by it. We need to upskill leaders so that everyone is aware of what is happening, the behaviour is addressed sooner, everyone has the courage and permission to call out bad behaviour. Courage is the most important of all the virtues, without courage you can’t do any of the other virtues consistently. “The behaviour we walk past is the behaviour we accept” Barriers to successful inclusion:
“The only person I can change is myself, how I show up might encourage others to shift their focus, their attention and their behaviour” If you are reading this, you are part of the generation that can make the change! Malala Youssef – Nobel Peace Prize award speech– “Let this end with us” Richard Watson – Futurist: Mega Trends and Technologies2017-2050 It seems that Richard and many others who look to the future can only be sure on one thing, “it is UNCERTAIN and there will be many ways of doing things”.Now for someone who is highly paid for their predictions this seems like a great way of hedging your bets. He also highlighted the worrying change in society with the dominance of screen delivered information and a sedentary lifestyle. Previously children would have been told “behave or you will have to go inside!”, now it is the opposite! He described a world where devices know more about you than you do about yourself. Anybody who says they know exactly what the future holds is lying. However, we spend too much time worrying about it. We NEED to spend time as communities figuring out what we want to happen, using a proactive and positive mindset. It doesn’t matter if we are wrong. We must all have a collective vision of where we want to go, build narratives around the vision and step towards it. I agree with Richards aim of… “Every day waking up and trying to get better, making things better for ourselves and others” Another interesting person is Yuval Noah Harari: 21 Lessons for 21stcentury - interview Professor Megan Reitz: Professor of Leadership and Dialogue Speaking Truth to Power – Have a look for yourself here– it was an excellent 60 mins. Megan delivered a fantastic session about “That moment!” The one a person decides, shall I say something or not, and educated us on the act of “Speaking up”. All the scandals in healthcare organisations of recent times have something in common. People knew bad stuff was going on, but they didn’t speak up, and this resulted in patients coming to harm. One reason is the belief that it is always someone else’s responsibility and absolving oneself from responsibility. “They” aren’t speaking up, “they” need to show courage. Another issue is that often those very people who say the one time they did build up the courage and spoke out, they weren’t listened to and it made no difference. What if you experimented, what difference would it make at a collective level? Think about an occasion where you decided to say something, or not. Megan uses T.R.U.T.H to discuss the issues about these decisions. TRUTH: Trust, Risk, Understanding, Titles, How-to Trust: The value of your own opinion Risk: Realizing the risks of speaking up to powerful people and the ensuing struggle Understanding: Will I be perceived negatively, will I upset someone,“Will I belong”? Titles: We label inherently. Depending on the context, convey levels of authority How-to: Knowing what to say, when, how and to whom Megan then describes a number of traps and behaviours we all fall into which stop us from having the conversations we know we should have! Speak-Up Traps: We doubt ourselves – Imposter syndrome. Check the voice, notice when it comes in. Engage with it, am I going to listen to it this time. The Blind Spot: You will not listen unless you trust the value of their opinions. Can I empathise with how risky it might feel for this person to be speaking up? What titles do I have on me to affect what kind of information this person is telling me? Individuals ALWAYS think they are better at listening than other people. Listen-up traps: It’s easy to forget that no matter how lovely and approachable we seem as juniors, decades later, given some labels and titles, we are all quite scary. Make sure you don’t send“Shut up” signals and not “speak up” signals by knowing your face (and the rest of your body language signals, and environment you create). Today and every day, we make choices about what to say and when to stay silent. When we really help someone else to speak up or silence them. Choices feel mundane but if you add them up together it is what defines you. How you speak up and listen up represents the values you hold and the culture in which you work. If you think about it and act accordingly, you will change habits and change cultures. Some exercises and information to peruse at home in your own time! Exercise 1: Personal Values Think about your own values! What matters to you? How do you display your values at work? Much of the conflict at work results from a mis-alignment of core values. Spend some time writing down your beliefs. What behaviours demonstrate your values? None of these have anything to do with medicine or your background/grade. Exercise: Search for 50 personal values on the internet. Step 1: Make 3 groups of importance to you (High, Medium, Low) Step 2: Place each of the 50 values in a group Step 3: Take the “High” group and again split these into high, medium and low. Step 4: Group similar values together until you have 3-5 left. Step 5: Welcome to your values, enjoy them, be true to them, live them! Check out…Harry Kramer, Values in Leadership. One moves around the grid, depending on what is being demanded of us. Who else is there? Personal circumstances? Ideally there is a sweet spot (in Green) of moving around all areas, aiming to avoid the inept/donkey. How do you bring people and landscape together in your head and put it onto paper? Stakeholder mapping, mind mapping, network mapping. Another tool: Understanding people landscape map(Like Nike said… just do it) Length of the line: how far they are away from you Arrow direction: if you want them to be closer or further from you Dotted lines: are relationships you want to develop Small circles: /10 effort to build relationship (realistically) Stops: how far you want to bring them closer Wordsadd a narrative: Rich picture without words doesn’t show much Update it regularly, do it for different work groups. Use it for work networks, family situations, family events. For example, see diagram below: Do you know the 9 protected characteristics in the UK workplace? Age, Disability, Gender Reassignment, Marriage and Civil Partnership, Pregnancy and Maternity, Race, Religion or Belief, Sex, Sexual Orientation. A reflective exercise to do at the end of any teaching session, activity or experience. Take for example this blog (which I’ll admit has a lot crammed into it). Try and think of at least one behaviour in each of the following headings... Start doing: something you don’t do but think you should actively work to do more of. Stop doing: something you currently do but will actively try to do less of or stop doing. Continue doing:Something you are doing already but will do more of it because it works. Assim Ali Javaid – ST3 Paediatric trainees in Wales are a lucky bunch in many ways but one of my personal favourites is the chance to spend your ST3 year as an academic year. As far as I know, Wales Deanery is the only one that offers this option. Everywhere else you’re either on an official Academic Training Fellow Programme or not. Wales Deanery has been running the Academic ST3 Year option for the last 3 years and it offers paediatric trainees in Wales a chance to explore interests in research and/or teaching before formally entering Level 2 training. This is done alongside providing out of hours clinical cover at the University Hospital of Wales (UHW), usually as the Specialty SHO on call. There is only one Academic ST3 post available per year and it is largely up to the trainee who gets the post how they use the year. As such, every trainee who has had the post for the last 3 years has had a different experience.
In my case, I have an interest in research and teaching and wanted to explore something related to Paediatric Emergency Medicine. After discussing options with various consultants, I decided to join Professor Alison Kemp’s team and explore burns injuries in children from a safeguarding perspective. Alongside this I have offered to cover a clinical trial being carried out by the UHW Research Unit, taken up multiple teaching opportunities and started a Postgraduate Certificate in Medical Education. With all this on my plate, my day-to-day work varies greatly and I don’t have a typical “day” of work. In order to give you an idea of what I’ve done with this year I’ll briefly mention the different roles I’ve taken on. It’s worth remembering though, that this is a very flexible year and there are a number of other ways to use the time. The bulk of my work is based in research. The burns team I work with has a database of around 4,000 burns cases with huge amounts of usable data recorded for each case. After deciding on a couple of research questions with Professor Kemp, most of my time is spent reading through the relevant literature, working with the database and trying to answer it. Proposing and answering research questions uses an entirely different set of skills to managing patients on the ward and one of the main advantages to this year is getting a chance to exercise a set of cognitive functions we rarely get to use in clinical practice. For those unfamiliar with statistical analysis, as I was, this can be pretty daunting at first but as you have no in-hours clinical commitments, there is plenty of time to learn how to work with biostatistics. This would essentially be all I did during the day if I hadn’t chosen to take up a number of extra activities to break the monotony of research. During most weeks I will have two to four half day sessions dedicated to doing some of this extra work. I provide clinical cover for a trial being carried out at the Research Unit in UHW, for which my job is writing prescriptions, doing blood tests, interpreting ECGs and assessing any children who become acutely unwell while participating in the trial. Alongside this I spend a lot of time teaching. There are numerous teaching opportunities with UHW or Cardiff University and, I should point out, all are available for anyone to help with. However, the advantages of being an Academic Trainee is that, first, you have the time available to do a lot of teaching and, secondly, you’re often one of the first trainees to come to mind when Consultants or registrars are looking for help with teaching. So far this year I’ve been involved with teaching clinical skills to medical students, facilitating ethical debates between medical students, providing teaching to medical students on paediatric emergencies and paediatric prescribing, helping with mock paediatric exams for medical students at UHW, being a clinical tutor to final year students doing a module in Patient Safety, doing paediatric simulation training with final year medical students and providing teaching sessions for paediatric trainees due to sit their MRCPCH written or clinical exams. There are considerable out of hour’s responsibilities too. The Academic ST3 usually goes on to the Specialty SHO on call rota, which is 50% banded at present, providing out of hours cover for Surgery, Neurology, Cardiology, Respiratory, Renal and Oncology. However, another great advantage to being an ST3 at UHW is the option to step up and cover your on call shifts as the Registrar instead. UHW is a nice place to do this as you’ll be paired with registrar covering General Paediatrics (usually more senior than yourself) and there’s an onsite PICU registrar for help also. Of course stepping up to Registrar is entirely optional and the post is based on the assumption of SHO level cover. If you’re considering applying for the Academic post for ST3 there is only one place available per year, so it can be competitive. In order to qualify, the applicant has to be on course to have completed their membership exams, i.e. all the written papers and the clinical exam, by the end of ST2. If that’s the case, what you need to consider is whether this is what you’d like to do with your ST3 year. Trainees who aren’t particularly interested in research or teaching, those who want to get as much SHO level clinical experience before entering Level 2 training or those who want to skip ST3 altogether and go straight to ST4 probably have little to gain from spending their ST3 year on an Academic post. It’s also not particularly great for those who want to gain early experience in a particular sub-specialty in UHW, with a possible future SPIN or Grid application in mind. However, this is a fantastic post for anyone with an interest in research and/or teaching, for those looking to improve their CV for a future Grid application or those who just want a bit of a break from constant clinical practice. It’s a rare chance to experience something outside of clinical practice, without having to take time out of the programme in order to accomplish it. Personally, I can’t recommend the Academic post highly enough! An OOPE in Sydney, Australia. Dr Thomas Cromarty I have just returned from an OOPE and wanted to share my experience of living and working in Australia. After embarking on the best training scheme of them all (Paediatrics) in 2012, I worked around South Wales from ST1-5. The Welsh Paediatric Training Programme Director is keen to produce well rounded paediatricians and encouraged me take the opportunity in Westmead Children’s Emergency Department, Sydney. I could tell you about all the trips we went on: Visiting my dad in Canberra, Campervanning around Tasmania, watching the tennis in Melbourne, taking selfies with the quokkas on Rottnest island (Perth), surfing in Margaret River, watching the Commonwealth Games in the Gold Coast, swimming with turtles on the Great Barrier Reef and night treks in the Daintree rainforest. But that will just make you jealous and me sad, so I’ll try and give you unbiased view of my reflections on a year working there instead. “Big surf” in the Australian Life Saving Ironman @ Queenscliff Life Saving Club Nat and I with the Rottnest star of the show aka “The Quokka” It would make a mockery of a blog if I didn’t start by mentioning the Work:Life balance situation! My partner and I lived 500m the beach in a place called Queenscliff near Manly. Our end of the beach was quiet, had waves most of the time and was pretty much perfect. We lived on the top floor of an apartment block which included a roof top terrace aka skin cancer zone. As an “outdoorsy type” I was in heaven. There were running, cycling and triathlon clubs, surfing beaches, SUP, yoga studios, open water swimming and even Dragon Boat racing! You name it, it was expensive, but it was available. Unfortunately, I worked 40km away in the west of the city which meant that I had my old friend, traffic, to contend with on a regular basis. I worked 4 x 10 hour shifts per week in the Paeds ED, with most shifts mirroring the peak attendance times of 14:00-00:00. Despite the commute, there was no chance of me moving to other side of the world and not living by the Ocean! The Work: Positives
Dr Smarty Pants, hard at work… at Westmead Children’s Hospital The Work: Negatives
I produced a PDP of goals to achieve throughout the year, these included upgrading my USS skills as well as confidence managing paediatric trauma and minor injuries. I found this particularly useful and would encourage everyone to take some time to establish some short, medium, and long term goals for life both in and outside of work. I think it is essential for all medical staff to experience working in a number of different settings. This enables them to be exposed to a number of working environments and behaviours, choosing which to adopt into their personal style, facilitating their journey to becoming a more effective clinician and leader. My year working abroad will undoubtedly be different to yours and you need to decide if it is right for you (and your significant others!) What I would say though is if you don’t try it, you’ll never know… What’s the worst that could happen?! The start of “Hells Bells” 24 hour adventure race in Noosa, Queensland Helicopter trip over Sydney CBD Fair Dinkum, I had a ripper of a year out and am looking to continue that growth of skills this year as a Clinical Leadership Fellow in Cardiff and Vale, engaging junior doctors in leadership and QI development. If you want to get involved with this project, have any questions about taking a year out or just want to see some more photos please don’t hesitate to contact me at [email protected]. Favourite phrases:
Patient’s parent: She’s been crook for days mate? Doctor: Nah no worries mate, she’ll be right! Guest blog from Dr Nicole Parish, Clinical Psychologist, Noah’s Ark Hospital for Wales We’re led to believe that multitasking is a good thing. That tackling several activities in one go, while thinking of many more, is a highly regarded skill essential to our professional and personal lives. But could there be advantages of not planning the next activity while you’re still doing your last; of not checking your phone while eating lunch; or of not mentally replaying things from your day while watching TV? What if instead there was a drive to do one thing at one time? Well, that’s the concept of mindfulness: to actively focus your attention on one thing in the present moment and to do it in an accepting, non-judgmental way. I am Nicole, a Clinical Psychologist working within the Children’s Hospital for Wales and I am keen to promote the idea of mindfulness for staff well-being. As an outsider, I can see how a career in medicine could take its toll: the multiple demands, the irregular shift patterns and dealing with difficult situations on a daily basis. I feel it is important to do all we can to change the inevitably flawed systems in which we work in and, until then, support staff to manage it. Rather than just expecting them to cope. Thank you to Lisa Budd for her photograph from California Our working lives can make our already busy minds even more frantic. We’ll go over things that have happened; thinking about how things could have or should have gone. Equally, we daydream about what’s to come; practicing conversations in our head or imagining the worst case scenario. In recognising this, mindfulness first asks us to slow down the mental chitter chatter. To notice when your mind is going off on a tangent and to bring it back to the here-and-now. Then there’s the judgments we make. The continual and automatic criticisms we have about anything and everything. That sound is irritating, that person is really frustrating or I’m so stupid I shouldn’t have done that! This is why the second concept of mindfulness asks us to be open to all experiences in a non-judgmentally. Imagine two people are caught in a downpour of rain. One is furious, wishing they’d checked the weather forecast and worrying that they’ll get a cold. Whereas the other notices the pressure of the rain droplets on their shoulders and the feeling of cold water on their hands. Both of them will get just as wet, but their emotional experiences of the storm are going to be very different. Having said that, mindfulness isn’t a miracle cure that’s going to make all your stress disappear. But focusing on only one thing may help you to feel more settled, even if just for a moment. Perhaps doing less at once could help you to tackle more? And taking the time to tune into how you are feeling may motivate you to make beneficial changes. At work you’re expected to wash your hands between seeing patients, and perhaps there is a way to think about refreshing you mind in a similar way? Thank you to Lisa Budd for her photograph from California If you’re interested in finding out more, the books ‘Mindfulness: Finding peace in a frantic world’ by Mark Williams and Danny Penman, and ‘Wherever You Go, There You Are’ by Jon Kabat-Zinn are a good place to start. Plus many health boards in Wales offer mindfulness initiatives for staff. For example, I deliver drop-in mindfulness sessions every fortnight within Cardiff and Vale UHB. There are also free courses lead by Academi Wales, such as ‘An Introduction to Mindfulness’ and their 3-day retreat style ‘Explore and Walk’, which I can say first hand is brilliant.Want to start smaller? You can make tweaks to your routine to be more mindful, the trick is finding something that works for you. My sister, for example, is a fan of listening to an app on her phone for about 5-10 minutes a day (well, on the days she remembers and that’s fine!). If you’d like the structure of a guided meditation, and could benefit from taking yourself away for a short period of time, some good ones to try are Headspace (free to download, with an optional subscription), Buddhify (initial fee for the app, then free to use) and Smiling Mind (free to download and free to use). Whereas I prefer to build the ideas of mindfulness into what I am already doing. I use my walk home as an opportunity to focus on the scene around me, the colour of the trees and the movement of my feet. If that’s more up your street, try choosing one thing to do with more intent and curiosity. When brushing your teeth, notice the sensation of the bristles and taste of the toothpaste; when washing up, pay attention to the temperature of the water and the squeaky sound of the sponge; or perhaps sit down to really enjoy that cup of tea, rather than picking up your mug to take a sip only to find you’ve drunk it all!
So instead of multitasking, maybe it is time to try focusing your attention on just one thing? Purposefully and non-judgmentally. You won’t do it perfectly and you will get distracted. But that’s ok. Mindfulness isn’t about getting it right, it’s all about noticing, accepting and refocusing, many times over. “The little things? The little moments? They aren’t little.” – Jon Kabat-Zinn Rebecca Broomfield Maximising impact 13th-15th November, Southport Theatre and Convention Centre Once again I was privileged to attend the Association for Simulated Practice in Healthcare annual conference. The train journey to get here was epic but the conference was def. worth the travelling. The conference started with a Tuesday Evening Keynote after a day of workshops. An inspiring first session from Professor Tim Draycott. He spoke about simulation giving teams a chance to 'Have another go'. Team training and teams who train together the communicate well and share leadership. But he demonstrated many examples where teams training together did not improve outcomes. So therefore what is it about a team which makes them more effective? Professor Draycott suggested that teams who did this stated the emergency earlier, the amount of directed commands was higher and they communicated using an SBAR model (Situation, Background, Assessment, Recommendation) In teams that were training together but not seeing improvement in their outcomes he suggests looking further and ensuring that the equipment used is appropriate and that the simulations are standardised, like a recipe. He asks whether as we move forward we should be looking at simulation and evaluating it as we do pharmacological drugs - can we make it a qualy? This would engage and influence the policy makers. Could we offer insurance discounts to hospitals who regularly participate in team simulation and show that this has increased patient safety. We need to give simulation a value. He also suggested that simulation could be use to understand problems and help make the right way the easiest way. Therefore identifying ways which the system needs to change by running simulations. It is more than just knowledge transfer. Day 2 Day 2 began with one of the most inspiration speakers I have seen at a conference. Dr Kimberley Stone From Seattle Children's hospital spoke about using simulation to test out the design of a new children's hospital. They got the designers to mock up a card board version of areas such as the research room in the emergency department and the kitchen so they could run through how the rooms flowed and worked. When they found significant flaws in the design of the resus room they were able to redesign it and make it fit how they wanted it to work, all using simulation. Once the bricks were laid and the hospital was ready to open the simulated 'a day in the life of …. ward' before a patient stepped foot in the door. They were able to identify latent threats and patient safety issues and correct them without any chance for patients to come to harm. This offered me a completely different view of simulation and one which I had not thought of using simulation for but when you look at it, it makes complete sense. If we can do practise runs in the hospital before it's built we ensure that equipment is where we need it to be and patient flow is optimised. If we then SIM each area before it is used we can identify all the latent threats and eliminate them before they become close to making it into patient care. This use for simulation looks fantastic and in the future this should become the norm. Breakout sessions then commenced with a variety of talks on exciting projects which are happening around the country. I was particularly interested in Doreen Stockdale's presentation on running a 'Dragons Den' type competition for midwifery students to design an app which introduces the students to simulation teaching and how it works. It is often forgotten when you have been doing simulation for a while that to others it is an alien teaching form and they don't know how to do it. The app is in the process of being made and has 3 area's - Know yourself, know others and Get to know the story. I'm looking forward to seeing it finished and whether we could use it with our undergraduate students or nursing colleagues as an introduction to simulation. The next keynote was delivered by Professor Nick Sevdalis He spoke about moving simulation from looking at Efficacy (can I work?) to Effectiveness (Does it work?) Looking a scaling up simulation training programs and how we can make it work. Followed by more breakout sessions. The most interesting session I attended focused on developing non technical skills recognition for junior doctors through simulation teaching. This involved designing a 'Bingo' type card for simulation observers to focus on different human factors while the simulation session was going on rather than be passive observers. This helps in developing the knowledge of the junior doctors in human factors. The final keynote speaker on day 2 was Paul Gowen's who is the Lead consultant paramedic for the Scottish Ambulance service. He demonstrated the fantastic work which the Scottish Ambulance service has been doing for out of hospital cardiac arrests and was a very dynamic speaker, I would recommend watching his talk on catch up for a reminder about why we are all focusing on simulation to improve patient outcomes. After a meeting of the Paediatric special interest group was done it was onto the conference dinner. Photo's of this will not be shared but I loved the addition of a mini conference photo booth! Day 3 Day 3 started with 2 keynote speeches. The first delivered by Dr Neil Ralph @DrNRalph from Health Education England who shared the notion that we should be investing in the people who deliver the simualtions and focusing more on faculty development as well as working with e-LfH to offer e-learning around simulation. Followed by Professor Bob Stone who tooke the whole room into a world of virtual reality being utilised in the armed forces and how this can be applied to healthcare. He focused very much on 'Humans first, technology second' Mixed reality in healthcare is not yet fit for purpose but its developing fast and new opportunities are emerging. plus the simulation for evacuation of casualties on the helicopter looked absolutely fantastic. His keynote offered us a taste of what is yet to come, and it could make simulation even more exciting. I presented in the next breakout session the falls project detailed below. After lunch their were further breakout sessions to see what everybody else was doing within simulation around the country and learn about the introduction to the STEP program which ASPiH has developed to aid with the development of simulation technicians. The closing keynote was delivered by Bryn Baxendale. Who spoke about the development of health teams. I was lucky enough to get the opportunity to present some of the work we have been doing in Cardiff and Vale within the medical education team in simulation. Within Cardiff and Vale we have reorganised the way we have been creating and structuring our simulation courses. We have been making these more mutli-disciplinary and therefore focusing on team work within the NHS. We know that increasing team work increases productivity and improves patient safety. We have also been evaluating our simulation more effectively and have been able to show statistically significant increases in confidence and knowledge following attendance at a simulation course. We are creating simulation courses around significant targets for the trust such as the reduction of falls. I was lucky to present orally a project we did with the Trauma and Orthopaedic department. We created a patient story simulation from admission to post theatre in order to improve the confidence of the Foundation Doctors with patient management. This has been a very successful course which significantly improved the confidence of the trainees who have been through it. The second oral presentation I gave was on the Falls project. We are keen to develop simulation around significant patient safety issues and falls prevention and management has been highlighted as one of these. We have been working with a ward in our hospital and lead nurses have been trained in teaching simulation and are now delivering it to their teams. Again this project has been very successful. The two poster presentations are below and focus on a further 2 simulation course which are available. I was grateful to get the opportunity to present the fantastic work we have been doing in Cardiff and Vale to a wide audience. In summary, if you have any interest in simulation I would absolutely recommend that you put the ASPiH conference in you diary to attend, next year is in Belfast. The keynote speeches from this year can be found at: https://www.youtube.com/playlist?list=PLzm6Ad9XIwxksSlhE9BK4IQY2kOpKvxUJ Thank you to the ASPiH team for giving me the opportunity to present our work and to Cardiff and Vale for enabling me to attend this fantastic conference which has given me lots of exciting ideas. For more information:
Last years blog can be found here: https://www.wrenpaediatrics.com/blog/its-all-about-simulation ASPiH website: http://aspih.org.uk/ Follow on twitter: @ASPiHUK Conference website: http://www.aspihconference.co.uk/ |
Editors
Dr Annabel Greenwood Categories
All
|









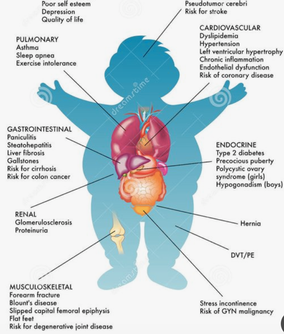
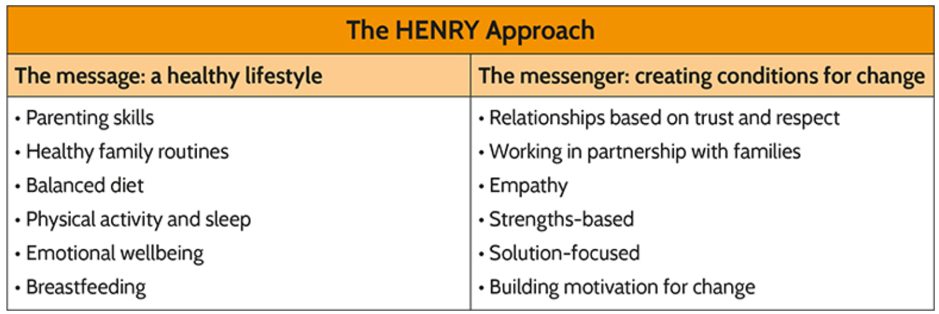

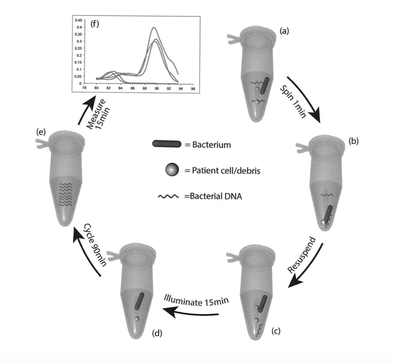




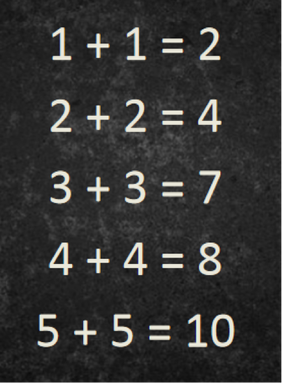


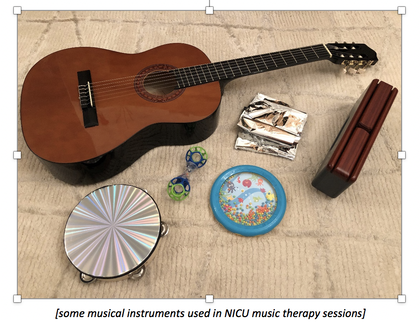
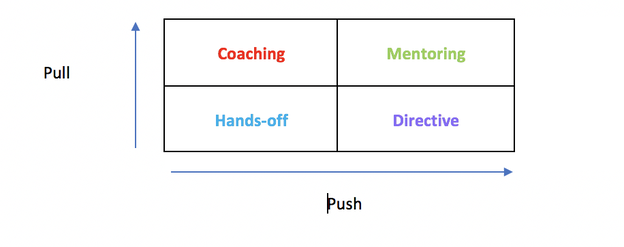
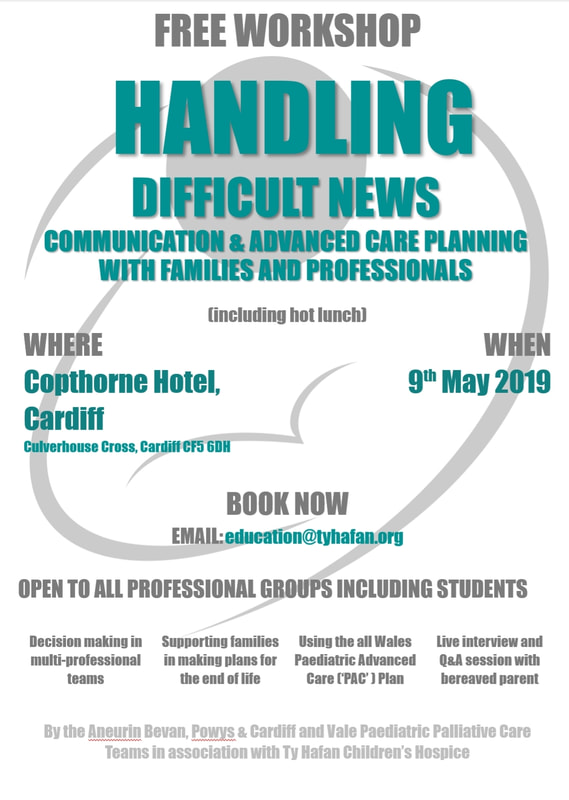







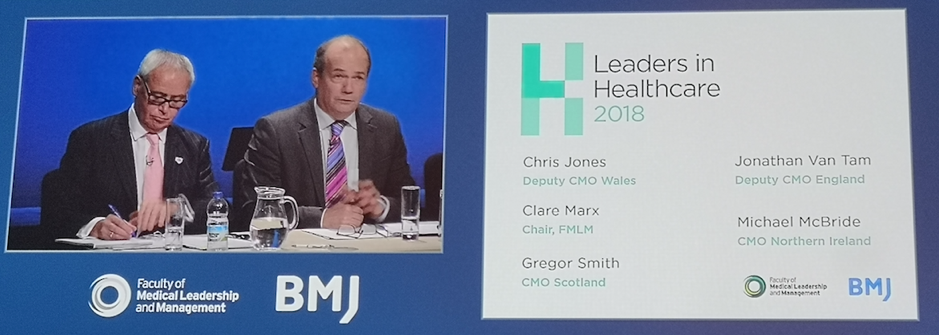
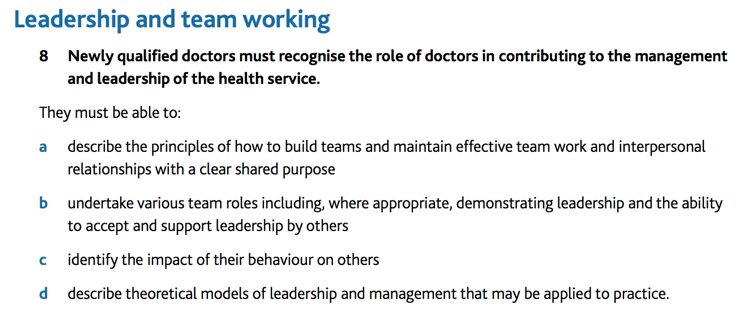
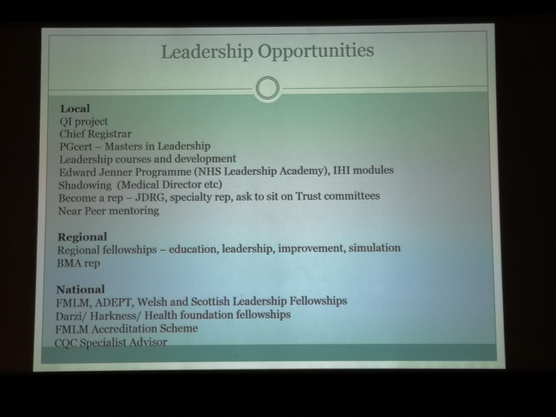
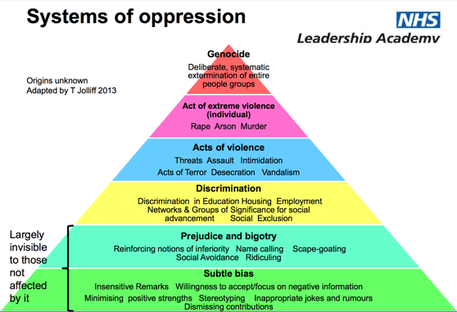
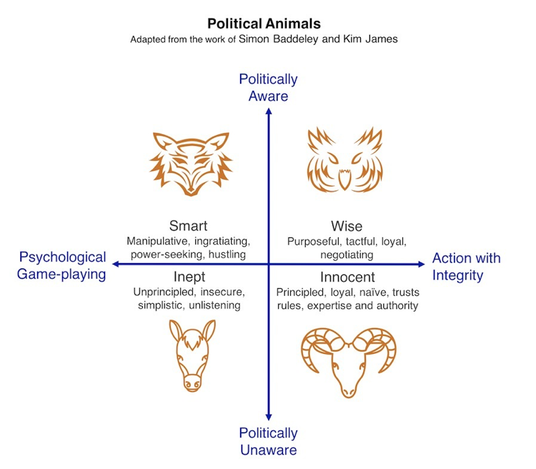
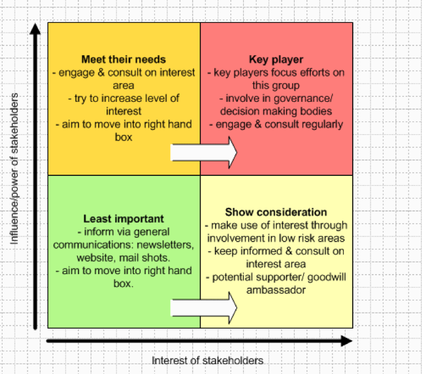
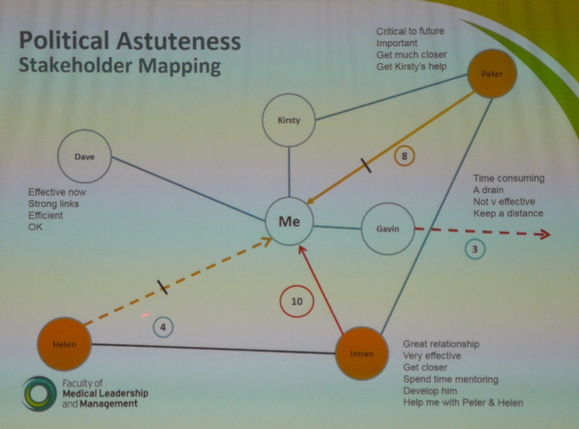










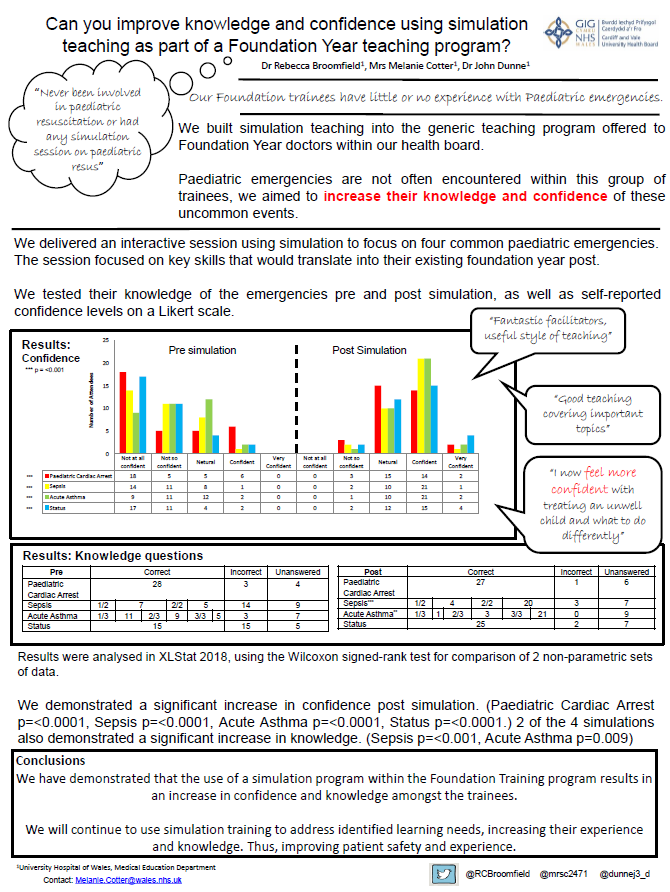
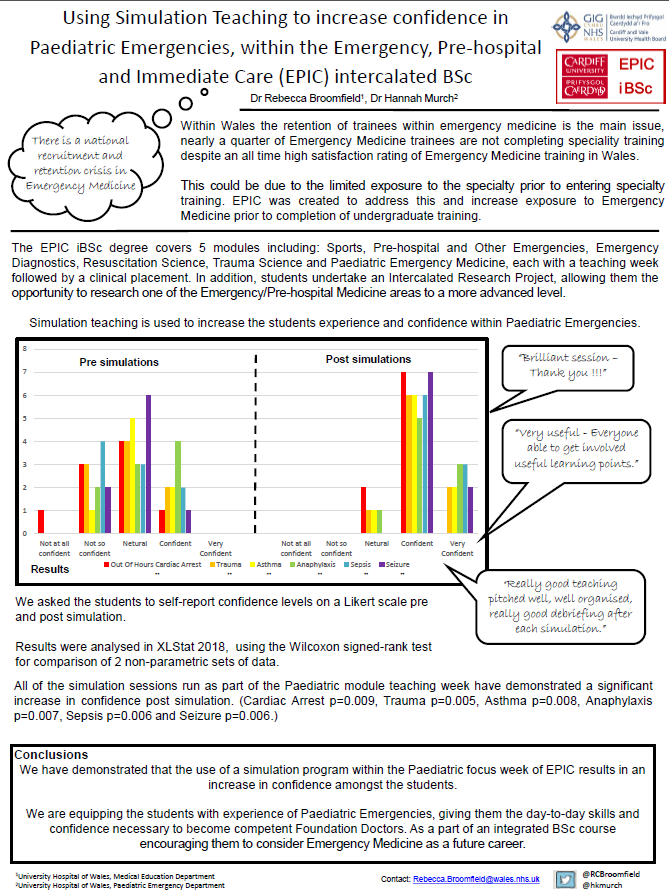
 RSS Feed
RSS Feed
